Mobius syndrome is characterised by damage in the nucleus of the sixth and seventh cranial nerves, with subsequent facial palsy and abduction limitation of the eyes. The aim of this article is to describe the ophthalmological findings of the Mobius syndrome in Mexican children.
Patients and methodsA cross-sectional, retrospective, observational and descriptive study was conducted. A review was made of the clinical charts of patients with Mobius syndrome who were seen in the National Institute of Pediatrics in Mexico, between the years 2000 and 2010.
ResultsA total of 64 charts were reviewed. The most important findings were eye abduction limitation (100%), facial palsy (100%), esotropia (54%), epicanthus (51.5%), entropion (22%), and history of use of abortion inducers in the mother in the first trimester of pregnancy (28%). We also found exotropia and hypertropia in some cases.
ConclusionsMobius syndrome has a wide spectrum of ophthalmological manifestations that are important to detect early in order to improve function and aesthetics.
El síndrome de Möebius es una enfermedad caracterizada por lesión en los núcleos del sexto y séptimo nervios craneales, produciendo parálisis facial y limitación a la abducción principalmente. El objetivo es describir los hallazgos oftalmológicos del síndrome de Möebius en niños mexicanos.
Pacientes y métodosEstudio retrospectivo, transversal, observacional y descriptivo. Se revisaron expedientes clínicos de los pacientes con síndrome de Möebius del Instituto Nacional de Pediatría de México atendidos entre los años 2000 y 2010.
ResultadosSe revisaron 64 expedientes clínicos. Los hallazgos más importantes fueron limitación a la abducción (100%), parálisis facial (100%) endotropia (54%), epicanto (51,5%), entropión (22%) y antecedente de uso de abortivos en la madre durante el primer trimestre de embarazo (28%). Sin embargo, también se presentaron hallazgos atípicos como exotropia e hipertropia.
ConclusionesEl síndrome de Möebius tiene una amplia gama de manifestaciones oftalmológicas que se deben detectar temprano para mejorar su función y estética.
Limitation of eye movements associated with facial palsy was first described by von Graefe in 1880.1 However, it was Möbius who noticed the association of congenital facial palsy with other malformations between 1888 and 1892.2–7 Möbius syndrome is a disease characterised by lesions in the facial (VII) and abducen (VI) nerves, with possible involvement of other cranial nerves and traversing long tracts in the brainstem. Its main manifestations are facial palsy, impairment of ocular abduction, and horizontal vergence abnormalities. Since it is a rare congenital disorder, there are few statistical data regarding its incidence.
Its cause remains unknown, and most cases are sporadic. Towfighi et al.8 proposed a classification system based on neuropathologic findings, but it has not been fully accepted. Two possible aetiologies are hypothesised: a genetic defect leading to abnormal development of the brainstem, and an ischaemic origin possibly caused by intrauterine or environmental toxicity that restricts blood flow to the brainstem during early embryonic development.9–13
Cytogenetic studies have found 2 possible loci for the syndrome, 1p22 and 13q12.2-q13.14–21 Healthy parents of a child with Möbius syndrome have a low probability of having another child with the disease. However, Möbius syndrome may be familial in some patients.19
Maldevelopment has been associated with the use of misoprostol in the early stages of pregnancy.7,9,14,21–29 It has also been associated with exposure to infection, alcohol, cocaine, and thalidomide.30
Verzijl9,11 and Roig Quilis31 propose that the disease be redefined as a syndrome of rhomboencephalic maldevelopment or brainstem dysgenesis with involvement of motor nuclei and axons, as well as traversing long tracts.
In addition to facial and eye involvement, the syndrome can affect oropharyngeal, craniofacial, musculoskeletal, and neurologic structures.5,11,13,21–40
Five patterns of strabismus have been described:38 bilateral restriction of abduction, bilateral restriction of abduction and adduction, bilateral restriction of abduction and adduction with globe retraction in adduction (as seen in Duane syndrome), asymmetrical or unilateral alterations in ocular motility, and restricted horizontal and vertical movement.
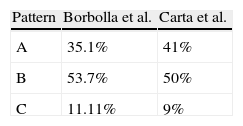
Carta et al.39 propose 3 patterns of strabismus. Pattern A consists of orthotopia due to damage to cells of the VI cranial nerve nucleus, the axons of which constitute the medial longitudinal fasciculus and synapse on the medial rectus subnucleus, leading to palsy in the lateral rectus muscle and balancing opposing forces so that the gaze is in primary position. Pattern B consists of esotropia due to bilateral lesion of only the ventral portion of the VI cranial nerve nucleus, leading to overreaction of the remaining neurons in the nucleus connecting to the subnucleus of the oculomotor (III) nerve, which innervates the contralateral medial rectus. Pattern C involves exotropia associated to vertical misalignment caused by rostral nerve damage extending into the midbrain, in proximity to the vertical gaze centre.
The first Möbius Syndrome Scientific Conference was held in Bethesda, Maryland, in 2007, during which the minimum diagnostic criteria for the syndrome were established: congenital, nonprogressive unilateral or bilateral facial palsy, and limitation of abduction. Additional findings may include deficits in other cranial nerves, and motor, orofacial, musculoskeletal, social, and neurodevelopmental impairment. Some authors use the term Möbius-like syndrome to refer to cases that do not meet the minimum criteria, although the difference between the two syndromes is not well defined.39
Since Möbius syndrome is a rare entity, few studies in the world make a detailed description of its ophthalmologic manifestations. We only know of one similar study in Latin America, performed in Brazil,40 while others are isolated case reports. The aim of our study is to offer a broader understanding of the ophthalmologic manifestations of this entity.
Patients and methodsWe conducted a descriptive, observational, cross-sectional retrospective study.
We reviewed the medical histories of patients with Möbius syndrome receiving care at the Instituto Nacional de Pediatría (National Paediatric Institute), Mexico, between 2000 and 2010, who met the minimum diagnostic criteria established at the First Möbius Syndrome Scientific Conference: congenital, nonprogressive unilateral or bilateral facial palsy, and limitation of abduction.
We collected and analysed data pertaining to the demographic characteristics and medical histories of the patients, reported by parents at the time of the first visit.
We recorded data on systemic manifestations, such as clubfoot, facial palsy, and psychomotor retardation. Special emphasis was placed on ophthalmologic findings. Visual acuity (VA) is reported using the Snellen scale; however, due to the young age at which most patients were admitted to the practise, we used a classification of VA based on fixation behaviour: central steady fixation (CSF), central unsteady fixation (CUF) and eccentric fixation (EF). Refraction defects were classified into 3 categories: simple myopia, simple hyperopia, and astigmatism.
We classified strabismus according to the direction (orthotropia, esotropia, exotropia, hypertropia and hypotropia), and magnitude (in prism dioptres [DPs]) of the deviation. Limitations of duction were classified into mild, moderate, or severe according to how far the eye could move away from an imaginary vertical or horizontal line passing through the centre of the palpebral fissure.
We also collected clinical data pertaining to the anterior and posterior eye segments and the annexes.
ResultsDemographic featuresWe reviewed the medical records of 64 patients with a final diagnosis of Möbius syndrome, 40 male (62.5%) and 24 female (37.5%). The age of the patients at the time of admission to the practise ranged from 1 to 135 months, with a mean age of 17 months. Of the 64 patients, 57 were diagnosed with Möbius syndrome, 5 had Poland syndrome, and the remaining 2 had Pierre Robin syndrome and Dandy Walker syndrome.
Medical historyEighteen mothers (28.1%) ingested abortion-inducing substances during the first trimester of gestation. Sixteen of them consumed misoprostol, 6 of them an unspecified substance described as an “abortive infusion”, and 1 an unspecified drug with the intention of aborting.
There were 28 mothers (43.7%) who ingested other medications or substances during the first trimester. The reported substances were tobacco, alcohol, birth-control medication, salbutamol, omeprazole, and acetylsalicylic acid.
Four mothers were younger than 18 years, and three were older than 35. The rest (89%) had ages ranging from 18 to 35 years.
A subset of mothers had a history of pregnancy complications: 22 patients had threatened miscarriage and 14 had urinary tract infections and/or cervicovaginitis. Rare events reported included presence of an intrauterine device (IUD) at the time of conception, prenatal diagnosis of intrauterine malnutrition and hydrocephalus, placenta previa, oligohydramnios, polyhydramnios, scorpion sting, dengue fever, gestational diabetes, and poliomyelitis.
Events prior to the pregnancy were also reported, including 2 pregnancies that resulted from sexual assault, a previous history of miscarriage in 2 mothers, and intake of retinoic acid for a year before conception in 1 mother.
A history of disease or malformation was reported for 3 fathers: 2 had polydactyly, and 1 had hepatitis C.
A familial history of the disease was not reported in any of the cases reviewed.
Fourteen patients had convulsive seizures (21.8%).
Physical examinationOphthalmologic findingsIn most patients, visual acuity was measured by means of a binocular assessment. Central steady fixation (CSF) was observed in 77.5% of the patients. Central unsteady fixation and eccentric fixation were observed in 4% of the patients. Among the patients in whom visual acuity could be measured, 10.2% had a VA ranging from 20/80 to 20/40, 4% had a VA greater than 20/30, and 4% had asymmetric VA and could not be included in either of the former categories.
As for refractive defects, 75% of the patients had simple hypermetropia, 17.8% astigmatism (myopic, hyperopic, and mixed), 3.5% simple myopia, and 3.5% emmetropia.
The medical records documented strabismus evaluations in 54 patients. Thirty-five of them (64.8%) had some type of strabismus, and 19 had orthotropia (35.1%). Isolated esotropia was the most frequent finding among patients with strabismus, accounting for 29 cases (82.8% of the cases of strabismus and 53.7% of the total number of cases in the study). Two patients had isolated exotropia, 2 patients esotropia associated to left hypertropia, 1 had isolated hypertropia, and the last one had exotropia associated to left eye hypertropia. The cases that involved some component of the vertical gaze (isolated or in association with a horizontal component) combined with isolated exotropias amount for 11.11% of the cases.
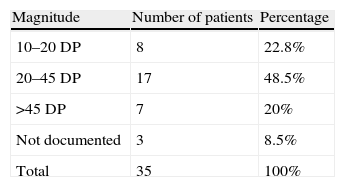
In most patients, the magnitude of strabismus ranged between 25 and 45 DP (Table 1).
An assessment of ductions and versions was documented in 49 cases. Of these, 100% had limited abduction in both eyes, and 16 cases (32.6%) also had limited adduction, 3 limited supraduction, and 2 limited infraduction.
The degree of duction limitation was described individually for each eye (98 eyes), and it was quantified empirically according to the distance travelled from the midline of the eye. The limitation was classified as severe if the eye did not travel beyond the midline, moderate if it passed the midline, and mild if it approached the corresponding palpebral canthus. Limited abduction was found in 100% of the eyes (severe in 76 eyes, moderate in 19, and mild in 3) and limited adduction was found in 32 (severe in 9 eyes, moderate in 21, and mild in 2). Inferior oblique overfunction was found in only 1 patient.
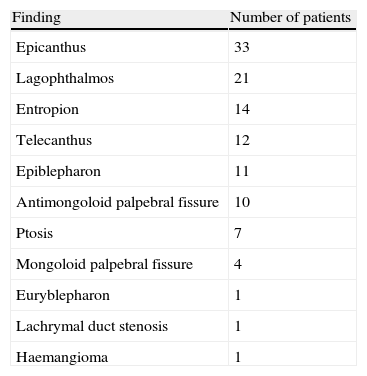
The examination of the eyelid and ocular annexes was documented in 100% of the medical histories. Epicanthus was the most frequent finding in these examinations (Table 2).
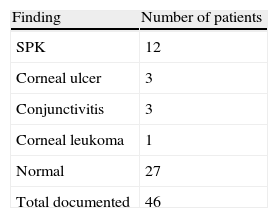
The anterior segment of the eye was affected in 19 patients. The condition found most frequently was superficial punctate keratopathy (Table 3).
Examination of the fundus revealed oblique optic disc in one patient.
Other physical findingsFacial palsy was bilateral in 52 patients and unilateral in 6; lateralisation was not specified in another 6.
Psychomotor development delays of varying degree were identified in 47 patients (73.4%). Delays were mild in 58.6% of the patients, moderate in 24.1%, and severe in 17.2%.
Twenty-seven patients (42.1%) had clubfoot, which was bilateral in 25, and unilateral in 2.
DiscussionFrom its earliest descriptions by von Graefe and Möbius1–3 to the various publications of cases and the few detailed descriptions of this entity, what we see is a group of patients with multiple systemic manifestations associated with a few common findings, specifically the presence of facial paralysis with abnormal ocular abduction. Recently it has been suggested that what we know as Möbius syndrome could be part of a disorder whose name or classification takes into account the different abnormalities involved and its pathoaetiology: rhomboencephalic maldevelopment (Verzijl et al.9–11) or brainstem dysgenesis (Roig Quilis31).
Male patients predominated in our study (62.3%), but other case series report a more balanced sex distribution.39,40
The aetiology of this syndrome remains unknown. Genetic and ischaemic causes for it have been hypothesised.9–21 The literature has also linked its development to exposure to misoprostol during gestation.7,9,14,21–29 Our analysis showed that nearly one third (28.1%) of the mothers of the patients in our series had used abortion-inducing substances in early pregnancy. Although the use of such substances was not specifically addressed in history taking, the documentation showed that 11 mothers (17.1%) had reported intake of misoprostol, and 6 (9.3%) consumption of herbal infusions with uterotonic properties. Considering that these percentages would be higher if mothers were specifically asked about the use of abortive substances, and that these substances are commonly sold illegally and without a prescription and extensively abused in Latin America, there may be a significant association between them and the development of Möbius syndrome. From a pathoaetiological perspective, these facts and the high percentage of genitourinary infections during pregnancy (21.8%) support the theory of an environmental (teratogenic, toxic, or infectious) or ischaemic cause for the development of the syndrome. No familial history of the disease was reported in any of the patients, and unfortunately no genetic tests had been performed to establish or determine the existence of genetic abnormalities that would support the theory that the disease has a genetic aetiology. Thus, we consider this a clear objective for future studies in our institution. An Italian case series39 showed a weaker association with the use of misoprostol, which was reported in only 2 of 55 cases, while the percentage reported in Brazil is higher (56.5%).40
Ophthalmologic data revealed that most patients (77.5%) had 20/100 vision in both eyes, and suggested the presence of amblyopia in only 2. This could be due to the presence of cross fixation, which does not allow the eyes to become amblyopic. Of the 2 patients with amblyopia, 1 had exotropia and the other hypertropia. As for refractive abnormalities, the large percentage of hyperopia (75%) could be due to the young age of the patients, and not be necessarily related to the features of the syndrome.
Two things stood out in the evaluation of strabismus: first, that while isolated esotropia is the most frequent type of strabismus in patients with Möbius syndrome, there were also patients with orthotropia, exotropia, and vertical movement defects. Second, that on analysing ocular ductions and versions, we found that while 100% of the patients presented limited abduction, a third of them (32.6%) also showed considerable restriction of adduction.
Similar findings were reported in the series of Carta et al.39 (Table 4). All their patients with orthotropia had limitations in conjugate movements with complete absence of convergence, and none had abnormal vertical versions. Patients with esotropia had severely limited abduction and normal or partially maintained adduction. Lastly, patients with exotropia had severe limitations of horizontal movements associated with vertical movement abnormalities.
In light of these findings we propose the possibility that ocular motility defects go beyond the isolated palsy or paresis of the VI cranial nerves, and that there may be simultaneous involvement of the III and IV nerves in many patients. Are these patients affected by a syndrome other than the one known as Möbius syndrome, or are all patients affected by a single entity with different manifestations? Our data could support the redefinition of the syndrome proposed by Verzijl9 and Roig Quilis31; however, we believe that the results observed in our study should be confirmed by means of adjunct studies, such as electromyography and muscle biopsy. We hypothesise that orthotropia may result from damage to the interneurons that extend from the nucleus of the VI nerve and connect with the III cranial nerve subnucleus that innervates the medial rectus muscle, leading to paralysis or paresis of the muscle, balancing opposing muscle forces, and precluding deviation. We propose that hypertropias and exotropia could result from ventral damage affecting not only the pons, but also the midbrain in proximity to the vertical gaze centre.39 This information suggests that the syndrome does not involve only the nuclei, as one of the described patterns (pattern A) is compatible with interconnection abnormalities (medial longitudinal fasciculus) and another (pattern C) with abnormalities in structures of the dorsal mesencephalon.
Many of the ophthalmic findings of our study have been described previously in the literature (epicanthus, incomplete eyelid closure, lagophthalmos, telecanthus, ptosis, epiblepharon, etc.), but we would like to highlight a finding that, to our knowledge, has yet to be reported: palpebral entropion. Thorough examination of patients with Möbius, this has led to the detection of superior and/or inferior palpebral entropion in some of them (21.8% in our study). We think that this may be due to loss of muscle tone in the anterior lamella of the lid, with the subsequent inward folding of the edge of the eyelid.
The predominant findings in the anterior segment examination were keratitis, ulcers, and conjunctivitis, in most cases associated with lagophthalmos or rubbing of eyelashes against the ocular globe in patients with entropion or epiblepharon.
As expected, a review of the clinical findings in these patients revealed a broad range of abnormalities. Other frequent systemic manifestations were lack of facial expression, psychomotor retardation (in all its degrees), broad and/or depressed nasal bridge, high arched palate, micrognathia and/or retrognathia, short neck, facial asymmetry, low-set ears, clinodactyly, webbed hands and feet, hypoacusis, tongue hypoplasia, swallowing disorders, and toe hypoplasia and clubfoot (42.1%) which is bilateral in most cases. Thus, the majority of the abnormalities are neurologic, craniofacial, or musculoskeletal.
One case was associated with Pierre Robin syndrome, identified by the finding of retro-micrognathia, glossoptosis, cleft palate, narrow upper airway requiring tracheostomy, and pectus excavatum, which appeared in combination with the manifestations of Möbius syndrome.
Five patients had Poland syndrome. All of them had hypoplasia or agenesis of the pectoralis major muscle. In some, this was associated with nipple abnormalities such as athelia (absence of the nipple), nipple hypoplasia, wide-spaced nipples; and ipsilateral hand malformations (agenesia, hypoplasia).
From a neurological standpoint, a remarkably high number of patients with this syndrome show delays in psychomotor development (73.4%). This may be related to systemic abnormalities such as hypoacusis or cleft lip and palate, which affect proper language development; to the convulsive seizures that affected 21% of our patients; or to the lack of facial expression that precludes assessment of social milestones such as smiling. Considering that life expectancy is long in these patients, early diagnosis and initiation of rehabilitation services are essential.
ConclusionMöbius syndrome is a rare entity. Its classical manifestations are lack of facial expression and esotropia. Our study showed that not all of our patients fitted that picture, as in some the syndrome may be associated with palsy of other cranial nerves. The use of abortive substances during pregnancy was documented in the medical records of a third of our patients. There are notable differences in the incidence of Möbius syndrome between Europe and Latin America, probably due to a more stringent control of the use of drugs and medicines during pregnancy in Europe.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Borbolla Pertierra AM, Acevedo González P, Bosch Canto V, Ordaz Favila JC, Juárez Echenique JC. Manifestaciones oculares y sistémicas del síndrome de Möebius. An Pediatr (Barc). 2014;81:297–302.
Previous presentations: This study was presented at the 2nd World Congress of Pediatric Ophthalmology and Strabismus; September 7–9, 2012, Milan, Italy; and at the Congreso Mexicano de Oftalmología; June 9–13, 2003, Guadalajara, Jalisco, Mexico.