The SARS-CoV-2 pandemic has had a great impact on the physical and psychological health of the population. The aim of this study was to evaluate child and adolescent mental health in a population cohort along the 2020–2021 school year.
MethodsThis was a prospective longitudinal study of a cohort of children from 5–14 years of age in Catalonia, Spain, performed from September 2020 to July 2021. The participants were randomly selected and accompanied by their primary care paediatrician. Evaluation of risk of psychopathology was performed using the Strengths and Difficulties Questionnaire (SDQ) carried out by one of the legal guardians of the child. We also collected sociodemographic and health variables of the participants and their nuclear family. Data were collected by an online survey through the RedCap platform at the beginning of the academic year and at the end of each trimester (4 cuts).
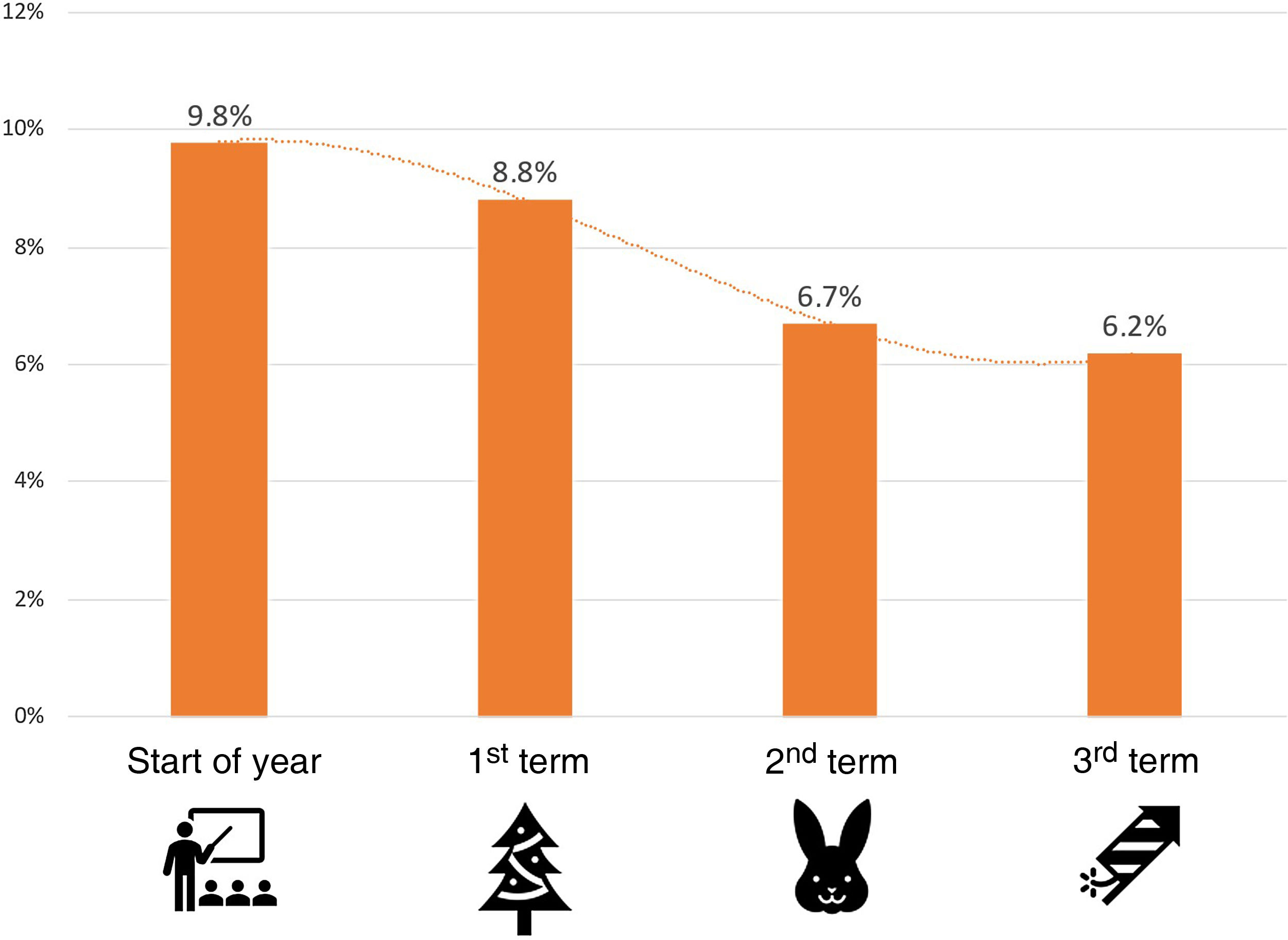
ResultsAt the beginning of the school year, 9.8% of the patients were probable cases of psychopathology compared to 6.2% at the end of the year. The perception of the level of preoccupation of the children for their health and that of their family was related to presenting psychopathology, especially at the beginning of the year, with the perception of a good family atmosphere being always related to lower risk. No variable related to COVID-19 was associated with an altered SDQ result.
ConclusionsAlong the 2020–2021 school year, the percentage of children with a probability of presenting psychopathology decreased from 9.8% to 6.2%.
La pandemia por SARS-CoV-2 ha tenido un alto impacto en la salud física y psicológica de la población. Nuestro objetivo fue evaluar la salud mental infanto-juvenil de una cohorte poblacional a lo largo del curso 2020-21.
Métodosestudio longitudinal y prospectivo de una cohorte de niños escolarizados entre 5 y 14 años en Cataluña entre septiembre 2020 y julio 2021. Los participantes fueron seleccionados de forma aleatoria y seguidos por el pediatra de referencia en la atención primaria. La evaluación del riesgo de psicopatología fue realizada a través del cuestionario Strengths and Difficulties Questionnaire (SDQ) contestada por un tutor legal del niño. Fueron recogidas también variables sociodemográficas y de salud del individuo y su núcleo de convivencia. Los datos fueron recogidos mediante una encuesta on line a través de la plataforma RedCap al inicio del curso y al final de cada trimestre (4 cortes).
ResultadosAl inicio del curso escolar el 9,8% de los pacientes fueron casos probables de psicopatología, frente al 6,2% de final de curso. La percepción del nivel de preocupación de los niños por su salud y la de su familia se relacionó con presentar psicopatología, especialmente al inicio del curso, mientras que la percepción de un buen ambiente familiar se relacionó en todo momento con menor riesgo. Ninguna variable relacionada con el COVID-19 se asoció con resultado alterado del SDQ.
ConclusionesA lo largo del curso escolar 2020-2021 el porcentaje de niños con probabilidad de presentar psicopatología mejoró y pasó del 9,8% al 6,2%.
The coronavirus 2019 (COVID-19) pandemic has been a public health crisis of global importance.1 The impact of acute infection by SARS-CoV-2 in the paediatric population has been low, as its course is generally mild.2,3 However, the changes the pandemic has imposed on the lives of children and adolescents (which we will refer to from this point as “children” for the sake of brevity) has brought their mental health into focus.4,5 One of the main changes has been the interruption of their schooling. It is estimated that up to 1500 million youth and children aged less than 20 years did not attend school during the first wave of the pandemic. According to an analysis by UNICEF,6 >13% of children aged 10–19 years had some form of mental health disorder in 2019. Early data on the impact of COVID-19 on mental health were first reported for the adult population7 and later for the paediatric population.8 These studies evinced a deterioration of mental health caused by the disease itself but also by the policy and public health measures adopted to contain transmission of the virus and respond to the pandemic.9 Other authors reported substantial increases in the prevalence of depression and anxiety in children.10,11
In Spain, the pandemic prompted the imposition of home confinement for nearly 3 months and the closure of schools for 6 months.12 Various domestic studies evinced an increased incidence of stress, anxiety and depression in adolescents.13 Many parents and caregivers (which we will refer to from this point as simply “parents”) noticed changes in their children’s mood and behaviour.14 A study conducted in our autonomous community, Catalonia, found an increased incidence of mood and behavioural symptoms in young children during the home confinement period.15 Some studies demonstrated that the impact was greater in socially vulnerable families.16 Certain authors proposed that the impact on mental health could persist or even increase with time,17 although there is scarce data from population-based and longitudinal studies18 on the mental health of children during the COVID-19 pandemic.
The aim of the study presented here, “Paediatrics and Mental Health” (PEDSAME), was to assess the mental health of the paediatric population and potentially associated factors at the population level and prospectively in the first school year of the COVID-19 pandemic.
Material and methodsStudy designWe conducted a prospective, longitudinal and observational study between September 2020 and July 2021 (2020–2021 school year). The study was conducted through the primary care paediatrics research network (XaRePAP) of the Section on Primary Care of the Societat Catalana de Pediatria (Catalonian Society of Paediatrics). This network includes primary care paediatricians and paediatric nurses with full representation of the Catalonian territory, including rural and urban areas.
ParticipantsEach participating paediatrician or nurse (Appendix B in Supplementary material) used a random number list to select a sample of 15 children from their caseloads. The sample consisted of children aged 5–14 years residing in Catalonia included in the caseloads of the participating providers. The exclusion criteria were lack of signed informed consent, inability to contact the patient by telephone and presence of a language barrier.
We estimated the necessary sample size based on the size of population aged 5–24 years in Catalonia (833 000, source: Statistical Institute of Catalonia [IDESCAT]).19 The expected prevalence of mental health disorders used as reference was 7.5%.19 We calculated the sample size required for a precision of 3% and a 95% level of confidence. The result was that the sample needed to include a minimum of 297 individual (calculation made with the Epidat software, version 3.1).
Data collectionOnce the sample was selected, we contacted one parent/legal tutor per child by telephone to invite them to participate in the study. A link was then provided via electronic mail through the RedCap platform20 to access all the necessary information about the study, sign the informed consent form and complete the online questionnaire (Appendix B in Supplementary material). For families without internet access, we offered the possibility of participating through an in-person interview.
We collected data at 4 timepoints during the school year: start of school year (September–October 2020), end of first term (December 2020–January 2021), end of second term (March–April 2021) and end of the school year (June–July 2021). At each time point, the parents completed the parent version of the Strengths and Difficulties Questionnaire (SDQ)21 in relation to the child at the present moment. They also answered different questions regarding the impact of the COVID-19 pandemic on the family and household, any psychological symptoms the child may have developed since the previous timepoint, any existing medical or psychiatric diagnoses in the child, and aspects related on sleep patterns, appetite, feelings, behaviour, worry and screen use (Appendix B in Supplementary material).
The SDQ is a validated instrument for assessment of the risk of psychiatric disorders in minors.21 It can detect emotional and behavioural problems in children aged 5–17 years. It is composed of 25 items grouped in 5 scales: emotional symptoms, conduct problems, peer relationship problems, hyperactivity/inattention and prosocial behaviour. We used the validated Spanish version of the SDQ,22 available at www.sdqinfo.com. To allow comparison with prepandemic results,19 we interpreted the results applying the same categories as the Department of Health of Catalonia: normal (0–13 points), possible case (14–16 points) and probable case (17–40 points).
Ethical considerationsThe study was developed in adherence with good clinical practice protocols. The PEDSAME was approved by the Ethics Committee of the Jordi Gol Institute of Primary Care Research (IDIAP) under code 20/142-PVC.
Statistical analysisWe performed a descriptive analysis of the sample data. We summarised quantitative data using the mean and compared them with the t-test. We summarised categorical data as percentages and compared them with the χ2 test. We considered differences statistically significant if the P value was less than 0.05.
The total SDQ score was calculated at each time point. For each timepoint, we compared the different variables under study in patients who were “probable cases” versus all other patients. We performed a multivariate analysis by means of binary logistic regression to determine which factors were associated with SDQ scores in the pathological range, including in the model those variables that remained significant at every timepoint of the follow-up.
The statistical analyses were performed with the software SPSS, version 25 (SPSS Inc, Chicago, IL, USA).
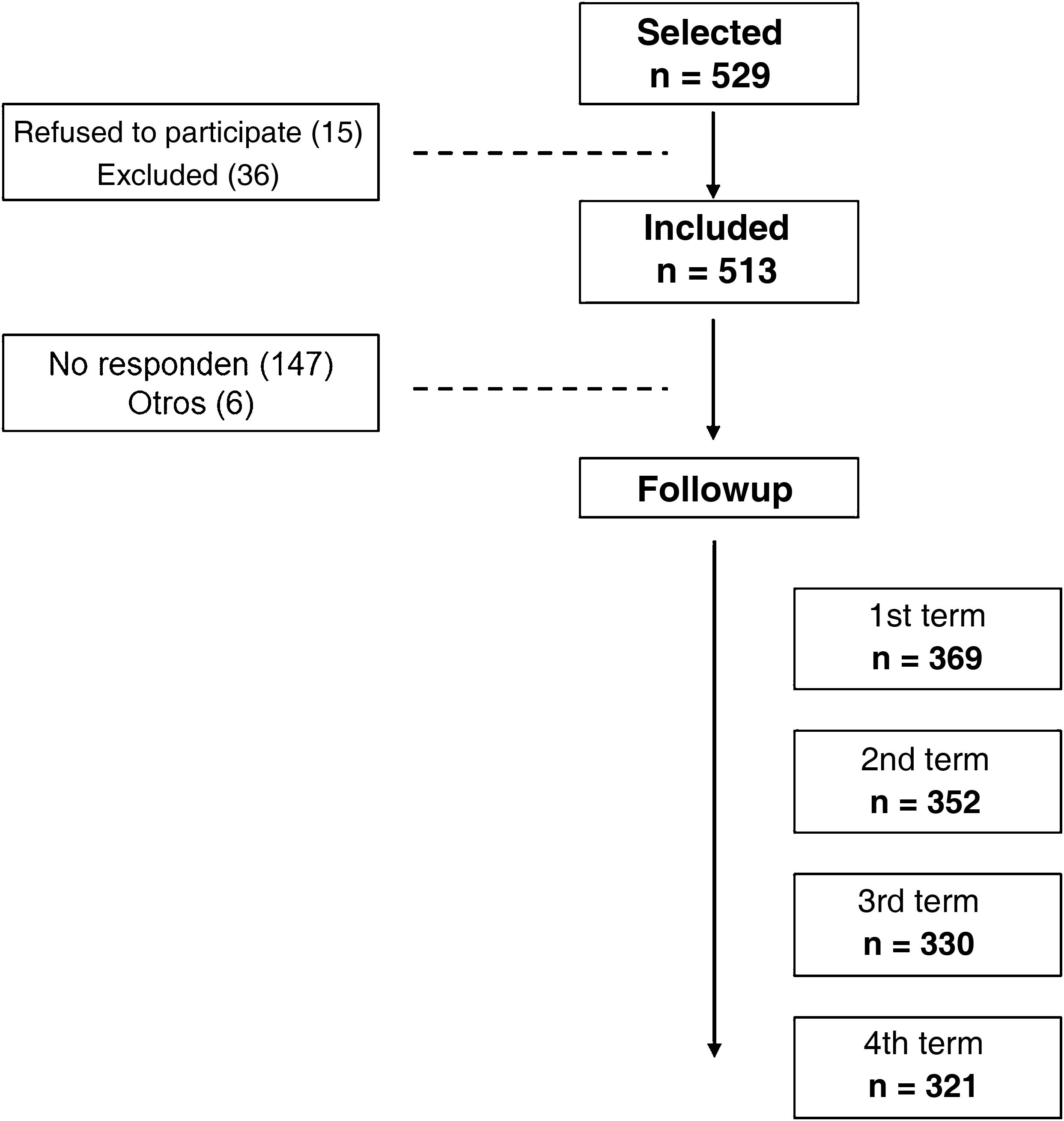
ResultsOf the 529 children selected at random, 369 were included in the analysis of the first timepoint (September 2020) and 321 in the analysis at the end of the study (July 2021) (13% lost to follow-up) (Fig. 1).
Descriptive analysis of the sampleTable 1 summarises the general characteristics of the sample; it is worth highlighting that 9.5% of the patients had a previous psychiatric or neurodevelopmental disorder diagnosis.
General characteristics of the sample.
| n = 369 | % | 95% CI | |
|---|---|---|---|
| Demographic characteristics | |||
| Female child | 195 | 52.8% | 47.6−58.1 |
| Mother was the participating parent | 319 | 86.4% | 82.8−90.1 |
| Parental nationality: Spanish | 304 | 82.4% | 78.4−86.4 |
| Child’s nationality: Spanish | 353 | 95.7% | 93.5−97.9 |
| Living with parents | 309 | 83.7% | 79.8−87.6 |
| Living in an apartment/flat | 243 | 65.9% | 60.9−70.8 |
| Home >90 m2 | 227 | 61.5% | 56.4−66.6 |
| Health-related characteristics | |||
| Absence of chronic disease | 352 | 95.4% | 93.1−97.7 |
| Parental history of mental health disorders | 14 | 3.8% | 1.7−5.9 |
| Previous diagnosis of psychiatric or neurodevelopmental disorder | 35 | 9.5% | 6.4−12.6 |
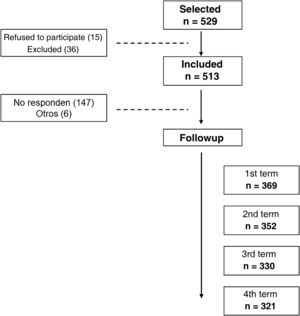
The primary outcome of the PEDSAME study was the SDQ score. At the beginning of the year, 9.8% of the patients were probable cases of a psychiatric disorder (while 11.1% were possible cases). The percentage of probable cases decreased gradually in the course of the school year, and was lowest in June 2021 with 6.2% probable cases (and 9.7% possible cases) (Fig. 2).
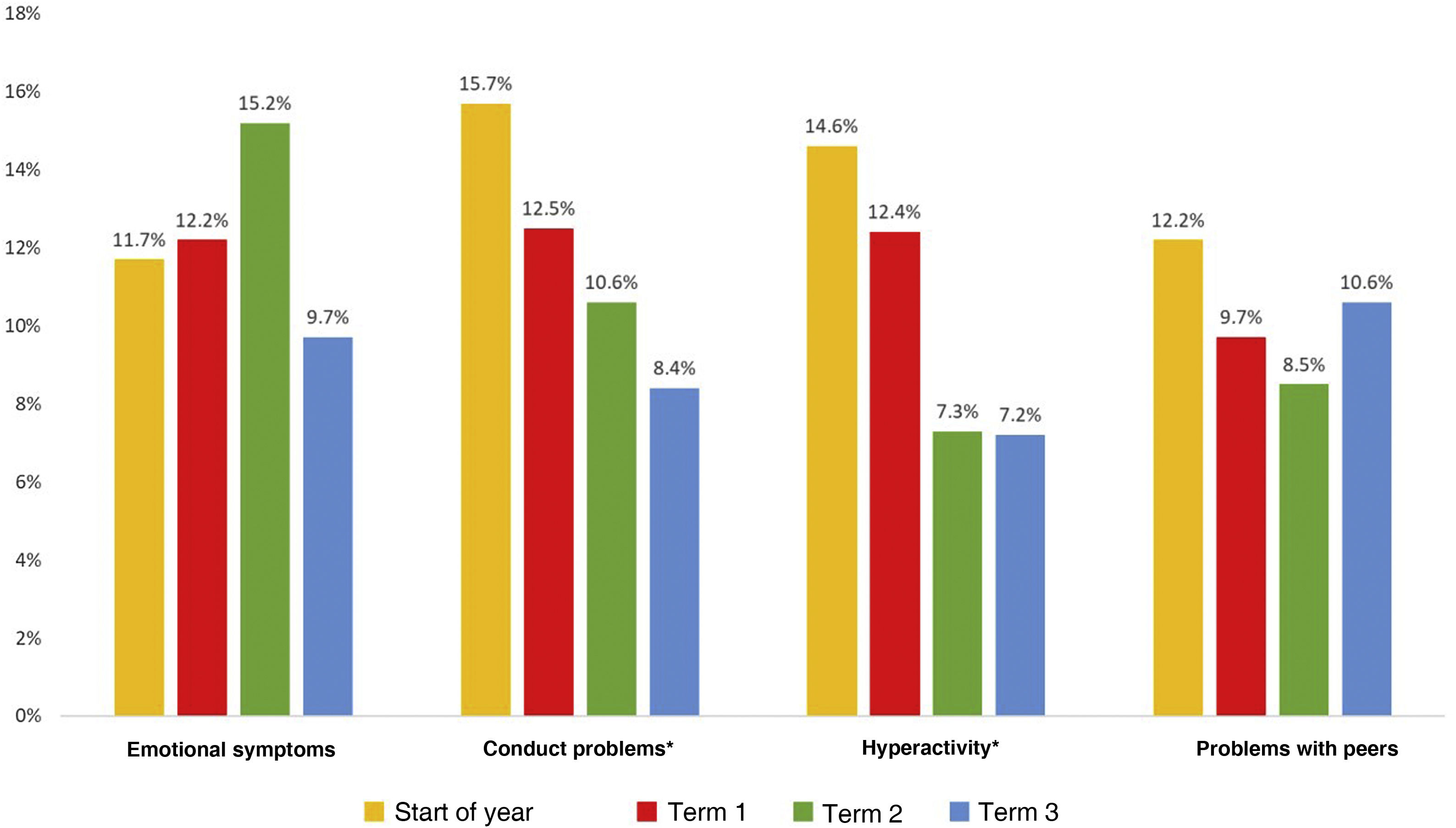
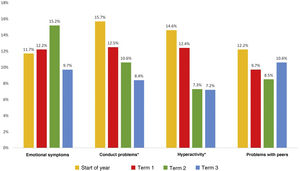
In the separate analysis of the SDQ scales (Fig. 3), conduct problems and hyperactivity/inattention exhibited clear improvement during the school year. These problems were significantly more prevalent in children aged 5–8 years in the first timepoint. Emotional symptoms were the most prevalent problem at the end of the second term, and problems with peer relationships were the most prevalent at the end of the school year.
Children with abnormal SDQ scores in September worried more than those with scores in the normal range. In the course of the year, this difference stopped being significant, while a positive perception of the home environment was associated with a normal SDQ score throughout the school year. None of the variables associated with the COVID-19 pandemic (confinement measures, disease in the child or a family member, hospital admissions or deaths) was associated with abnormal scores in the SDQ. On the other hand, a previous history of psychiatric illness was strongly associated with having an abnormal SDQ score throughout the follow-up. In the last 2 timepoints, scoring in the abnormal range was also significantly associated with the initiation of mental health care (Table 2).
Comparison of children with normal and abnormal SDQ scores and of the level of worry of the child and parents during the school year, the home environment, initiation of mental health care and a pre-existing psychiatric diagnosis.
| Variable | Category | Start of year(n = 369) | 1st term (n = 352) | 2nd term(n = 330) | 3rd term(n = 321) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Normal SDQ n (%a) | Abnormal SDQ n (%a) | Pb | Normal SDQ n (%a) | Abnormal SDQ n (%a) | Pb | Normal SDQ n (%a) | Abnormal SDQ n (%a) | Pb | Normal SDQ n (%a) | Abnormal SDQ n (%a) | Pb | ||
| Level of worry of child for own health | None/Mild | 193 (58%) | 11 (30.6%) | 0.000 | 158 (49.2%) | 10 (32.3%) | 0.118 | 168 (54.5%) | 7 (31.8%) | 0.116 | 194 (64.5%) | 10 (50.0%) | 0.402 |
| Moderate | 101 (30.3%) | 11 (30.6%) | 79 (24.6%) | 8 (25.8%) | 71 (23.1%) | 8 (36.4%) | 48 (15.9%) | 5 (25.0%) | |||||
| High/Very high | 39 (11.7%) | 14 (38.9%) | 84 (26.2%) | 13 (41.9%) | 69 (22.4%) | 7 (31.8%) | 59 (19.6%) | 5 (25.0%) | |||||
| Level of worry of child for family’s health | None/Mild | 92 (27.6%) | 5 (13.9%) | 0.203 | 65 (20.3%) | 5 (16.1%) | 0.412 | 77 (25.0%) | 4 (18.2%) | 0.617 | 129 (42.9%) | 7 (35.0%) | 0.237 |
| Moderate | 90 (27%) | 12 (33.3%) | 70 (21.9%) | 10 (32.3%) | 85 (27.6%) | 8 (36.4%) | 70 (23.3%) | 8 (40.0%) | |||||
| High/Very high | 151 (45.3%) | 19 (52.8%) | 186 (57.8%) | 16 (51.6%) | 146 (47.4%) | 10 (45.5%) | 102 (33.9%) | 5 (25.0%) | |||||
| Home environment | Very bad/Bad | 86 (25.8%) | 22 (61.1%) | <0.001 | 7 (2.2%) | 7 (22.6%) | <0.001 | 6 (2%) | 6 (27.3%) | <0.001 | 4 (1.3%) | 2 (10%) | <0.001 |
| Normal | – | – | 93 (29.9%) | 16 (51.6%) | 93 (30.2%) | 10 (45.5%) | 66 (22%) | 10 (50%) | |||||
| Good/Very good | 247 (74.2%) | 14 (38.9%) | 221 (68.8%) | 8 (25.8%) | 209 (67.9%) | 6 (27.3%) | 231 (76.7%) | 8 (40%) | |||||
| Initiation of mental health care | No | 316 | 30 | 0.060 | 306 (95.3%) | 27 (87.1%) | 0.075 | 293 (94.9%) | 13 (61.9%) | <0.001 | 286 (95%) | 15 (75%) | 0.005 |
| Yes | 17 | 6 | 15 (4.7%) | 4 (12.9%) | 16 (5.1%) | 8 (31.8%) | 15 (5%) | 5 (25%) | |||||
| Previous psychiatric diagnosis | No | 309 (92.8%) | 25 (69.4%) | 0.000 | 295 (91.8%) | 23 (74.2%) | 0.005 | 282 (91.5%) | 17 (77.3%) | 0.045 | 279 (92.6%) | 15 (75%) | 0.019 |
| Yes | 24 (7.2%) | 11 (30.6%) | 26 (8.2%) | 8 (25.8%) | 26 (8.5%) | 5 (22.7%) | 22 (7.4%) | 5 (25%) | |||||
We conducted a logistic regression analysis introducing in the model the 2 variables in which we found statistically significant differences between children with normal and abnormal SDQ scores in all 4 timepoints: the perception of the home environment and the having a pre-existing psychiatric diagnosis. Table 3 presents the corresponding odds ratios. A positive home environment was associated with normal scores in the SDQ throughout the school year, while having a pre-existing psychiatric diagnosis was associated with abnormal scores in the SDQ.
Multivariate analysis including variables with significant differences.
| Variable | Category | Start of year | 1st term | 2nd term | 3rd term |
|---|---|---|---|---|---|
| Perceived home environment | Very bad or bad | Reference | Reference | Reference | Reference |
| Normal | – | 0.12 (0.04−0.43) | 0.07 (0.02−0.28) | 0.24 (0.04−1.53) | |
| Good or very good | 0.46 (0.32−0.67) | 0.03 (0.01−0.10) | 0.02 (0.01−0.08) | 0.05 (0.01−0.35) | |
| Previous psychiatric diagnosis | Yes/No | 5.91 (2.47−14.16) | 4.32 (1.62−11.54) | 4.77 (1.50−15.23) | 5.17 (1.61−16.66) |
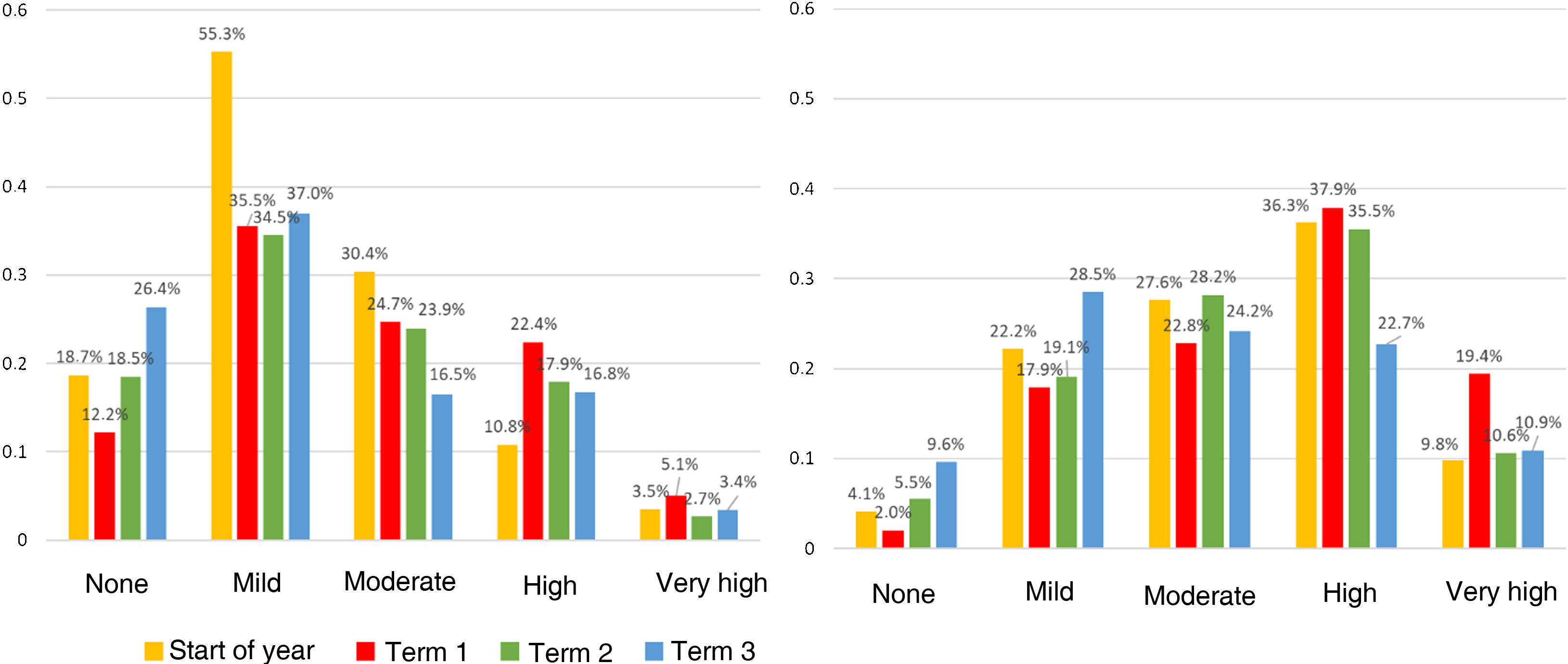
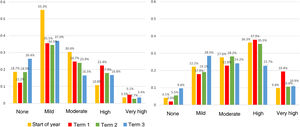
Table 4 presents the changes over the school year in the worry of children regarding their own health, the worry of parents regarding health in the family, the perception of the home environment, the impact of COVID-19 on the family and the potential impact on mental health. Children tended to worry less than their parents (Fig. 4). The level of worry of families and children about their health were greater in the first and second terms and had improved by the end of the third term. The percentage of families that perceived the home environment as very bad decreased significantly over time, and at the end of the year none reported a bad home environment.
Worry about health in children and parents, perception of home environment, impact of COVID-19 on the family and potential mental health effects.
| Variable | Category | Start of year n = 369 (%) | 1st term n = 352 (%) | 2nd term n = 330 (%) | 3rd term n = 321 (%) |
|---|---|---|---|---|---|
| Level of worry of child about own’s health | None | 69 (18.7%) | 43 (12.2%) | 61 (18.5%) | 85 (26.4%) |
| Mild | 135 (55.3%) | 125 (35.5%) | 114 (34.5%) | 118 (37.0%) | |
| Moderate | 112 (30.4%) | 87 (24.7%) | 79 (23.9%) | 53 (16.5%) | |
| High | 40 (10.8%) | 79(22.4%) | 66 (17.9%) | 54 (16.8%) | |
| Very high | 13 (3.5%) | 18 (5.1%) | 10 (2.7%) | 11 (3.4%) | |
| Parental level of worry about health in family | None | 15 (4.1%) | 7 (2.0%) | 18 (5.5%) | 31 (9.6%) |
| Mild | 82 (22.2%) | 63 (17.9%) | 63 (19.1%) | 104 (28.5%) | |
| Moderate | 102 (27.6%) | 80 (22.8%) | 93 (28.2%) | 78 (24.2%) | |
| High | 134 (36.3%) | 133 (37.9%) | 117 (35.5%) | 73 (22.7%) | |
| Very high | 36 (9.8%) | 68 (19.4%) | 39 (10.6%) | 35 (10.9%) | |
| Perceived home environment | Very bad | 105 (28.6%) | 2 (0.6%) | 2 (0.6%) | 0 (0.0%) |
| Bad | 3 (0.8%) | 12 (3.4%) | 10 (3.1%) | 7 (2.2%) | |
| Normal | 0 (0.0%) | 109 (31.0%) | 103 (31.2%) | 76 (23.7%) | |
| Good | 160 (43.3%) | 151 (42.9%) | 135 (41.0%) | 149 (46.4%) | |
| Very good | 101 (27.2%) | 78 (22.2%) | 80 (24.2%) | 89 (27.7%) | |
| Were you confined at home? | Never | 339 (91.9%) | 224 (63.6%) | 216 (65.3%) | 233 (72.6%) |
| Once | 26 (7%) | 108 (30.7%) | 86 (26.1%) | 74 (23.1%) | |
| Twice | 3 (0.8%) | 14 (4.0%) | 24 (7.3%) | 13 (4.0%) | |
| > twice | 1 (0.3%) | 6 (1.7%) | 4 (1.1%) | 1 (0.3%) | |
| Did the child have COVID? | No | 362 (98.1%) | 335 (95.2%) | 317 (96.1%) | 310 (96.6%) |
| Yes, asymptomatic | 5 (1.4%) | 11 (3.1%) | 9 (2.7%) | 7 (2.2%) | |
| Yes, symptomatic | 2 (0.5%) | 6 (1.7%) | 4 (1.2%) | 4 (1.3%) | |
| Were there COVID cases in the family? | Yes | 61 (16.5%) | 74 (21.0%) | 64 (19.4%) | 43 (13.4%) |
| Was anyone in the family hospitalised? | Yes | 22 (6.0%) | 20 (5.6%) | 14 (4.2%) | 8 (2.5%) |
| Did anyone in the family die? | Yes | 9 (2.4%) | 5 (1.4%) | 4 (1.2%) | 3 (0.9%) |
| Did the child start to receive mental health services? | Yes | 23 (6.2%) | 19 (5.4%) | 24 (7.3%) | 21 (6.5%) |
The results obtained at the beginning of the school year, after a 6-month closure of schools in Catalonia, yielded a percentage of probable cases of psychiatric disorder of 9.8% among the patients,23 a clear increase compared to the 7.5% reported before the pandemic.19 Higher levels of worry in children regarding their own and their family’s health were associated with the presence of mental health problems, especially at the start of the year, while a positive perception of the home environment was associated with a lower risk. None of the variables related to COVID-19 were associated with abnormal scores in the SDQ. The proportion of children at risk of mental health disorders decreased gradually over the 4 timepoints to 6.2% at the end of the school year.
To our knowledge, no study published to date has followed up a cohort through the entire first year of school in the COVID-19 pandemic. Most studies conducted on the paediatric population have been cross-sectional, which carries intrinsic limitations, and only a few have yielded longitudinal data. Most of the latter have compared the prepandemic period with a single timepoint in the pandemic.9,24 The COPSY study published data on 2 timepoints covering a longer period. The clearest worsening in mental health occurred between the prepandemic period and the first timepoint (May–June 2020), although the mental health of children and adolescents continued to get worse through the second timepoint (December 2020–January 2021), coinciding with a significant confinement measures.25 In contrast, adolescents and young adults in the United States recovered prepandemic levels of mental health earlier, by summer of 2020.26 This differed from the results of the PEDSAME study, which found an even higher frequency of mental health problems in the autumn/winter of 2020 (9.8%/8.8%), without recovery of prepandemic mental health until later, in March and especially June 2021 (6.2%). The recovery of mental health to prepandemic levels could take longer in children and adolescents compared to adults,27 perhaps due to the imposition of greater restrictions to their school and social lives.
Most studies have identified adolescents as a subset of the population particularly vulnerable to mental health disorders during the COVID-19 pandemic.24,28 Our study also found a higher frequency of emotional symptoms in this age group compared to prepubertal children. However, we ought to underscore that the most affected age group was children aged 5–8 years, a difference that was significant in the first timepoint, in agreement with other studies that also used the SDQ or equivalent instruments.29,30 This could be due to a frequent focus on internalizing disorders, such as depression and anxiety,18,31 while little attention has been paid to externalising disorders32 (conduct disorder or attention-deficit hyperactivity disorder), the incidence of which, as observed in our study, is higher at younger ages. The SDQ has proven to be a useful instrument to assess the risk of mental health disorders in children. It allows assessment, on one hand, of internalizing symptoms and, on the other, externalising symptoms, which are more prevalent in younger children and which may go undetected.
The restrictions imposed in successive waves, although generally less strict compared to the initial home confinement measure, could explain the greater impact on the mental health of younger children, who need spaces outside the home to move around and socialize, as opposed to adolescents who can partly make up for restrictions through online social interaction. In younger children, the inability to understand the reasons for confinement and other changes in their routine on account of the pandemic could contribute to the increase in anxiety and suffering related to COVID-19.29,33
When it came to the variables associated with changes in mental health, we found that the level of worry of both children and parents regarding health, identified as a determinant of mental health,34 decreased over the school year. In fact, only the worry of children was significantly associated with an increased risk of mental health problems, and only at the beginning of the school year. On the other hand, a positive perception of the home environment was associated with adequate mental health throughout the follow-up. Numerous studies have found that the level of anxiety10 or neuroticism of parents35 is associated with abnormal SDQ results in children.36 Several authors25,37 have found that a positive home environment (adequate social support and good communication within the family) was associated with better mental health status in children, and especially in adolescents, during the pandemic.38 On the other hand, none of the variables directly related to COVID-19 was significantly associated with mental health. Contrary to the findings of Matalí-Costa and Camprodon-Rosanas,29 we did not find an association between a death in the family and less favourable results in the SDQ. The CLoCk study, conducted in England, also did not find significant differences in the frequency of abnormal SDQ scores between children that had positive SARS-CoV-2 test results and children who did not.39 The variable associated most strongly with abnormal results in the SDQ was a previous diagnosis of psychiatric or neurodevelopmental disorders, in agreement with the previous literature,32,40 as was to be expected.
The analysis of the data collected in the PEDSAME study throughout the 2020–2021 school year show that, in spite of experiencing the pandemic, the percentage of children considered probable cases of mental disorder decreased over the year. Each of the timepoints happened to coincide with the different waves of the COVID-19 pandemic in Spain, in spite of which the percentage of children with SDQ scores in the abnormal range kept decreasing. It is possible that the relaxation of social distancing measures (opening schools and allowing a degree of social contact) played a part in this improvement. Several studies have evinced the negative impact of school closures on the mental health of children.4,24,25,40 While the PEDSAME study was not designed to assess the role of schools in paediatric mental health, the progressive decrease in mental health problems over the school year supports this hypothesis and could support the exertion of extreme caution in imposing school closures in the future.
The most important limitation of the study is that we did not have questionnaires completed by the children themselves from a certain age. Internalizing symptoms are more easily identified if the source is the patient versus a proxy; nevertheless, the analysis detected an increase in emotional symptoms in the subgroup aged 12–14 years. The mother completed the questionnaire in 86.2% of cases, a sex disparity that could be a source of bias. This is a consistent issue across studies.29,34,39 We controlled for the risk of selection bias associated with differences in internet access by offering an interview, in person or by other means. We ought to highlight that the Catalonian public health system is universal and free of cost for all children, which limits the possibility of selection bias due to socioeconomic or cultural factors. The main strength of the PEDSAME study is that it was conducted in a random sample representative of the population, as opposed to a sample of convenience recruited through social networks or other channels. Secondly, it is one of the few longitudinal studies analysing child and adolescent mental health in the context of the pandemic, and the only one at the time of this writing that followed up the sample throughout the entire 2020–2021 school year, at 4 different timepoints, which allowed an adequate assessment of temporal trends in the cohort. The low proportion of participants lost to follow-up (13%) makes the results robust.
Additional population-based longitudinal studies would be helpful to gain a better understanding of the impact of pandemics on child and adolescent mental health. This would allow the identification and development of the most appropriate measures to confront them.
ConclusionThe mental health of children and adolescents in Catalonia, assessed by means of the SDQ in a paediatric sample, worsened 6 months into the pandemic during the closure of physical schools compared to previous population-based data. During the follow-up of the study cohort, we found that the proportion of children with a SDQ score in the abnormal range decreased through the 2020–2021 school year. The level of worry experienced by children about their own health and that of their family members was associated with the presence of mental health disorders, especially at the beginning of the school year. A positive perception of the home environment was associated with a lower frequency of mental health problems. None of the variables pertaining to COVID-19 was associated with having SDQ scores in the abnormal range.
Conflicts of interestThe authors have no conflicts of interest to declare.
We thank all the paediatricians and paediatric nurses of the XaRePAP who participated in the study for their time, dedication and patience. We also thank every child and adolescent who participated in the study as well as their parents for their dedication and perseverance in completing the questionnaires.
These authors have contributed equally to this article (shared first authorship).
Previous meetings: The results of the study were presented as an oral communication at the 18th Congress of Updates in Paediatric of the Asociación Española de Pediatría de Atención Primaria (AEPap), March 2022, Madrid, the XXVI Meeting of the Societat Catalana de Pediatria, June 2022, Lleida, and the 9th Congress of the European Academy of Paediatric Societies, October 2022, Barcelona.