In a world that is increasingly technological and interconnected, but also more violent, overexploited and polluted, Paediatric Environmental Health (PEH) is one of the best contributions to improve global health. Few areas of the planet have a high affinity with common values and interests, such as the European Union (EU), Latin America and the Caribbean (LAC). The investments and actions of the PEH in pre- and postnatal periods during the first two decades of life will generate countless benefits in the health and well-being during the human life span. Detecting, reducing, or eliminating physical, chemical, biological and social pollutants is one of the main missions and actions of the PEH. In this special article, an update review is presented on the threats, challenges and cooperation opportunities in PEH among bio-health professionals and other social sectors involved, from the EU and LAC. New professional profiles, knowledge structures and architectures for engagement emerge. Courageous leaderships, new substantial resources, broad social changes, and the necessary collaboration between the two regions will be required to improve the health of present and future generations.
En un mundo cada vez más tecnológico e interconectado, pero también más violento, esquilmado y contaminado, la salud medioambiental pediátrica (SMAP) constituye una de las mejores contribuciones para mejorar la salud global. Pocas zonas del planeta tienen una afinidad tan alta en valores e intereses como la Unión Europea (UE), América Latina y el Caribe (ALC). Las inversiones y actuaciones de la SMAP en periodos pre y posnatales durante las dos primeras décadas de vida generarán incontables beneficios en la salud y en el bienestar general en todas las épocas posteriores de la vida. Detectar, disminuir o eliminar los contaminantes físicos, químicos, biológicos y sociales es una de las principales misiones y acciones de la SMAP. En este artículo especial describimos, actualizamos y divulgamos las amenazas, los desafíos y las oportunidades de cooperación en la SMAP entre los profesionales biosanitarios y restantes sectores sociales implicados de la UE y de ALC. Surgen nuevos perfiles profesionales, estructuras de conocimiento y arquitecturas para el compromiso. Se requerirán liderazgos valientes, nuevos recursos sustanciales, amplios cambios sociales y la necesaria colaboración entre ambas regiones para mejorar la salud de las generaciones presentes y futuras.
Scientific development has achieved indisputable improvements worldwide in health care indicators, with a decrease in child mortality and increased control of child and adolescent diseases. On the whole, this has resulted in progressive increases in wellbeing and life expectancy. Between 1990 and 2016, the worldwide mortality rate in the under-five population decreased from 93 to 41 deaths per 1000 live births, and to less than 20 in the Latin America and the Caribbean (LAC) region and less than 10 in the European Union (EU).1,2
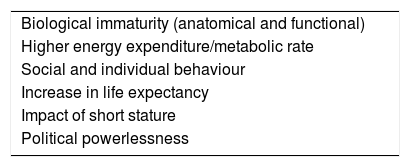
But these benefits have not come without a cost in the form of ecosystem degradation and pollution, which have in turn brought along increases in the incidence of environmental diseases. Pollution and the diseases associated with it affect countries at every level of development. Children are particularly vulnerable to the adverse effects of pollution (Table 1).3,4 In 1993, the World Health Organization (WHO) defined environmental health (EH) as comprising: (a) the aspects of human health, including quality of life, that are determined by physical, chemical, biological, social, and psychosocial factors in the environment, and (b) the theory and practice of assessing, correcting, controlling, and preventing those factors in the environment that can potentially affect adversely the health of present and future generations.5
The EU and LAC regions share similar values and are bound by historical, cultural and economic ties.6 The aim of our article is to present the threats, challenges and opportunities in paediatric environmental health (PEH) to paediatricians and biomedical professionals in the EU–LAC, and to propose useful pathways for different scenarios in child and adolescent health.
Threats to children's and adolescent's environmental healthAccording to the WHO, environmental factors contribute to 26% of annual deaths in the under-five population, amounting to approximately 1.5 million deaths worldwide, two thirds of which correspond to developing countries, and most of them related to respiratory or enteral diseases and air and water pollution.7
The main threats to PEH in these regions are7–16:
- •
Climate change. Significant global threat. It generates extreme weather events, heat waves, floods, food insecurity and an increase in disease. Eighty-eight percent of the morbidity and mortality related to climate change corresponds to the under-five population.8
- •
Air and soil pollution. Result from human activity, including polluting industries such as energy, paper, incineration and dumping of urban and industrial waste, active or abandoned mining areas, traffic and use of pesticides, herbicides and fertilisers. More than 90% of children breath polluted air.3,9
- •
Foods and malnutrition. Many foods are contaminated by organochlorine compounds, heavy metals, pesticides and chemicals used in the manufacturing, preparation and preservation of processed foods, which has an impact on child development. Malnutrition (obesity or undernutrition) also causes disease.7
- •
Safety of drinking water. Drinking water is a finite resource and accounts for less than 3.5% of all water bodies in the planet. Guaranteeing a sufficient supply of potable water is a population health quality indicator in the XXI century. Approximately 5% of the population in the EU–LAC do not have access to potable water.7
- •
Legal and illegal drugs. Exposure during prenatal life, childhood or adolescence. Approximately 25% of pregnant women in the EU and 11% in LAC consume alcohol,10 and this proportion can be as high as 70% in some regions.11 Consumption of alcohol, tobacco, cocaine or cannabis continues to grow among pregnant women and adolescents in some regions.
- •
Deforestation and desertification. Progressive deforestation is increasing desertification. These phenomena result from the excessive human exploitation of natural resources, the extraction of fossil fuels, the growth of multinational food corporations, socioeconomic factors and inadequate environmental policy. Natural disasters and infectious and parasitic diseases exacerbate the deleterious effects of climate change.12
- •
Sea and ocean health, impaired by acidification and raising temperatures. Oceans are biological and natural resources that generate employment, provide routes of transport and communication and regulate climate.13
- •
Lack of contact with nature. Children currently spend too much of their time indoors. Contact with nature and direct contact with other human beings are decreasing and being replaced by an expanding virtual reality, a trend associated with obesity, respiratory and cardiovascular diseases, behavioural problems, worsening of chronic diseases, vitamin D deficiency, sensory deficits and an increased exposure to carcinogens.14
- •
Poverty and environmental injustice.15,16 This is the leading paediatric environmental risk in the EU–LAC regions. Poverty is associated with greater pollution and poorer sanitation in domestic, work and community environments, with a higher presence of polluting industries and less healthy lifestyle habits. It creates conditions that promote child labour and sexual exploitation as well as clandestine adoption. It also contributes to the increase in migration in the EU and LAC. Insecurity, violence and armed conflicts hinder development and wellbeing in children and adolescents in different regions of the EU and LAC.
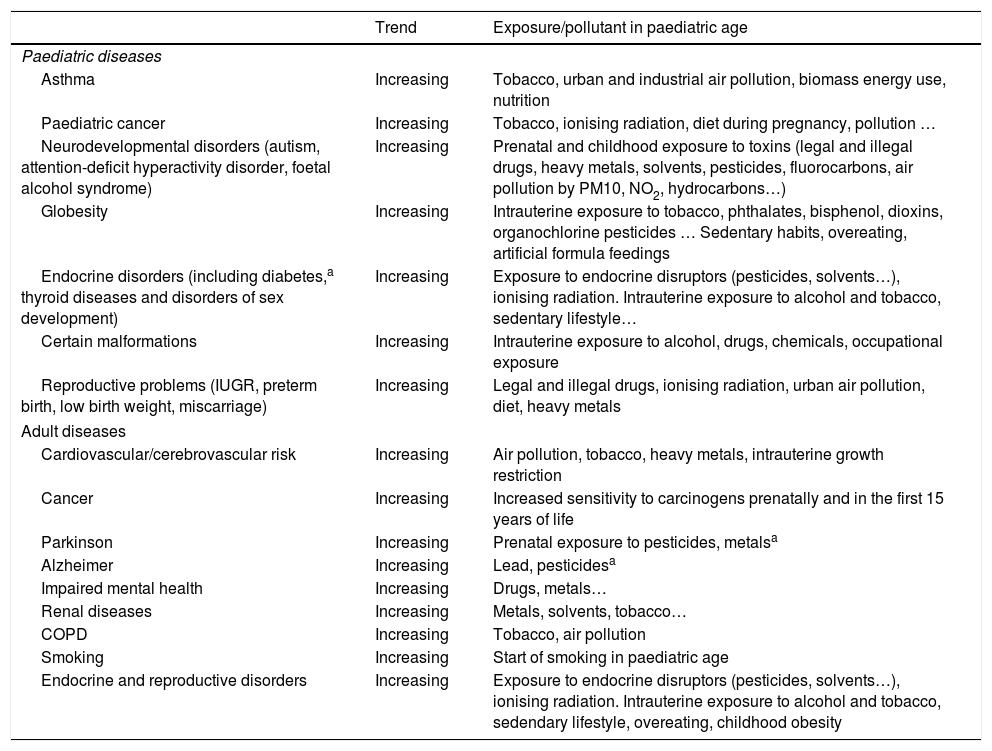
Children under five years of age account for 40% of cases of environment-related diseases.17 There are differences between countries based on income level, but there is an overall increasing trend in the incidence of paediatric and adult chronic diseases related to early exposure to environmental hazards (Table 2).
- a)
Respiratory diseases and asthma. Respiratory diseases are the leading cause of paediatric morbidity and mortality worldwide. They include acute and chronic diseases, most importantly those involving the lungs and bronchi, such as bronchopulmonary dysplasia, tuberculosis, congenital infections, asthma and cystic fibrosis.18 In children, these diseases and exposure to air pollution hinder lung development and predispose individuals to chronic obstructive pulmonary disease in adulthood.9,19Asthma is the most frequent chronic disease in the paediatric population, especially between ages 5 and 14 years.18 It has exhibited progressive increases worldwide, although its distribution varies widely between regions. Tobacco, the use of biomass energy, urban and industrial air pollution and malnutrition are some of the risk factors for acute and chronic respiratory disease.9,18
- b)
Childhood cancer. Since 1980, the overall age-standardised incidence rate of childhood cancers (age 0–14 years) has increased from 124 to 140 per million person-years. In South American, it has increased from 116 to 133 per million person-years, and in Western Europe, from 132 to 160 per million person-years. In the EU, the overall 5-year survival nears 80%, with 5-year survival nearing 100% in some types of cancer.20 The populations and economies in LAC are growing rapidly, with 26% of the overall population aged 15 years or less, and 24000 new cases of childhood cancer a year. Within the LAC region, survival rates are similar to those in the EU in Chile and Uruguay, while in other countries they do not even reach 40%.21
- c)
Endocrine disorders. In the EU, in the past century the age at menarche has decreased from 17 to 12 years, and in countries in LAC there has been a reduction in the age at onset of puberty in girls. Precocious puberty increases the risk of breast and ovarian cancer, cardiovascular disease, infertility, teen pregnancy and psychiatric disorders. There has been an increase in the incidence of urogenital malformations, poor sperm quality and testicular cancer.22The global prevalence of diabetes has doubled since 1980. An increase by 38% in the incidence of diabetes is expected in LAC by 2025 in association with increasing urbanisation, dietary changes, alcohol use and sedentary lifestyles. In recent decades, the annual incidence of type 1 diabetes has increased by nearly 3% in high-income countries. In the EU, type 1 diabetes in 10 times more frequent compared to LAC.23 Eliminating exposure to endocrine disruptors will be a challenge in the prevention of all these disorders.
- d)
Neurodevelopmental/psychiatric disorders. Exposure to neurotoxins during childhood or in critical periods of organogenesis or cellular development during prenatal or postnatal life may produce brain damage and cause neurologic changes. These effects may manifest during childhood or in adulthood, and in some cases be permanent.24The evidence on the association of early exposure to environmental toxins, such as air pollution or alcohol, with neurodevelopmental disorders continues to grow. In the paediatric population, there is a prevalence of intellectual disability of nearly 1%, of learning disorders of 5% to 10% and of attention deficit hyperactivity disorder of 6% to 17% (1% corresponding to autism); foetal alcohol spectrum disorders affect 1.7% of children in LAC and 3.7% of children in the EU.10
- e)
Malnutrition: globesity versus global hunger. The abuse of hypercaloric and high-protein diets results in the deaths of millions of consumers in high-income countries from diseases associated with globesity (cardiovascular and cerebrovascular diseases, diabetes or cancer), and obesity is a global pandemic in the EU-ALC. The increase in child globesity is a significant challenge in the EU–LAC. On the other hand, many poor countries are affected by undernutrition, as individuals are not given access to arable land to feed their families. Worldwide, approximately 41 million children aged 5 years and under are overweight or obese, while 540000 a year die from starvation.25 The Decade of Action on Nutrition initiative (2016–2025) seeks to redouble the efforts to free the world from malnutrition.
- f)
Parasitic and vector-borne diseases.7 Climate change, migration and globalisation are changing the prevalence and geographical distribution of these diseases in the EU-ALC. Their prevalence is greater in countries with deficient hygiene and sanitation systems.
Chronic diseases of childhood, adolescence and adulthood. Trends and association with exposure to specific environmental factors in the paediatric age period.
| Trend | Exposure/pollutant in paediatric age | |
|---|---|---|
| Paediatric diseases | ||
| Asthma | Increasing | Tobacco, urban and industrial air pollution, biomass energy use, nutrition |
| Paediatric cancer | Increasing | Tobacco, ionising radiation, diet during pregnancy, pollution … |
| Neurodevelopmental disorders (autism, attention-deficit hyperactivity disorder, foetal alcohol syndrome) | Increasing | Prenatal and childhood exposure to toxins (legal and illegal drugs, heavy metals, solvents, pesticides, fluorocarbons, air pollution by PM10, NO2, hydrocarbons…) |
| Globesity | Increasing | Intrauterine exposure to tobacco, phthalates, bisphenol, dioxins, organochlorine pesticides … Sedentary habits, overeating, artificial formula feedings |
| Endocrine disorders (including diabetes,a thyroid diseases and disorders of sex development) | Increasing | Exposure to endocrine disruptors (pesticides, solvents…), ionising radiation. Intrauterine exposure to alcohol and tobacco, sedentary lifestyle… |
| Certain malformations | Increasing | Intrauterine exposure to alcohol, drugs, chemicals, occupational exposure |
| Reproductive problems (IUGR, preterm birth, low birth weight, miscarriage) | Increasing | Legal and illegal drugs, ionising radiation, urban air pollution, diet, heavy metals |
| Adult diseases | ||
| Cardiovascular/cerebrovascular risk | Increasing | Air pollution, tobacco, heavy metals, intrauterine growth restriction |
| Cancer | Increasing | Increased sensitivity to carcinogens prenatally and in the first 15 years of life |
| Parkinson | Increasing | Prenatal exposure to pesticides, metalsa |
| Alzheimer | Increasing | Lead, pesticidesa |
| Impaired mental health | Increasing | Drugs, metals… |
| Renal diseases | Increasing | Metals, solvents, tobacco… |
| COPD | Increasing | Tobacco, air pollution |
| Smoking | Increasing | Start of smoking in paediatric age |
| Endocrine and reproductive disorders | Increasing | Exposure to endocrine disruptors (pesticides, solvents…), ionising radiation. Intrauterine exposure to alcohol and tobacco, sedendary lifestyle, overeating, childhood obesity |
In all nations, the health interventions with the highest economic and social returns are those that increase the resources allocated to pregnancy, childhood and adolescence.26 A good example is childhood vaccination.
The increases in health care costs associated with the treatment of chronic diseases provide an excellent opportunity to develop health economics models based on the prevention of diseases and environmental hazards.
All children, wherever they live, are affected by environmental hazards. However, rightful access to effective diagnostic tests and treatment, technology and psychosocial care varies widely and is a source of injustice worldwide. Poverty and race are key determinants of environmental injustice and threats to paediatric health.16
Inequities in childhood are associated with the costs of economic productivity and chronic disease in adults.27 Environmental degradation and vulnerable policies contribute to the persistence of these inequities in health.16
Natural resource depletionIncreases in population and human activity and the abuse of natural resources lead to the overexploitation of the planet, with an associated decline in biodiversity and the overall sustainability of life on Earth. According to the Global Footprint Network,28 the greatest ecological footprints correspond to the EU, Brazil, Chile and Argentina. In LAC there has been a dramatic 89% decrease in biodiversity relative to 1970. Twenty percent of the Amazon rain forest has been lost in only 50 years. It would take 1.7 planets Earth to produce all resources currently used by the global population sustainably.
Ageing and urban development29Between 2000 and 2050, the proportion of the global population aged 60 or more years will increase from 11% to 22%. At present, this age subset amounts to 24% of the total population in the EU and 11% of the total population in LAC. The declines in birth rates and increases in life expectancy are key factors in the global population ageing, although international migration flows have also contributed to changes in age distribution in regions of the EU and LAC.
In the next 15 years, the population aged 60 years and older will grow by 71% in LAC and by 23% in the EU. The ageing index of the population (the ratio of individuals aged >60 years over those aged <15 years) in LAC was 0.44 in 2015 and is expected to rise to 1.53 by 2050, exceeding the ageing index predicted for Europe in 2075.29 The ageing of the population calls for action in the area of chronic diseases in every age group. Many chronic diseases of adulthood are subclinical during childhood. To improve the health of the ageing population, we need to optimise paediatric health, making prevention of environmental risk factors a priority among the competencies of paediatricians.
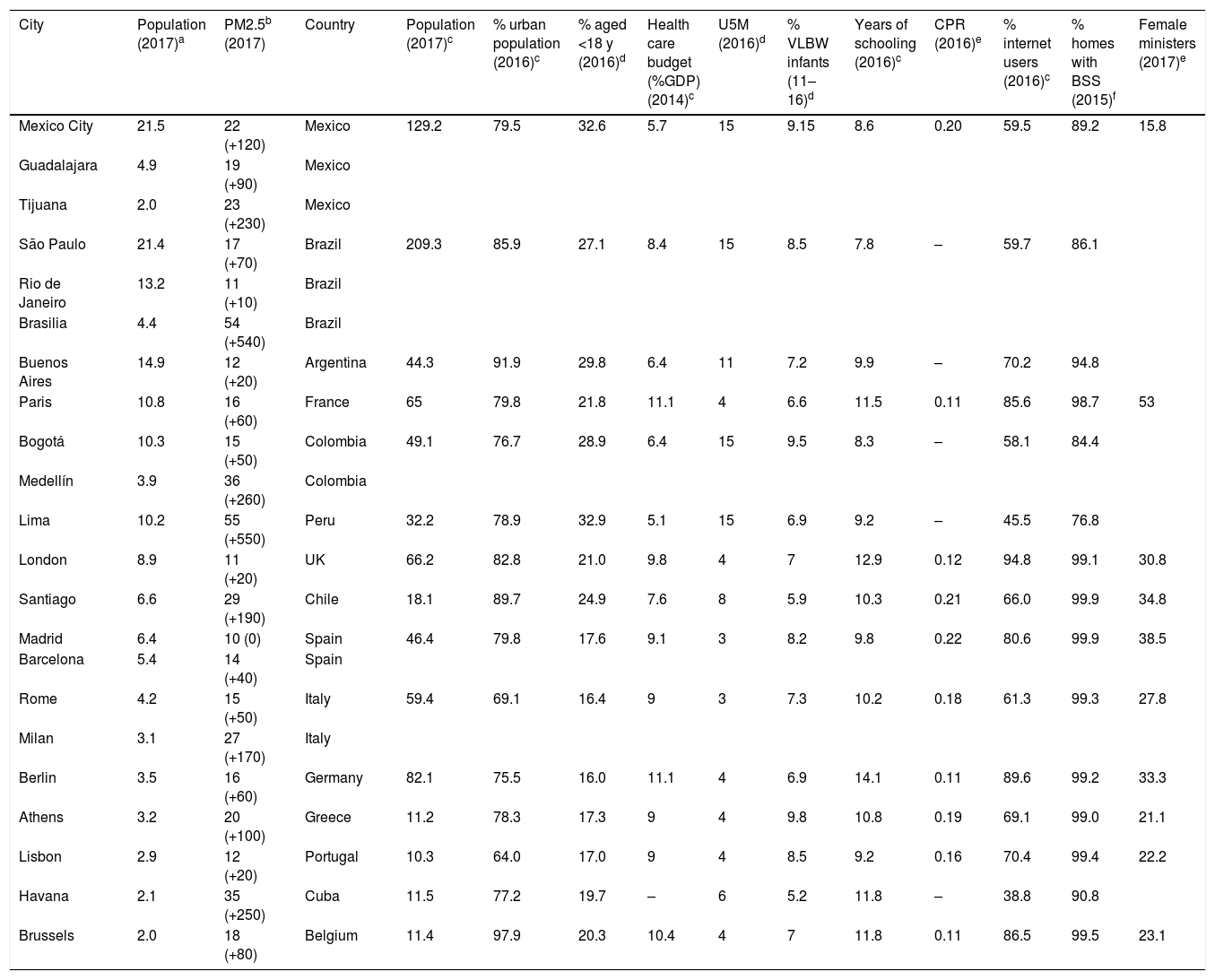
In 2015, 74% of the population of the EU and 80% of the population of LAC resided in cities, and 20% to 21% in suburban areas characterised by greater poverty and violence. Although in the last 2 decades the proportion of the population living in slums has decreased in LAC, in absolute terms the number has increased to 111 million.30Table 3 presents the most populous cities and data for some indicators.
Sociodemographic characteristics. Level of pollution in urban areas in the EU–LAC with populations of more than 2 million and additional nationwide indicators.
| City | Population (2017)a | PM2.5b (2017) | Country | Population (2017)c | % urban population (2016)c | % aged <18 y (2016)d | Health care budget (%GDP) (2014)c | U5M (2016)d | % VLBW infants (11–16)d | Years of schooling (2016)c | CPR (2016)e | % internet users (2016)c | % homes with BSS (2015)f | Female ministers (2017)e |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mexico City | 21.5 | 22 (+120) | Mexico | 129.2 | 79.5 | 32.6 | 5.7 | 15 | 9.15 | 8.6 | 0.20 | 59.5 | 89.2 | 15.8 |
| Guadalajara | 4.9 | 19 (+90) | Mexico | |||||||||||
| Tijuana | 2.0 | 23 (+230) | Mexico | |||||||||||
| São Paulo | 21.4 | 17 (+70) | Brazil | 209.3 | 85.9 | 27.1 | 8.4 | 15 | 8.5 | 7.8 | – | 59.7 | 86.1 | |
| Rio de Janeiro | 13.2 | 11 (+10) | Brazil | |||||||||||
| Brasilia | 4.4 | 54 (+540) | Brazil | |||||||||||
| Buenos Aires | 14.9 | 12 (+20) | Argentina | 44.3 | 91.9 | 29.8 | 6.4 | 11 | 7.2 | 9.9 | – | 70.2 | 94.8 | |
| Paris | 10.8 | 16 (+60) | France | 65 | 79.8 | 21.8 | 11.1 | 4 | 6.6 | 11.5 | 0.11 | 85.6 | 98.7 | 53 |
| Bogotá | 10.3 | 15 (+50) | Colombia | 49.1 | 76.7 | 28.9 | 6.4 | 15 | 9.5 | 8.3 | – | 58.1 | 84.4 | |
| Medellín | 3.9 | 36 (+260) | Colombia | |||||||||||
| Lima | 10.2 | 55 (+550) | Peru | 32.2 | 78.9 | 32.9 | 5.1 | 15 | 6.9 | 9.2 | – | 45.5 | 76.8 | |
| London | 8.9 | 11 (+20) | UK | 66.2 | 82.8 | 21.0 | 9.8 | 4 | 7 | 12.9 | 0.12 | 94.8 | 99.1 | 30.8 |
| Santiago | 6.6 | 29 (+190) | Chile | 18.1 | 89.7 | 24.9 | 7.6 | 8 | 5.9 | 10.3 | 0.21 | 66.0 | 99.9 | 34.8 |
| Madrid | 6.4 | 10 (0) | Spain | 46.4 | 79.8 | 17.6 | 9.1 | 3 | 8.2 | 9.8 | 0.22 | 80.6 | 99.9 | 38.5 |
| Barcelona | 5.4 | 14 (+40) | Spain | |||||||||||
| Rome | 4.2 | 15 (+50) | Italy | 59.4 | 69.1 | 16.4 | 9 | 3 | 7.3 | 10.2 | 0.18 | 61.3 | 99.3 | 27.8 |
| Milan | 3.1 | 27 (+170) | Italy | |||||||||||
| Berlin | 3.5 | 16 (+60) | Germany | 82.1 | 75.5 | 16.0 | 11.1 | 4 | 6.9 | 14.1 | 0.11 | 89.6 | 99.2 | 33.3 |
| Athens | 3.2 | 20 (+100) | Greece | 11.2 | 78.3 | 17.3 | 9 | 4 | 9.8 | 10.8 | 0.19 | 69.1 | 99.0 | 21.1 |
| Lisbon | 2.9 | 12 (+20) | Portugal | 10.3 | 64.0 | 17.0 | 9 | 4 | 8.5 | 9.2 | 0.16 | 70.4 | 99.4 | 22.2 |
| Havana | 2.1 | 35 (+250) | Cuba | 11.5 | 77.2 | 19.7 | – | 6 | 5.2 | 11.8 | – | 38.8 | 90.8 | |
| Brussels | 2.0 | 18 (+80) | Belgium | 11.4 | 97.9 | 20.3 | 10.4 | 4 | 7 | 11.8 | 0.11 | 86.5 | 99.5 | 23.1 |
BSS, basic sanitation services; CPR, child poverty rate; GDP, gross domestic product; U5M, under-five mortality; VLBW, very low birth weight.
Annual mean concentration of particulate matter with a diameter of less than 2.5 microns (PM2.5, μg/m3) (% in excess of the upper threshold proposed by WHO, 10μg/m3), http://www.who.int/airpollution/data/cities/en/.
https://www1.compareyourcountry.org/inequality/en.
Under-five mortality rate: probability of dying between birth and exactly age 5 years, expressed per 1000 live births.
Low birth weight: percentage of children that weighed less than 2500 at birth.
Internet users: estimated number of internet users in the total population. The calculation includes individuals that accessed the internet from any type of device (including mobile phones) in the past 12 months.
Urban population: percent of the population residing in urban areas, defined according to the definition applied in the most recent nationwide population census.
Child poverty rate: proportion of the population aged less than 18 years living with a household income of less than 50% the national average. The household income is calculated as the income after taxes and transfers and adjusted for the number of members of the household.
The construct of the family varies significantly between countries and communities. Democracy and globalisation promote family health in low- and high-income countries. The integration of low-income countries in the global economy is associated with increases in education and household incomes, thus improving child health.31
The use of technology is changing how family and interpersonal relationships are conceived. The introduction of technology makes the lives of individuals easier, but also changes human relations and health with both positive and negative effects. Technology interferes with interpersonal relationships and has physical, behavioural and emotional repercussions.
Opportunities for paediatric environmental healthIncreasing social awarenessThe increasing awareness in society of the interrelationship of health and environment is the main drive to push for changes in global policies to give a greater priority to children.
In addition, populations are increasingly demanding democracy, participation and freedom in shaping the context of their lives, including improved environmental conditions. Paediatricians play a key role in the management of environmental diseases by identifying environmental risk factors in their patients, providing guidance about them to reduce exposure, researching these diseases and helping other professionals, parents and society develop skills for their prevention. Their participation is a must in any debate regarding PEH, as is their involvement in advocacy for policies or environmental practices that can contribute to the protection of paediatric health.32
The sensorisation of life33,34We are immersed in the digital age, with greater access to information and improved real-time communication capabilities planet-wide, which allows the integration of distant professionals to obtain local, regional and global data for the purpose of developing integral strategies.
The changing patterns of environmental health require a more creative approach and strategy. Emerging sensing and biomonitoring technologies will improve prevention, diagnosis and treatment while reducing the burden of chronic environmental diseases in the EU–LAC by reaching remote geographical areas. Furthermore, the sensoriszation of ecosystems, clinical biomonitoring and digital platforms will lead to efficient and innovative health care models. It will be key, however, to assess how this will transform the lives of children.
New professional profilesWe need new professionals adapted to a “child and environmental health” culture. The creation of advisory committees, structures and tools are important steps to promote science in the field of PEH.3 Many PEH-related visits involve healthy individuals concerned by environmental factors, but society in general seeks interlocutors to which to address emerging concerns. New health care investment and business models will develop based on prediction, prevention, personalisation and community participation. The integration of PEH in clinical practice will contribute to a shift by which 80% of paediatricians will act as health consultants by 2050.33,34
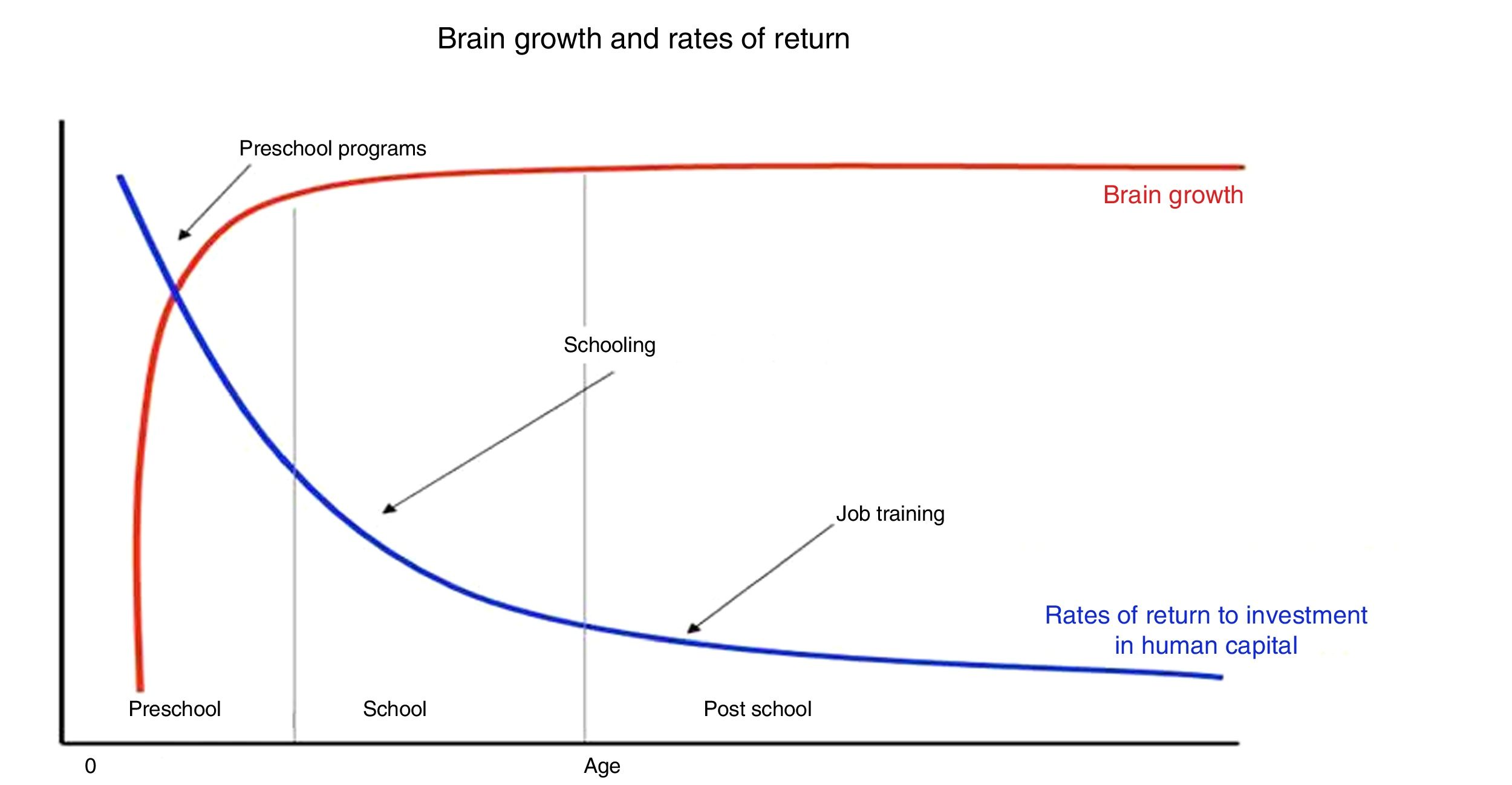
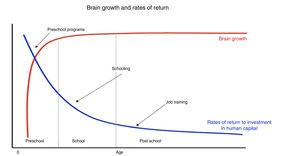
Plasticity and optimal child and adolescent development4,9,26Some types of childhood exposure are associated to chronic diseases in adulthood. Between 90% and 95% of the mass of the human brain develops starting in intrauterine life through age 5 years. The prenatal period and childhood and adolescence are critical periods of opportunity in the development of human neuroplasticity and cellular resilience to increase paediatric and adult wellbeing (Fig. 1).
The period with the highest economic returns of investment is pregnancy through age 5 years.
Source: Borrowed with the permission of Heckman & Carneiro Human Social Policy, 2003, RAND, Benefits and Costs of Early-Childhood Interventions, A Documented Briefing, Lynn A. Karoly, Susan S. Everingham, Jill Hoube, Rebecca Kilburn, C. Peter Rydell, Matthew Sanders, Peter W. Greenwood, April, 1997.
We need to create international networks and centres of excellence devoted to research in PEH involving professionals and institutions in the EU and LAC, such as the ENSUCHICA Network on “the environment, child cancer and child survival”. We also need to establish partnerships for the effective and direct exchange of information and research coordination with the aim of improving child health and reducing social disparities and pollution.3,35
Creation of paediatric environmental health unitsThe WHO and the EU have promoted the creation of paediatric environmental health speciality units (PEHSUs).32,36 These units, also known as children's environmental health units (CEHUs), are clinical units staffed by paediatricians and biomedical professionals with expertise in PEH in cooperation with other health professionals (obstetricians, toxicology specialists) and professionals in other fields (engineers, environmental workers, educators, psychologists, chemists …). Their purpose is to identify and assess environmental risks and diseases affecting the paediatric population, and to engage in education, training, research and school- and community-based health interventions. The PEHSU is a useful strategy in PEH to apply the precautionary principle in clinical practice. Networks of PEHSUs in the United States and Spain are helping launch similar initiatives in Mexico, Argentina and Uruguay.32,37
Clinical tools: the green page and the paediatric environmental history32,36The Green Page (GP) for EU–LAC is a tool designed in the context of health care policies delivered at the primary care level and consists of a basic screen for environmental factors that are relevant to paediatric health, to be accompanied by guidance and brief interventions in PEH. The GP includes basic questions regarding prenatal and postnatal life that explore different types of exposure: community-based (neighbourhoods and schools), domestic, related to parental occupation and related to lifestyle. There are different GP models, and they need to be adapted to each specific environment.
The GP is a useful tool in primary care. Its integration in check-up visits or prenatal or routine paediatric visits in the EU and LAC can identify risks associated to environmental pollution in pregnant women and children, increase the awareness and sensitivity of health care professionals and families in regard to environmental issues and improve prevention and quality of life at the community level. A GP form for pregnancy designed in the EU (including a mobile health version) is currently undergoing transcultural adaptation for its use in LAC.33,38
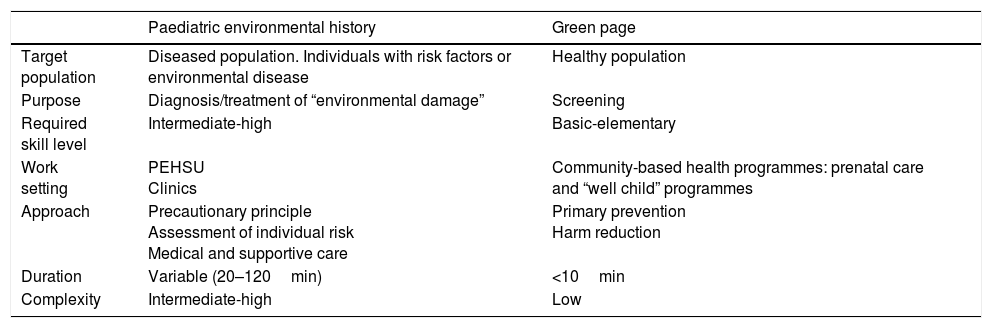
The paediatric environmental history (PEHi) is part of the standard health record. It comprises a series of questions to assess individual risk to identify environmental risk factors and prevent their effects. The role of PEHSUs in training paediatricians on the use of this tool is key. Table 4 summarises the differences between the GP and the PEHi.
Differences between the paediatric environmental history (PEHi) and the green page (GP).
| Paediatric environmental history | Green page | |
|---|---|---|
| Target population | Diseased population. Individuals with risk factors or environmental disease | Healthy population |
| Purpose | Diagnosis/treatment of “environmental damage” | Screening |
| Required skill level | Intermediate-high | Basic-elementary |
| Work setting | PEHSU Clinics | Community-based health programmes: prenatal care and “well child” programmes |
| Approach | Precautionary principle Assessment of individual risk Medical and supportive care | Primary prevention Harm reduction |
| Duration | Variable (20–120min) | <10min |
| Complexity | Intermediate-high | Low |
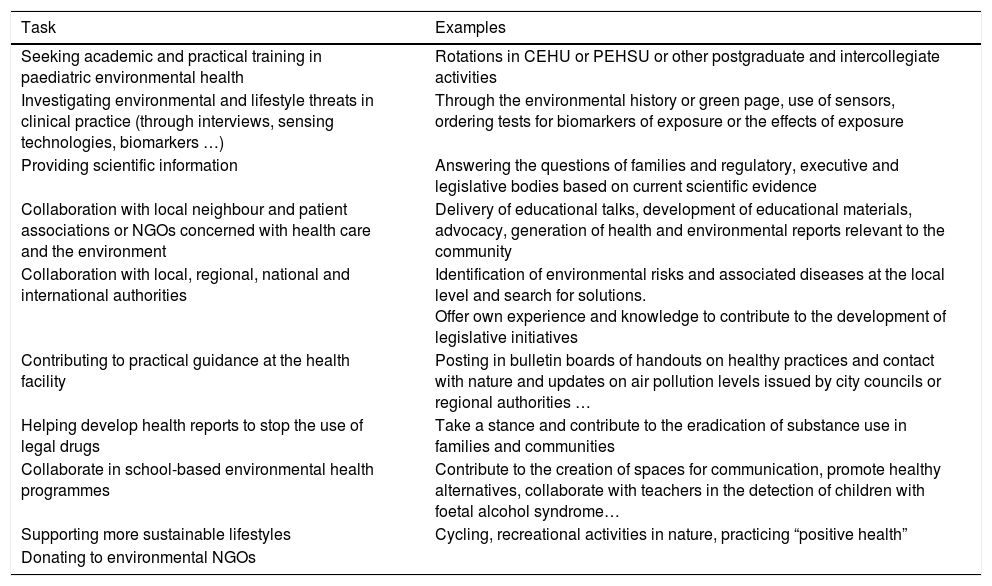
We need to advocate for the inclusion of environmental health items in the national budgets of the EU and LAC to fund and properly equip PEHSUs or CEHUs and to introduce PEH as a subject in the curricula of undergraduate and postgraduate degrees in health care and the biomedical sciences.36Table 5 proposes tasks through which paediatricians could become involved in PEH.
Tasks through which health care professionals may become involved in the promotion of child and adolescent environmental health.
| Task | Examples |
|---|---|
| Seeking academic and practical training in paediatric environmental health | Rotations in CEHU or PEHSU or other postgraduate and intercollegiate activities |
| Investigating environmental and lifestyle threats in clinical practice (through interviews, sensing technologies, biomarkers …) | Through the environmental history or green page, use of sensors, ordering tests for biomarkers of exposure or the effects of exposure |
| Providing scientific information | Answering the questions of families and regulatory, executive and legislative bodies based on current scientific evidence |
| Collaboration with local neighbour and patient associations or NGOs concerned with health care and the environment | Delivery of educational talks, development of educational materials, advocacy, generation of health and environmental reports relevant to the community |
| Collaboration with local, regional, national and international authorities | Identification of environmental risks and associated diseases at the local level and search for solutions. Offer own experience and knowledge to contribute to the development of legislative initiatives |
| Contributing to practical guidance at the health facility | Posting in bulletin boards of handouts on healthy practices and contact with nature and updates on air pollution levels issued by city councils or regional authorities … |
| Helping develop health reports to stop the use of legal drugs | Take a stance and contribute to the eradication of substance use in families and communities |
| Collaborate in school-based environmental health programmes | Contribute to the creation of spaces for communication, promote healthy alternatives, collaborate with teachers in the detection of children with foetal alcohol syndrome… |
| Supporting more sustainable lifestyles | Cycling, recreational activities in nature, practicing “positive health” |
| Donating to environmental NGOs |
We need to better educate resident physicians and nurses in training in the fields of paediatrics, obstetrics and family medicine in the integration of PEH in clinical practice.
Paediatrics societies will form committees on PEH32,39 to develop guidelines and programmes for training on specific competencies like the fellowship programmes in the United States.37
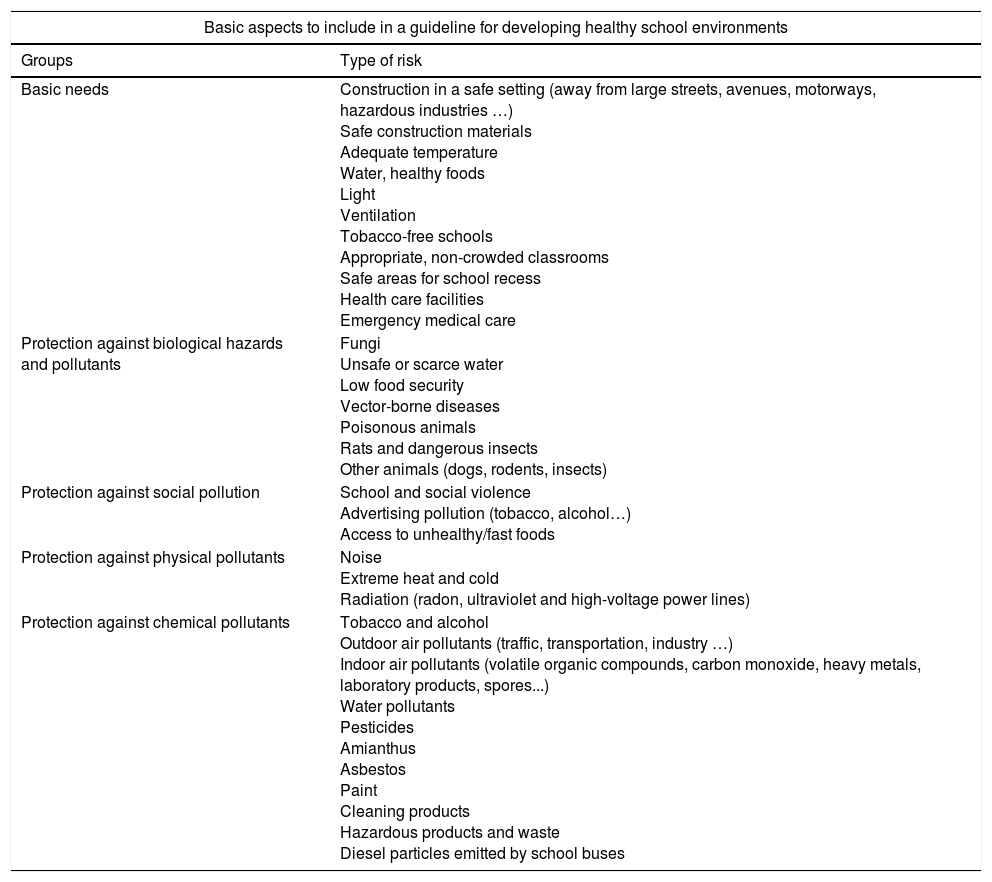
Development of healthy school environments40Children spend 40h a week in schools and child care centres. These settings raise concerns in parents regarding the exposure to pollutants. At the same time, fields concerned with education (education, teaching and learning) must take into account environmental pollutants (Table 6) and their adverse effects on health and natural ecosystems. The development of a guideline on school-based environmental health will help develop specific skills in school nurses.
Basic aspects of school-based environmental health.
| Basic aspects to include in a guideline for developing healthy school environments | |
|---|---|
| Groups | Type of risk |
| Basic needs | Construction in a safe setting (away from large streets, avenues, motorways, hazardous industries …) Safe construction materials Adequate temperature Water, healthy foods Light Ventilation Tobacco-free schools Appropriate, non-crowded classrooms Safe areas for school recess Health care facilities Emergency medical care |
| Protection against biological hazards and pollutants | Fungi Unsafe or scarce water Low food security Vector-borne diseases Poisonous animals Rats and dangerous insects Other animals (dogs, rodents, insects) |
| Protection against social pollution | School and social violence Advertising pollution (tobacco, alcohol…) Access to unhealthy/fast foods |
| Protection against physical pollutants | Noise Extreme heat and cold Radiation (radon, ultraviolet and high-voltage power lines) |
| Protection against chemical pollutants | Tobacco and alcohol Outdoor air pollutants (traffic, transportation, industry …) Indoor air pollutants (volatile organic compounds, carbon monoxide, heavy metals, laboratory products, spores...) Water pollutants Pesticides Amianthus Asbestos Paint Cleaning products Hazardous products and waste Diesel particles emitted by school buses |
Few regions in the planet have as high an affinity in values and interests as the EU and LAC. Improving PEH in the EU–LAC will require courageous leadership, new essential resources and significant social changes. Acknowledging both differences and common interests and promoting EU–LAC cooperation from the government, citizenry and the biomedical professions can have a powerful effect on improving PEH and reducing inequity, thus generating new opportunities.
FundingInternational Network Environment, Survival and Childhood Cancer (ENSUCHICA) in Europe and Latin America (FFIS EU17-01-01); Mount Sinai International Exchange Program for Minority Students; National Center on Minority Health and Health Disparities NIH (T37 MD001452); Fundación Séneca (MUR#19884-GERM-15); ICARUS (Horizon 2020: 690105); SaludAire-España (PI18CIII/00022); FIS 12/01416 and PI16CIII/00009.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Ortega-García JA, Tellerías L, Ferrís-Tortajada J, Boldo E, Campillo-López F, van den Hazel P, et al. Amenazas, desafíos y oportunidades para la salud medioambiental pediátrica en Europa, América Latina y el Caribe. An Pediatr (Barc). 2019;90:124.e1–124.e11.