Moebius syndrome (MS) is characterised by non-progressing congenital facial palsy and impaired ocular abduction due to involvement of the VII (facial) and VI (abducens) cranial nerves, respectively. Its prevalence is estimated at 1 in 125000 live births, with no difference between the sexes.1 The aetiology of MS is unknown; the disorder has been associated with genetic and environmental factors, such as foetal ischaemia and the use of drugs such as misoprostol during early pregnancy.2 Although it is widely known as MS, from the perspective of dysmorphology it would be more correctly termed as a sequence, as an initial change during embryonal development would result in a cascade of secondary events.
Moebius syndrome can be diagnosed early in the neonatal period. Its characteristic features are deficient sucking due to incomplete closure of the lips, the absence of a facial expression, incomplete closure of the eyelids during sleep, drooling and esotropia.1
Abnormalities in swallowing and breathing are frequent in newborns with this disease. Approximately 90% of these patients had craniofacial anomalies that predispose the newborn to airway obstruction.3
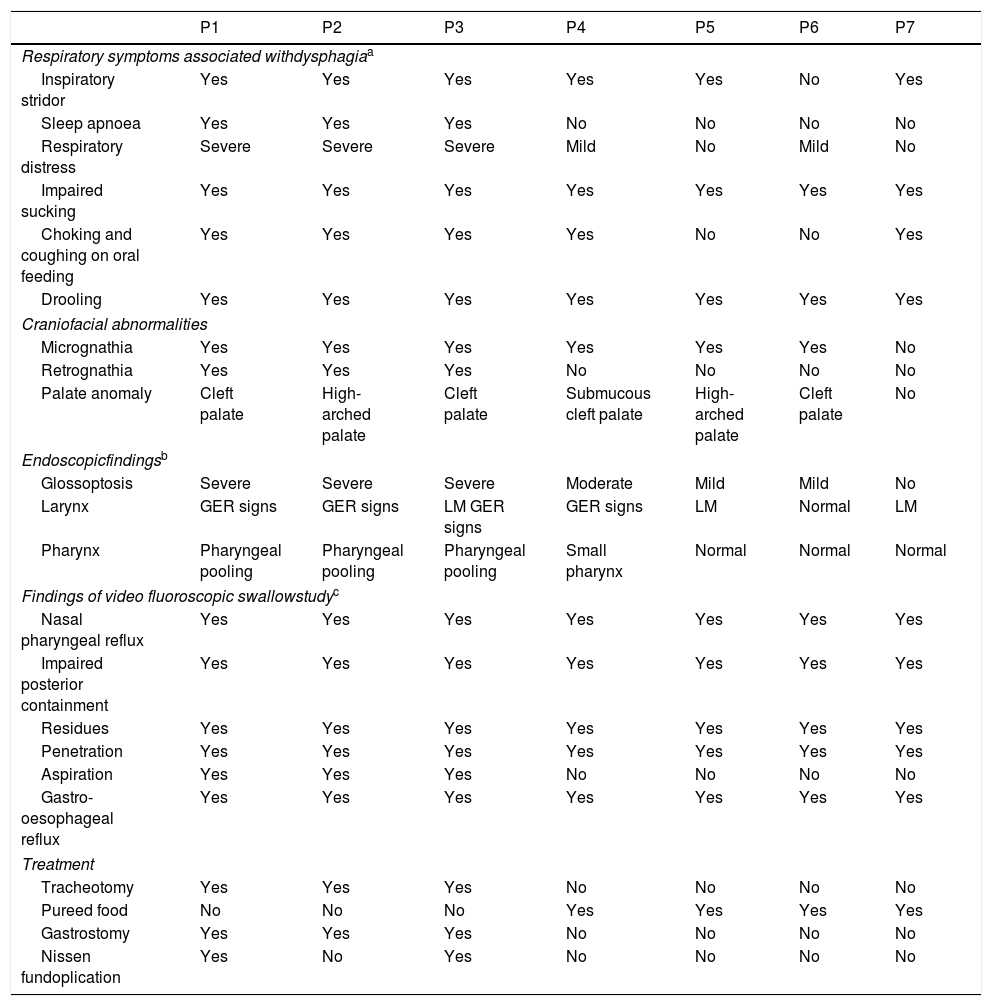
We made a retrospective review of the cases of 7 newborns (5 male) with MS managed at the department of otorhinolaryngology in the 2006–2018 period, analysing the clinical manifestations, the findings of endoscopy and the video fluoroscopic swallow study and the treatment received (Table 1).
Clinical manifestations, craniofacial anomalies, findings of endoscopic examination and video fluoroscopy swallow study, and treatment of patients with MS.
| P1 | P2 | P3 | P4 | P5 | P6 | P7 | |
|---|---|---|---|---|---|---|---|
| Respiratory symptoms associated withdysphagiaa | |||||||
| Inspiratory stridor | Yes | Yes | Yes | Yes | Yes | No | Yes |
| Sleep apnoea | Yes | Yes | Yes | No | No | No | No |
| Respiratory distress | Severe | Severe | Severe | Mild | No | Mild | No |
| Impaired sucking | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Choking and coughing on oral feeding | Yes | Yes | Yes | Yes | No | No | Yes |
| Drooling | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Craniofacial abnormalities | |||||||
| Micrognathia | Yes | Yes | Yes | Yes | Yes | Yes | No |
| Retrognathia | Yes | Yes | Yes | No | No | No | No |
| Palate anomaly | Cleft palate | High-arched palate | Cleft palate | Submucous cleft palate | High-arched palate | Cleft palate | No |
| Endoscopicfindingsb | |||||||
| Glossoptosis | Severe | Severe | Severe | Moderate | Mild | Mild | No |
| Larynx | GER signs | GER signs | LM GER signs | GER signs | LM | Normal | LM |
| Pharynx | Pharyngeal pooling | Pharyngeal pooling | Pharyngeal pooling | Small pharynx | Normal | Normal | Normal |
| Findings of video fluoroscopic swallowstudyc | |||||||
| Nasal pharyngeal reflux | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Impaired posterior containment | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Residues | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Penetration | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Aspiration | Yes | Yes | Yes | No | No | No | No |
| Gastro-oesophageal reflux | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Treatment | |||||||
| Tracheotomy | Yes | Yes | Yes | No | No | No | No |
| Pureed food | No | No | No | Yes | Yes | Yes | Yes |
| Gastrostomy | Yes | Yes | Yes | No | No | No | No |
| Nissen fundoplication | Yes | No | Yes | No | No | No | No |
LM, laryngomalacia; MS, Moebius syndrome; P, patient.
GER signs: indirect signs of gastro-oesophageal reflux (arytenoid swelling and redness, congestion of the mucosa of the posterior pharyngeal wall).
All the patients had strabismus and bilateral facial palsy (Fig. 1). Three patients (42.9%) had a history of maternal use of a drug use to induce abortion (misoprostol) in the first trimester of pregnancy. Three patients presented associated malformations: Poland syndrome in 1 (hypoplasia of the major pectoralis muscle) and Pierre-Robin sequence in 2 (retrognathia, cleft palate and glossoptosis).
Newborn with bilateral facial palsy at rest (A) and during crying (B): (A) incomplete closure of eyelids (lagophthalmos). (B) Evident facial asymmetry during crying. “Mask face” with partial conservation of function of right inferior facial musculature (deviation of homolateral corner of the mouth). (C) Same patient featured in A and B at age 3 months with nasogastric and a tracheostomy tubes. Evidence of esotropia and low position of the ears. (D) Bilateral clubfoot.
The examination detected micrognathia, palate anomalies and glossoptosis in 6 patients (85.7%) and retrognathia in 3 (42.9%). The 3 patients that experienced severe respiratory distress underwent intubation with a Holinger anterior commissure laryngoscope by an ear, nose and throat (ENT) specialist with specific training in complex airway management in children, followed by performance of tracheotomy.
The video fluoroscopic swallow study revealed laryngeal penetration in all patients and lower airway aspiration in 3 (42.9%). All 7 patients underwent placement of a nasogastric tube in the first days of life. All received treatment for reflux and early swallowing rehabilitation.
Other findings included involvement of other cranial nerves (n=4), hypotonia (n=6), club foot (n=7), heart disease (n=2), chest and outer ear malformations (n=4).
The mean duration of follow-up was 6 years. Two patients still need tracheostomy and gastrostomy tubes and have language delay, autism and self-harming behaviours (P1 and P3). Another patient (P2) underwent decannulation at age 3 years, and at present can consume foods of any consistency by mouth and exhibits adequate cognitive functioning, as do the remaining patients.
The clinical picture of MS is heterogeneous. Its differential diagnosis must include various diseases that can cause facial paralysis: neonatal trauma (use of forceps), hereditary congenital facial paresis, myotonic dystrophy, infectious diseases (otitis, herpes zoster), various cancers or Guillain-Barré syndrome, among others.
As was the case in other published case series, we found a strong association between attempted termination of pregnancy with misoprostol and the subsequent birth of an individual with MS.2
Early rehabilitation of swallowing is essential. The combination of motor rehabilitation and dietary modification allow improvement in swallowing. In most cases, eating skills improve as the child grows. Gastrostomy is indicated in cases where safe and effective oral feeding cannot be achieved.
Retromicrognathia can cause posterior displacement of the tongue toward the pharynx (glossoptosis), obstructing the airway. Most patients respond to positional therapy, although extreme cases may require tracheotomy. At present, jaw distraction is the first-line treatment for this condition, as it prevents the need for tracheotomy and other, less effective procedures such as glossopexy.
Many children with MS require multiple surgeries, for instance, facial reconstructive surgery and/or surgical correction of strabismus. There is a high risk associated with the use of anaesthesia.4
Limited mouth opening, retromicrognathia, glossoptosis and cleft palate are frequent features in patients with MS that have been associated with failed or difficult intubation. In this patients, spontaneous ventilation should be considered with avoidance of muscle relaxants. Face masks with Guedel airways may be useful. Laryngeal mask airways and flexible bronchoscopy are alternative methods that should be available to patients.4–6
The management of children with MS requires a multidisciplinary team. Early rehabilitation is essential to optimise the recovery of the different impaired functions and improve outcomes and quality of life in these patients.
Please cite this article as: Cuestas G, Quiroga V, Zanetta A, Giménez E. Manejo de la vía aérea en el neonato con síndrome de Moebius. An Pediatr (Barc). 2019;91:264–267.