Isotonic fluids, in most cases, are the safest way to dispense fluids intravenously. The aim of this study was to determine the prescription of maintenance intravenous fluids and to study possible associated factors.
Material and methodA descriptive, cross-sectional, multi-centre study was performed. A questionnaire was sent nationwide to several healthcare providers via an online survey, sent by email through different Medical Scientific Societies, and the Official Spanish Medical Association, between December 2016 and December 2017.
ResultsA total of 487 questionnaires were received, of which 456 were submitted by paediatricians. More than one quarter (28.95%) (95% CI; 24.77–33.13) of the paediatricians usually dispense hypotonic fluids and 81.14% (95% CI; 77.54–84.74) prescribe infusion rates based on the Holliday and Segar protocol. The general profile of paediatricians who prescribe hypotonic fluids intravenously in Spain are medical residents, paediatricians working in paediatric non-intensive care units, in private hospitals, and those who recognise that no consensus exists among their direct work colleagues regarding this subject.
ConclusionsMore than twenty-five per cent of all paediatricians in our country continue to use hypotonic fluids as maintenance intravenous fluid therapy. There might be several potential factors associated to this. These kind of studies provide evidence of the great difficulties in transferring scientific knowledge to clinical practice.
Los fluidos isotónicos, en la mayoría de los casos, constituyen la forma más segura de administración de líquidos por vía intravenosa. Los objetivos de nuestro trabajo han sido describir las prácticas de prescripción de los fluidos intravenosos de mantenimiento y estudiar los posibles factores asociados.
Material y métodoEstudio transversal, descriptivo, multicéntrico de ámbito nacional, mediante encuesta on-line, difundida a través de sociedades científicas médicas y la Organización Médica Colegial, entre diciembre de 2016 y diciembre de 2017.
ResultadosUn total de 487 encuestas fueron recibidas, 456 de pediatras. El 28,95% (IC 95%: 24,77-33,13) de ellos prescribían habitualmente fluidos hipotónicos y el 81,14% (IC 95%: 77,54-84,74) se basaba en la regla de Holliday y Segar para calcular el volumen total a infundir. El perfil del pediatra en España que utiliza fluidos hipotónicos intravenosos es el de médico residente de pediatría, pediatra que trabaja en áreas diferentes a las unidades de cuidados intensivos pediátricos, en hospitales privados, y aquellos que reconocen que no existe un consenso al respecto en su grupo de trabajo.
ConclusionesMás de una cuarta parte de los pediatras en nuestro país sigue utilizando los fluidos hipotónicos como fluidoterapia intravenosa de mantenimiento. Diferentes factores podrían estar asociados a este hecho. Estos estudios son prueba de las grandes dificultades existentes para trasladar el conocimiento a la práctica.
Since the publication of the article by Holliday and Segar in 1957, maintenance intravenous fluid therapy (MIVFT) in paediatrics has consisted in the administration of hypotonic fluids, with the total volume calculated based on the estimated energy expenditure, which falls between the basal metabolic rate and the expenditure expected during normal physical activity.1 From then to now, there have been reports of cases of dilutional hyponatraemia secondary to the use of hypotonic fluids with an excess of electrolyte-free water, administration of excessive volumes or elevation of antidiuretic hormone (ADH) secondary to some disease-related processes.2,3 In 2003, Moritz et al. first proposed the use of isotonic fluids as a safer alternative to the traditional approach,4 a suggestion that was disputed in 2 articles written in response by Holliday et al.5,6 The latter structured their arguments around 2 main points, the normalization of the excess of ADH by intravenous administration of a bolus of isotonic fluid at a rate of 20–40mL/kg over 2–4h, and the current lack of evidence from clinical trials supporting the approach proposed by Moritz et al. However, the public health systems of different countries took the evidence on the risks of hypotonic fluids seriously and issued very clear recommendations on the subject.7–9 Two meta-analyses published in 201410,11 concluded that the use of isotonic fluids for MIVFT compared to hypotonic fluids decreased the risk (although not completely eliminating it) of development of hyponatraemia without increasing the risk of complications such as hypernatraemia, high blood pressure and/or oedema, as evinced by the clinical trial conducted by McNab et al.12 However, most of the patients included in the reviewed studies were postsurgical patients or patients with severe illness admitted to the paediatric intensive care unit (PICU), so the conclusions of these meta-analyses may not be applicable to patients in non-intensive care wards. In 2015, Friedman et al.13 published a clinical trial that found no differences in sodium serum levels at 24 and 48h from initiation of MIVFT, regardless of whether the administered fluid was isotonic (sodium chloride [NaCl] 0.9%+dextrose [D] 5%) or hypotonic (NaCl 0.45%+D 5%). However, the 2 observed cases of hyponatraemia occurred in 2 patients of the hypotonic fluid group, requiring their removal from the study 24h after initiation of infusion. In the same study, there were cases of high blood pressure, hypernatraemia and oedema in the isotonic fluid group, which seriously challenged the strong evidence in favour of isotonic fluids of the meta-analyses published a year before.10,11
In the past decade, several studies have found variability in the approaches to the delivery of MIVFT, and at present, the Holliday–Segar method continues to prevail in everyday clinical practice.14–19
In this framework, the aim of our study was to describe the knowledge and attitudes of health care providers in Spain regarding MIVFT in paediatrics, their variability, and the possible factors at play.
Materials and methodsStudy design and universeWe conducted a cross-sectional observational study. We started by reviewing the consensus guidelines on intravenous fluid therapy of the Sociedad Española de Pediatría Hospitalaria (Spanish Society of Paediatric Inpatient Care)20 and 2 other publications on the subject21,22 to develop a 19-item questionnaire (see the supplemental material in Appendix B) in Google Drive. Since there were no validated instruments that could be used for a study of this nature, we had to develop a questionnaire that, in the opinion of our research team, explored essential aspects of MIVFT taking into account the objectives of the study and based on the scientific evidence published to date: total volume to administer in 24h, tonicity and fluid ion composition. The questionnaire also had to explore factors related to the clinician and the care setting that might influence prescription practices, as had been done in previous studies.14–16 We distributed the final questionnaire electronically to Spanish regional and national as well as international medical and surgical societies whose members engage in paediatric care and may prescribe MIVFT, requesting their collaboration to distribute the questionnaire to their members. We also sent the link to the questionnaire to the Board of Physicians of the province where the study originated asking for help in distributing it to the remaining Boards in Spain. The online form that was distributed specified that only health providers that prescribed MIVFT to paediatric patients should complete the questionnaire.
Inclusion criteriaOur survey was aimed at all health care providers managing MIVFT in paediatric patients aged 1 month through 14 years in 4 key settings: emergency care, acute ward care, surgical care and paediatric intensive care.
Data collectionWe distributed the questionnaire online at three different time points following a pre-established protocol: first distribution, December 2016; second distribution, February to March 2017; third distribution, May 2017. We collected responses until December 31, 2017.
Statistical analysis of the dataAll the variables under study were qualitative, and we summarised the data as absolute frequencies and percentages with the corresponding 95% confidence intervals. We analysed the association between these variables by means of the chi square test. This was followed by a multivariate analysis using binary logistic regression, with a single dependent variable (“routine use of hypotonic fluids for MIVFT”) and including in the model the variables that had been significant or marginally significant in the bivariate analysis, or those that were not statistically significant but we considered clinically relevant. We defined statistical significance as a p-value of less than 0.05 and marginal significance as a p-value of at least 0.05 but less than 0.25.
We calculated that a sample size of 385 would be sufficient to estimate population proportions, for an assumed proportion of approximately 50%, with a 95% level of confidence and a precision of ±5 percentage points. We performed the statistical analysis with the software SPSS for Windows version 21.0 (SPSS Inc; Chicago, United States).
Ethical considerationsThe study was approved by the ethics and research committee of the coordinating hospital. It included no patient data, and participation in the survey was voluntary and anonymous. The researchers involved in the project were the sole individuals that had access to the survey data, which were collected solely for the purpose of statistical analysis.
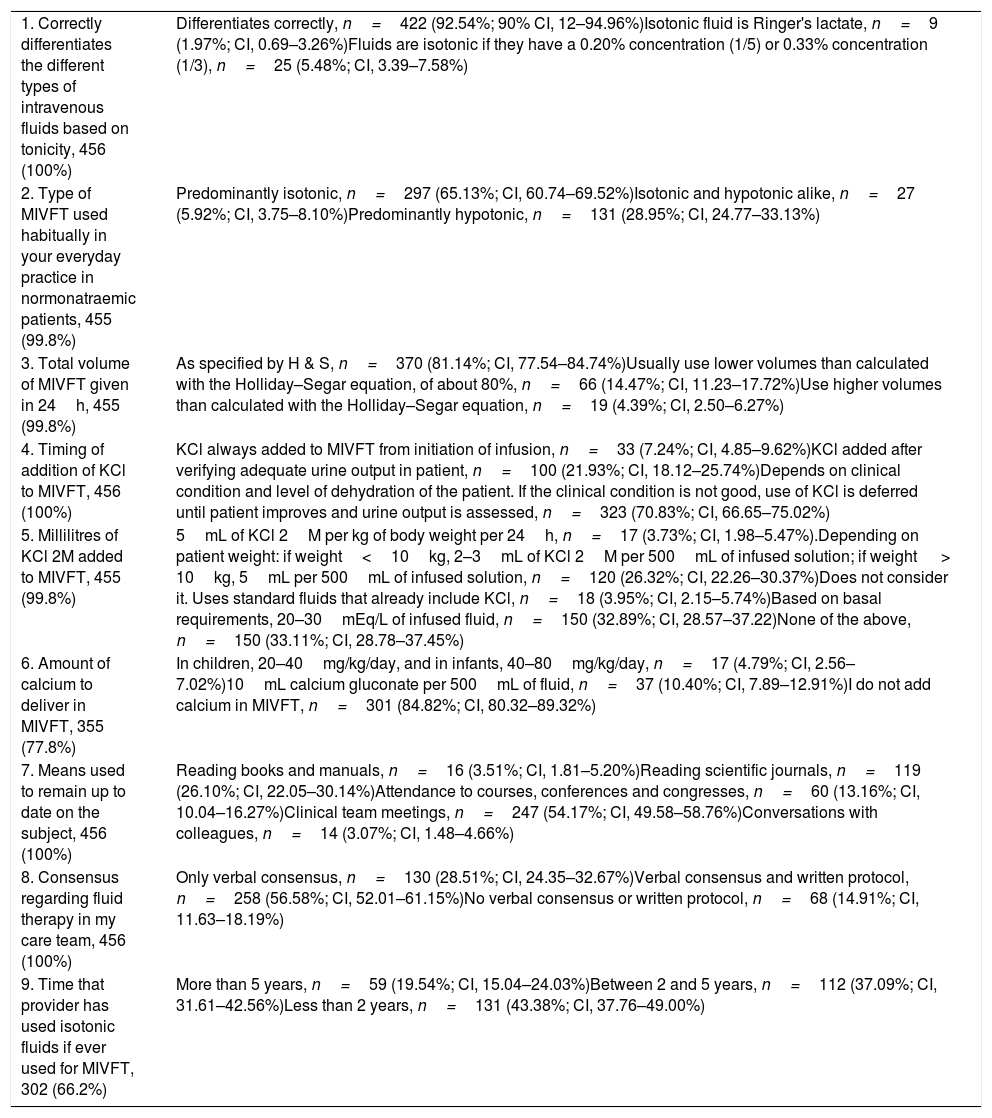
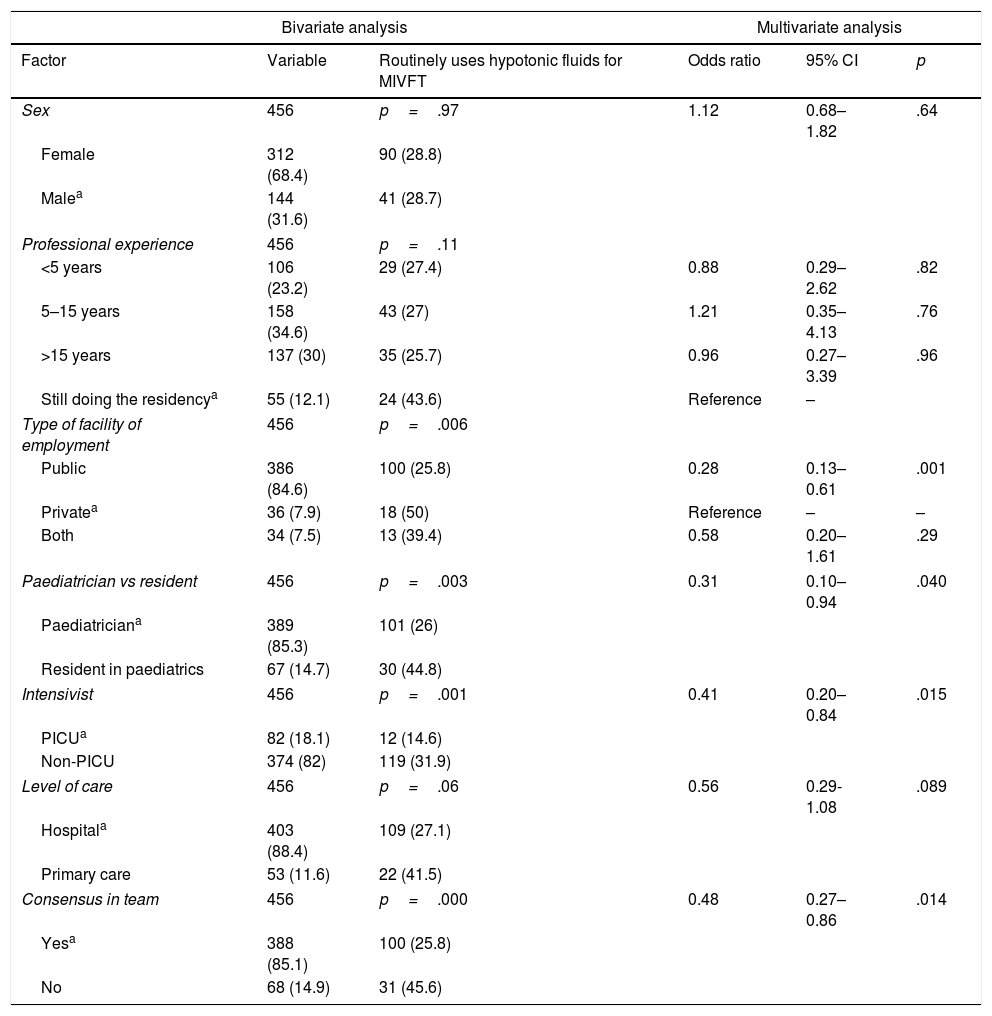
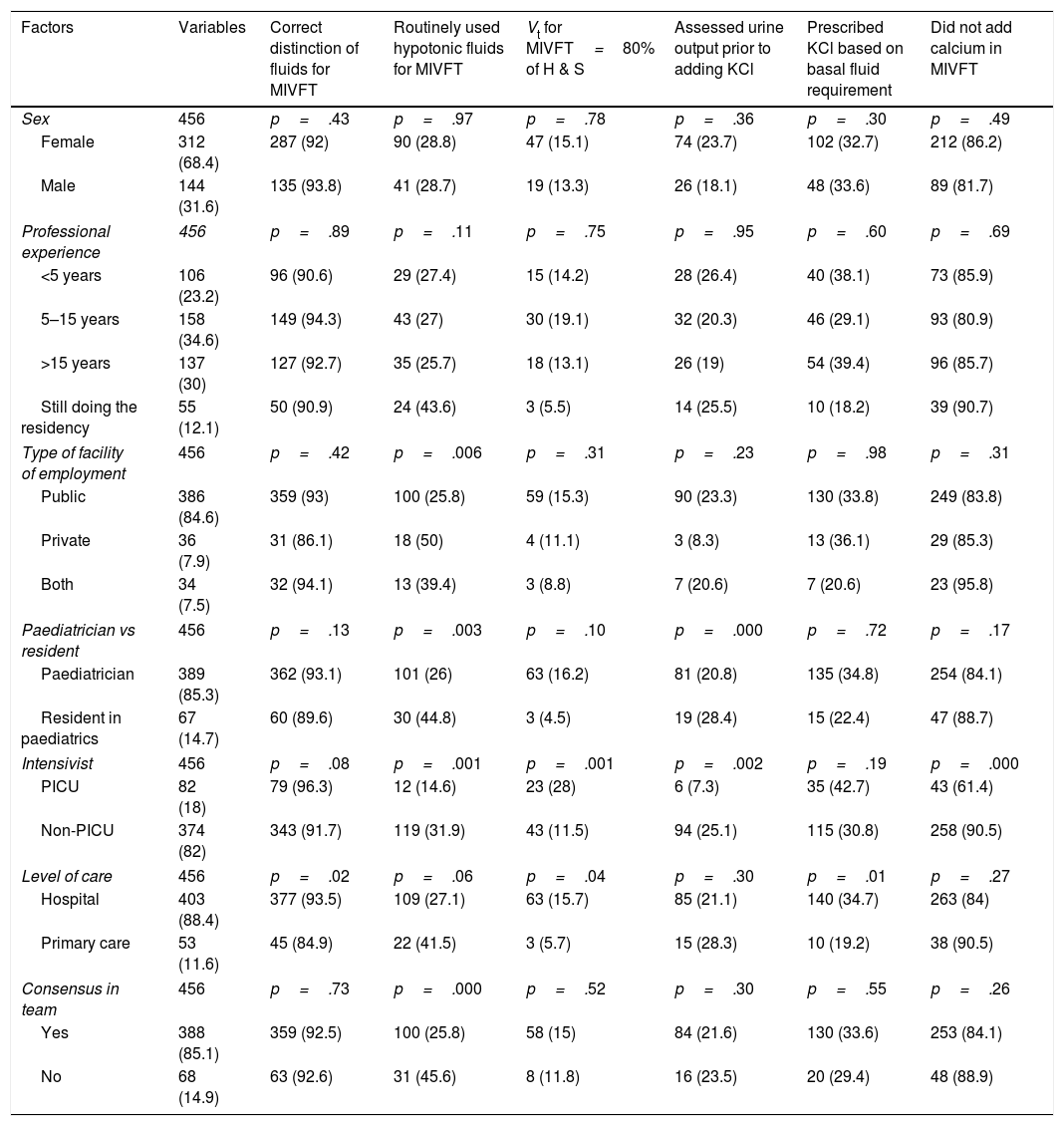
ResultsWe received a total of 487 responses, 456 from paediatricians, of whom 67 (14.69%) were residents in training. Based on data published by the Sociedad Española de Pediatría Hospitalaria,23 the total number of paediatricians employed in public and private hospitals in Spain amounted to 4194 in 2011. This entails that the response rate for our survey was of approximately 10.8%. We received the most answers from the following 6 autonomous regions in Spain: Madrid, 115 (25.21%); Valencia, 105 (23.02%); Andalusia, 55 (12.06%); Canary Islands, 32 (7.03%); Castilla La Mancha, 31 (6.81%); and Catalonia, 28, (6.14%). We received a total of 90 responses from the remaining autonomous regions combined (19.73%). Table 1 summarises the questionnaire items and the answer choices. The most salient findings were that 7.45% (95% CI, 4.22–10.68%) of respondents did not correctly differentiate between hypotonic and isotonic from a conceptual standpoint. Hypotonic fluids were used habitually by 28.95% of clinicians (95% CI, 24.77–33.13%), and only 14.47% (95% CI, 11.23–17.72) used volumes smaller than the volumes that would be administered using the Holliday–Segar method. In addition, 14.91% of respondents (95% CI, 11.63–18.19%) reported that there was no consensus regarding this issue in their care team. On the other hand, we found an association between the use of hypotonic fluids and the characteristics of prescribing clinicians and their work settings. Table 2 presents the results of the bivariate and multivariate analyses on this aspect, highlighting the factors with the strongest correlation to the prescription of hypotonic fluids. The use of volumes smaller than those proposed traditionally was also associated to a specific professional profile, as clinicians employed in PICU settings were more likely to use smaller volumes compared to those employed in non-intensive care settings (28% versus 11.5%). Only 19 of the surveyed paediatricians (4.3%) used volumes greater than recommended by Holliday and Segar, and 9 of them (2% of the total) also prescribed hypotonic fluids. Table 3 presents results on other aspects related to the prescription of MIVFT and some factors that may be associated with it.
Main questions asked in the questionnaire and percent distribution of answers given to each.
| 1. Correctly differentiates the different types of intravenous fluids based on tonicity, 456 (100%) | Differentiates correctly, n=422 (92.54%; 90% CI, 12–94.96%)Isotonic fluid is Ringer's lactate, n=9 (1.97%; CI, 0.69–3.26%)Fluids are isotonic if they have a 0.20% concentration (1/5) or 0.33% concentration (1/3), n=25 (5.48%; CI, 3.39–7.58%) |
| 2. Type of MIVFT used habitually in your everyday practice in normonatraemic patients, 455 (99.8%) | Predominantly isotonic, n=297 (65.13%; CI, 60.74–69.52%)Isotonic and hypotonic alike, n=27 (5.92%; CI, 3.75–8.10%)Predominantly hypotonic, n=131 (28.95%; CI, 24.77–33.13%) |
| 3. Total volume of MIVFT given in 24h, 455 (99.8%) | As specified by H & S, n=370 (81.14%; CI, 77.54–84.74%)Usually use lower volumes than calculated with the Holliday–Segar equation, of about 80%, n=66 (14.47%; CI, 11.23–17.72%)Use higher volumes than calculated with the Holliday–Segar equation, n=19 (4.39%; CI, 2.50–6.27%) |
| 4. Timing of addition of KCl to MIVFT, 456 (100%) | KCl always added to MIVFT from initiation of infusion, n=33 (7.24%; CI, 4.85–9.62%)KCl added after verifying adequate urine output in patient, n=100 (21.93%; CI, 18.12–25.74%)Depends on clinical condition and level of dehydration of the patient. If the clinical condition is not good, use of KCl is deferred until patient improves and urine output is assessed, n=323 (70.83%; CI, 66.65–75.02%) |
| 5. Millilitres of KCl 2M added to MIVFT, 455 (99.8%) | 5mL of KCl 2M per kg of body weight per 24h, n=17 (3.73%; CI, 1.98–5.47%).Depending on patient weight: if weight<10kg, 2–3mL of KCl 2M per 500mL of infused solution; if weight > 10kg, 5mL per 500mL of infused solution, n=120 (26.32%; CI, 22.26–30.37%)Does not consider it. Uses standard fluids that already include KCl, n=18 (3.95%; CI, 2.15–5.74%)Based on basal requirements, 20–30mEq/L of infused fluid, n=150 (32.89%; CI, 28.57–37.22)None of the above, n=150 (33.11%; CI, 28.78–37.45%) |
| 6. Amount of calcium to deliver in MIVFT, 355 (77.8%) | In children, 20–40mg/kg/day, and in infants, 40–80mg/kg/day, n=17 (4.79%; CI, 2.56–7.02%)10mL calcium gluconate per 500mL of fluid, n=37 (10.40%; CI, 7.89–12.91%)I do not add calcium in MIVFT, n=301 (84.82%; CI, 80.32–89.32%) |
| 7. Means used to remain up to date on the subject, 456 (100%) | Reading books and manuals, n=16 (3.51%; CI, 1.81–5.20%)Reading scientific journals, n=119 (26.10%; CI, 22.05–30.14%)Attendance to courses, conferences and congresses, n=60 (13.16%; CI, 10.04–16.27%)Clinical team meetings, n=247 (54.17%; CI, 49.58–58.76%)Conversations with colleagues, n=14 (3.07%; CI, 1.48–4.66%) |
| 8. Consensus regarding fluid therapy in my care team, 456 (100%) | Only verbal consensus, n=130 (28.51%; CI, 24.35–32.67%)Verbal consensus and written protocol, n=258 (56.58%; CI, 52.01–61.15%)No verbal consensus or written protocol, n=68 (14.91%; CI, 11.63–18.19%) |
| 9. Time that provider has used isotonic fluids if ever used for MIVFT, 302 (66.2%) | More than 5 years, n=59 (19.54%; CI, 15.04–24.03%)Between 2 and 5 years, n=112 (37.09%; CI, 31.61–42.56%)Less than 2 years, n=131 (43.38%; CI, 37.76–49.00%) |
The left column presents the question asked, expressing the number of answers received as absolute frequency and percentage of the total in parenthesis. The right column shows the different answer choices and gives the absolute frequency and the percentage corresponding to each of them with the 95% confidence interval in parenthesis.
CI, confidence interval; KCl, potassium chloride; MIVFT, maintenance intravenous fluid therapy; 2M, 2 molar.
Factors associated with the prescription of hypotonic fluids for maintenance intravenous fluid therapy: bivariate and multivariate analysis.
| Bivariate analysis | Multivariate analysis | ||||
|---|---|---|---|---|---|
| Factor | Variable | Routinely uses hypotonic fluids for MIVFT | Odds ratio | 95% CI | p |
| Sex | 456 | p=.97 | 1.12 | 0.68–1.82 | .64 |
| Female | 312 (68.4) | 90 (28.8) | |||
| Malea | 144 (31.6) | 41 (28.7) | |||
| Professional experience | 456 | p=.11 | |||
| <5 years | 106 (23.2) | 29 (27.4) | 0.88 | 0.29–2.62 | .82 |
| 5–15 years | 158 (34.6) | 43 (27) | 1.21 | 0.35–4.13 | .76 |
| >15 years | 137 (30) | 35 (25.7) | 0.96 | 0.27–3.39 | .96 |
| Still doing the residencya | 55 (12.1) | 24 (43.6) | Reference | – | |
| Type of facility of employment | 456 | p=.006 | |||
| Public | 386 (84.6) | 100 (25.8) | 0.28 | 0.13–0.61 | .001 |
| Privatea | 36 (7.9) | 18 (50) | Reference | – | – |
| Both | 34 (7.5) | 13 (39.4) | 0.58 | 0.20–1.61 | .29 |
| Paediatrician vs resident | 456 | p=.003 | 0.31 | 0.10–0.94 | .040 |
| Paediatriciana | 389 (85.3) | 101 (26) | |||
| Resident in paediatrics | 67 (14.7) | 30 (44.8) | |||
| Intensivist | 456 | p=.001 | 0.41 | 0.20–0.84 | .015 |
| PICUa | 82 (18.1) | 12 (14.6) | |||
| Non-PICU | 374 (82) | 119 (31.9) | |||
| Level of care | 456 | p=.06 | 0.56 | 0.29-1.08 | .089 |
| Hospitala | 403 (88.4) | 109 (27.1) | |||
| Primary care | 53 (11.6) | 22 (41.5) | |||
| Consensus in team | 456 | p=.000 | 0.48 | 0.27–0.86 | .014 |
| Yesa | 388 (85.1) | 100 (25.8) | |||
| No | 68 (14.9) | 31 (45.6) | |||
CI, confidence interval; PICU, paediatric intensive care unit.
Factors associated with different aspects of the maintenance intravenous fluid therapy prescribed by clinicians: bivariate analysis.
| Factors | Variables | Correct distinction of fluids for MIVFT | Routinely used hypotonic fluids for MIVFT | Vt for MIVFT=80% of H & S | Assessed urine output prior to adding KCl | Prescribed KCl based on basal fluid requirement | Did not add calcium in MIVFT |
|---|---|---|---|---|---|---|---|
| Sex | 456 | p=.43 | p=.97 | p=.78 | p=.36 | p=.30 | p=.49 |
| Female | 312 (68.4) | 287 (92) | 90 (28.8) | 47 (15.1) | 74 (23.7) | 102 (32.7) | 212 (86.2) |
| Male | 144 (31.6) | 135 (93.8) | 41 (28.7) | 19 (13.3) | 26 (18.1) | 48 (33.6) | 89 (81.7) |
| Professional experience | 456 | p=.89 | p=.11 | p=.75 | p=.95 | p=.60 | p=.69 |
| <5 years | 106 (23.2) | 96 (90.6) | 29 (27.4) | 15 (14.2) | 28 (26.4) | 40 (38.1) | 73 (85.9) |
| 5–15 years | 158 (34.6) | 149 (94.3) | 43 (27) | 30 (19.1) | 32 (20.3) | 46 (29.1) | 93 (80.9) |
| >15 years | 137 (30) | 127 (92.7) | 35 (25.7) | 18 (13.1) | 26 (19) | 54 (39.4) | 96 (85.7) |
| Still doing the residency | 55 (12.1) | 50 (90.9) | 24 (43.6) | 3 (5.5) | 14 (25.5) | 10 (18.2) | 39 (90.7) |
| Type of facility of employment | 456 | p=.42 | p=.006 | p=.31 | p=.23 | p=.98 | p=.31 |
| Public | 386 (84.6) | 359 (93) | 100 (25.8) | 59 (15.3) | 90 (23.3) | 130 (33.8) | 249 (83.8) |
| Private | 36 (7.9) | 31 (86.1) | 18 (50) | 4 (11.1) | 3 (8.3) | 13 (36.1) | 29 (85.3) |
| Both | 34 (7.5) | 32 (94.1) | 13 (39.4) | 3 (8.8) | 7 (20.6) | 7 (20.6) | 23 (95.8) |
| Paediatrician vs resident | 456 | p=.13 | p=.003 | p=.10 | p=.000 | p=.72 | p=.17 |
| Paediatrician | 389 (85.3) | 362 (93.1) | 101 (26) | 63 (16.2) | 81 (20.8) | 135 (34.8) | 254 (84.1) |
| Resident in paediatrics | 67 (14.7) | 60 (89.6) | 30 (44.8) | 3 (4.5) | 19 (28.4) | 15 (22.4) | 47 (88.7) |
| Intensivist | 456 | p=.08 | p=.001 | p=.001 | p=.002 | p=.19 | p=.000 |
| PICU | 82 (18) | 79 (96.3) | 12 (14.6) | 23 (28) | 6 (7.3) | 35 (42.7) | 43 (61.4) |
| Non-PICU | 374 (82) | 343 (91.7) | 119 (31.9) | 43 (11.5) | 94 (25.1) | 115 (30.8) | 258 (90.5) |
| Level of care | 456 | p=.02 | p=.06 | p=.04 | p=.30 | p=.01 | p=.27 |
| Hospital | 403 (88.4) | 377 (93.5) | 109 (27.1) | 63 (15.7) | 85 (21.1) | 140 (34.7) | 263 (84) |
| Primary care | 53 (11.6) | 45 (84.9) | 22 (41.5) | 3 (5.7) | 15 (28.3) | 10 (19.2) | 38 (90.5) |
| Consensus in team | 456 | p=.73 | p=.000 | p=.52 | p=.30 | p=.55 | p=.26 |
| Yes | 388 (85.1) | 359 (92.5) | 100 (25.8) | 58 (15) | 84 (21.6) | 130 (33.6) | 253 (84.1) |
| No | 68 (14.9) | 63 (92.6) | 31 (45.6) | 8 (11.8) | 16 (23.5) | 20 (29.4) | 48 (88.9) |
KCl, potassium chloride; H & S, Holliday and Segar; MIVFT, maintenance intravenous fluid therapy; PICU, paediatric intensive care unit; Vt, total volume.
There is a substantial amount of evidence that supports the use of isotonic fluids for MIVFT.10,11,24 Thus, it seems that the time has come to consider switching from the use of hypotonic fluids (NaCl≤0.45%+D 5%) to the use of isotonic fluids (NaCl 0.9%+D 5%) in the majority of patients receiving MIVFT.25–27 However, studies conducted in different countries show that this is not happening,14–19 including our own, as 28.9% of respondents reported the routine use of hypotonic fluids in their usual clinical practice. Furthermore, 7.4% of the clinicians included in our study did not correctly differentiate intravenous fluids based on tonicity. On the other hand, from a physiological perspective it seems logical that using as reference the volumes proposed by Holliday and Segar, which are calculated based on healthy children with normal activity, we may be overestimating the fluid requirements of hospitalised patients, given the inactivity associated with any hospital stay and the retention of free water that may result from the elevation of ADH in response to various non-osmotic stimuli present in these patients. For this reason, some providers prescribe lower total volumes for MIVFT, as evinced by the study of Davies et al.15 In our study, 14.4% of respondents overall restricted the volume of fluids delivered for maintenance in their patients, and this proportion rose to 28% when it came to clinicians in the PICU. However, it is not possible to accurately determine the potency of the non-osmotic stimuli that patients experience during hospitalization. Surgical patients and patients with conditions involving the central nervous system (meningitis, encephalitis and severe head trauma) are likely to have the most elevated levels of ADH, and thus may be at highest risk of dilutional hypernatraemia if they are given hypotonic fluids in volumes calculated with the Holliday–Segar method. However, there are other hospitalised patients with mild diseases who, unlike the subsets of patients mentioned above, may not experience non-osmotic stimuli for ADH secretion and in whom prescription of volumes following the Holliday–Segar method may therefore be appropriate. The highest risk of dilutional hyponatraemia for paediatric inpatients would probably be associated with administration of hypotonic fluids at volumes above those recommended by Holliday and Segar, although we cannot assert this with confidence on the basis of the evidence that is currently available.3 We ought to highlight that while this practice was rare in our sample, reported by only 2% of respondents, we cannot assume that this is the case in the real world given the results of the study conducted in 2008 by Davies et al,15 in which up to 38% used maintenance rates above the Holliday–Segar standard which, combined with the use of hypotonic fluids, constituted an unsafe practice for the patient. Similarly, a recent systematic review with meta-analysis found an association between fluid overload and an increase in morbidity and mortality in critically ill paediatric patients.28
We did not find any studies in the literature describing clinical practice on this regard focused specifically on paediatricians. Most studies on the subject, with a survey format, assessed the knowledge of health care providers as to the type of fluids that must be administered in terms of tonicity and total volume with the presentation of different clinical scenarios. They found substantial variability on the type of fluid that would be used, with an overall predominance of hypotonic fluids, and no restriction on their volume. These differences have not been studied in depth, although Way et al.14 concluded that having received more extensive specific training on the subject and having performed more interventions on paediatric patients were associated with a higher probability of prescribing isotonic fluids. In a single-centre study conducted on a heterogeneous group of physicians, Keijzers et al.16 found that the correct choice of fluids in terms of tonicity and volume of infusion for a given clinical scenario was correlated to the amount of experience in the management of paediatric patients, with being a paediatrician or emergency care specialist versus a physician of any other specialty (surgery, anaesthesia), and with having received specific training on the prescription of fluids for maintenance in paediatric patients. Other studies have simply assessed the knowledge of clinicians in relation to the best available evidence at the moment, with some authors concluding that there is an increased tendency to prescribe hypotonic fluids in clinical situations that call for isotonic fluids when the patient is an infant aged less than 12 months compared to older patients.15–17,19
In our study, we found that working in a public versus a private health care facility, working in a PICU versus any other non-intensive care setting, being a paediatrician versus a resident in paediatrics and the presence versus the absence of a consensus on the practices related to MIVFT in the care team are factors that could be associated to the prescription or non-prescription of hypotonic fluids and the alternative use of isotonic fluids for MIVFT.
We also analysed prescription practices regarding the addition of potassium and calcium ions as components of MIVFT. We did not find any articles in the literature addressing specific aspects on the subject, such as deferring the addition of potassium to MIVFT until adequate urine output has been verified in the patient. Some manuals recommend doses of KCl of 20–40mEq/L,21,22 and we found no evidence in the literature on the optimal dosage. Another salient finding was the differences in opinion we found in regard to the addition of calcium, with the highest frequency of this practice found in intensive care specialists. Calcium homeostasis is of utmost importance in critical patients, especially those with polytrauma or in shock.29 This may be the reason why providers working in intensive care units are more likely to add this ion to the infusion. However, further and more specific studies are needed to clarify the rationale for these choices.
There are several limitations to our study. The main one is that we used a questionnaire developed by our team specifically for this study, and thus it has not been previously validated. The questionnaire was distributed by email and filled out online, which resulted in a limited response rate and thus a limited generalizability of the results. There was also a geographical bias in the distribution of respondents according to the autonomous region where they practiced, with a disproportionate predominance of responses from the Valencian Community, Madrid and Castilla La Mancha. Second, a significant bias that is difficult to avoid in studies of this nature is voluntary response bias, by which professionals who have an interest in the subject and who may have more updated knowledge on it are more likely to participate, thus skewing the distribution towards this group and altering the results, which consequently do not reflect the actual status quo. The third limitation is that whatever respondents reported was the customary clinical practice may not have been a reliable reflection of reality, as sometimes professionals answer according to what they believe should be done, rather than reporting what is done in actual practice.30 Another aspect to consider is that our study took place 14 years after Moritz et al. first proposed the use of isotonic fluids for maintenance,4 and 11 after the publication of the first study that analysed the prescription of MIVFT in the field of paediatrics.14 However, this fact, rather than devaluing our study, should be considered a reason for concern, as our findings suggest that there are still clinicians in Spain that prescribe MIVFT schemes that do not meet the needs of individual patients based on the best available evidence.
We ought to highlight the detail that our survey targeted paediatricians exclusively, since we did not find any other study on this subject in the literature that focused specifically on this medical specialty. Our study is also the largest one based on the number of responses obtained.14–19 Furthermore, we analysed additional aspects MIVFT that had not been investigated to date, such as the addition of potassium or calcium to fluids used for maintenance.
More than 1/4 of Spanish paediatricians continue to prescribe hypotonic fluids for MIVFT. We found several factors that may be associated to the variability exhibited by surveyed paediatricians in the application of scientific evidence to care delivery. Studies like the one presented here reflect the slow pace at which scientific evidence is translated to clinical practice.31 The ability to develop clinical practice guidelines that synthesise knowledge in order to convey and disseminate it effectively is what makes our health organizations institutions that offer high-quality and safe services to patients.32,33
Conflicts of interestThe authors have no conflicts of interest to declare.
We thank all of our colleagues that expressed their interest in the project by participating in the survey.
Also, we once again thank Rosa J. Bertolín Bernades, as this work would not have been possible without her.
Please cite this article as: Rius Peris JM, Rivas-Juesas C, Maraña Pérez AI, Piñeiro Pérez R, Modesto i Alapont V, Miranda Mallea J, et al. Uso de sueros hipotónicos en la prescripción de la fluidoterapia intravenosa de mantenimiento. An Pediatr (Barc). 2019;91:158–165. https://doi.org/10.1016/j.anpedi.2018.10.016