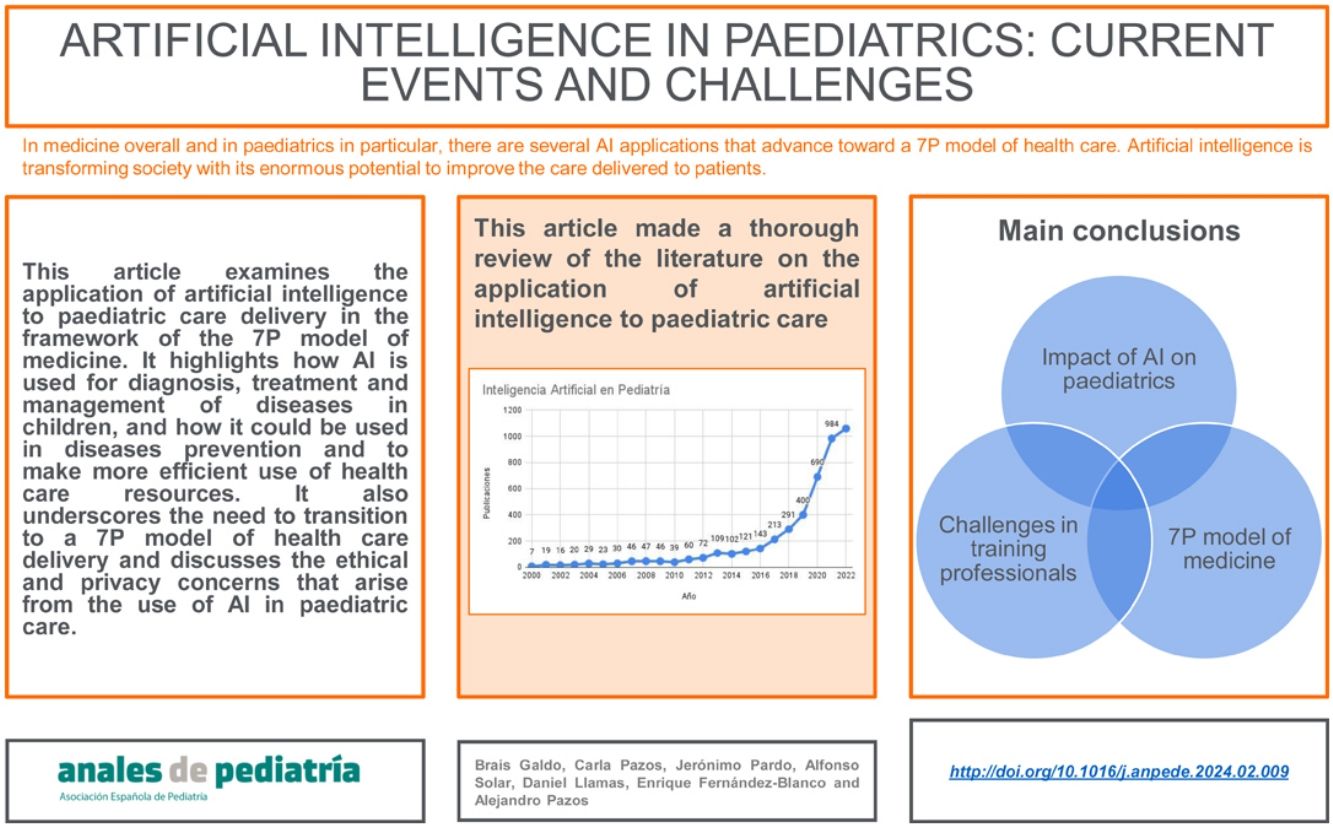
This article examines the use of artificial intelligence (AI) in the field of paediatric care within the framework of the 7P medicine model (Predictive, Preventive, Personalized, Precise, Participatory, Peripheral and Polyprofessional). It highlights various applications of AI in the diagnosis, treatment and management of paediatric diseases as well as the role of AI in prevention and in the efficient management of health care resources and the resulting impact on the sustainability of public health systems. Successful cases of the application of AI in the paediatric care setting are presented, placing emphasis on the need to move towards a 7P health care model. Artificial intelligence is revolutionizing society at large and has a great potential for significantly improving paediatric care.
Se examina el uso de la inteligencia artificial (IA) en el campo de la atención a la salud pediátrica dentro del marco de la "Medicina de las 7P" (Predictiva, Preventiva, Personalizada, Precisa, Participativa, Periférica y Poliprofesional). Se destacan diversas aplicaciones de la IA en el diagnóstico, el tratamiento y el control de enfermedades pediátricas, así como su papel en la prevención y en la gestión eficiente de los recursos médicos con su repercusión en la sostenibilidad de los sistemas públicos de salud. Se presentan casos de éxito de la aplicación de la IA en el ámbito pediátrico y se hace un gran énfasis en la necesidad de caminar hacia la Medicina de las 7P. La IA está revolucionando la sociedad en general ofreciendo un gran potencial para mejorar significativamente el cuidado de la salud en pediatría.
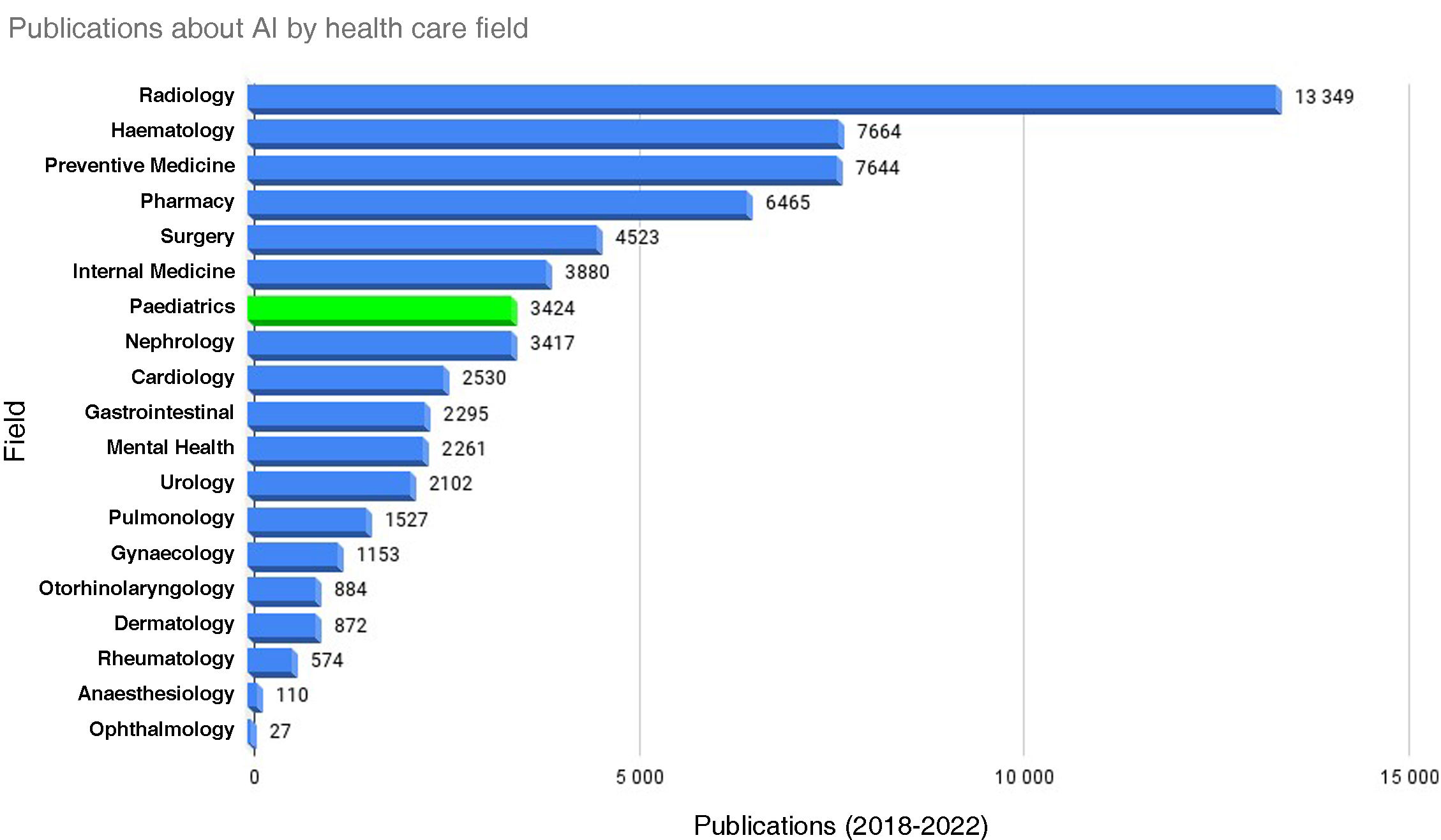
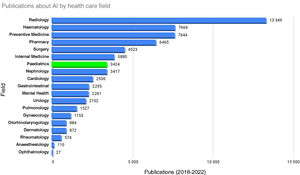
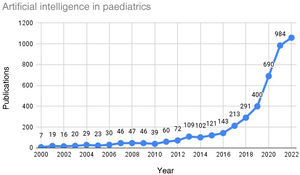
Artificial intelligence (AI) has emerged as one of the most disruptive technologies since the industrial revolution as a main driver in what has come to be known as the “information society”. Its application is changing the way of interacting in personal and business relationships in every sector, making vast advances possible. One of the fields on which AI is having a particularly important impact is health care, and paediatric care in particular. As can be seen in Fig. 1, paediatrics is one of the medical specialities in which the most research and development and innovation (R&D&i) projects have been carried out so far.
The aim of AI is the implementation of artificial systems behaving in such a way, should the same behaviour be exhibited by a human, would be considered intelligent. Its development has a strong biological inspiration. Among the key sources of inspiration are the neuron theory developed by Santiago Ramón y Cajal1 and Hebbian learning theory developed by Donald Hebb,2 which contemplated synaptic changes, so that acquired learning would reside in the distribution of connections between the processing elements. Some of the pioneers from a technological standpoint were Babbage and Lovelace,3 who built the first analytical engine, Turing4 with the development of the Turing machine and von Neumann5 with computer architecture. They were among the first individuals to ever consider the possibility of machines being able to exhibit intelligent behaviour. The advent of AI, as it is understood today, can be traced back to three publications from 1943 in the field of cybernetics.6 The first one considered the possibility of machines having teleological behaviour and of giving them objectives,7 the second one established the capacity of abstraction of machines8 and the third proposed the notion of an artificial neuron as a simplified functional model of the biological neuron.9 Artificial intelligence as was not formally conceptualized until the mid-twentieth century, when John McCarthy, accompanied by a dozen scientists, defined it and coined the term in 1956 in the conclusions of the Dartmouth Summer Research Project.10
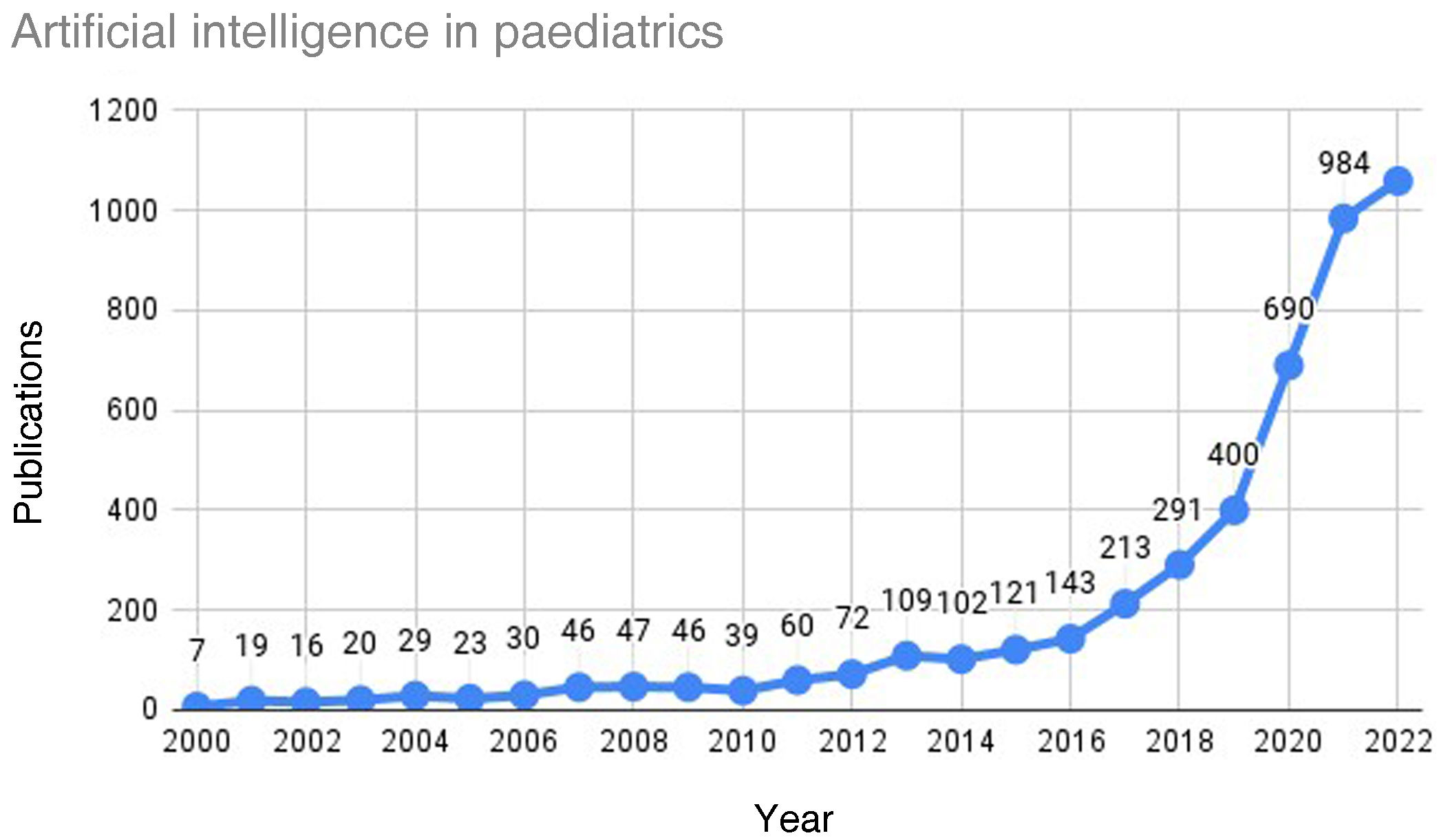
The first applications of AI in medicine hail back to the 1970s: MYCIN11 and CASNET12 were two expert systems developed within the symbolic AI approach. The first commercial applications of AI were introduced in the mid-1960s to reduce noise in telephonic communications with Madaline networks,13 developed within the connectionist AI approach that predominates today thanks to deep learning systems, which offer a potential for learning of a magnitude yet unknown. They offer new perspectives and tools that are complemented with the contributions of health care professionals. As can be seen in Fig. 2, the number of studies in which AI was applied in the field of paediatrics has been increasing exponentially since 2016, a trend that is expected to continue.
Different guidelines are being developed at Stanford University for the safe inclusion of paediatric data in AI-driven medical research, which raises a variety of concerns.14 The aim of these guidelines is to help address the unique complexities presented by children in relation to AI, including consent, explainability and equity. Some of the steps to take moving forward will be the development by consensus of ontologies and standards and the publication of consensus statements by all involved stakeholders.
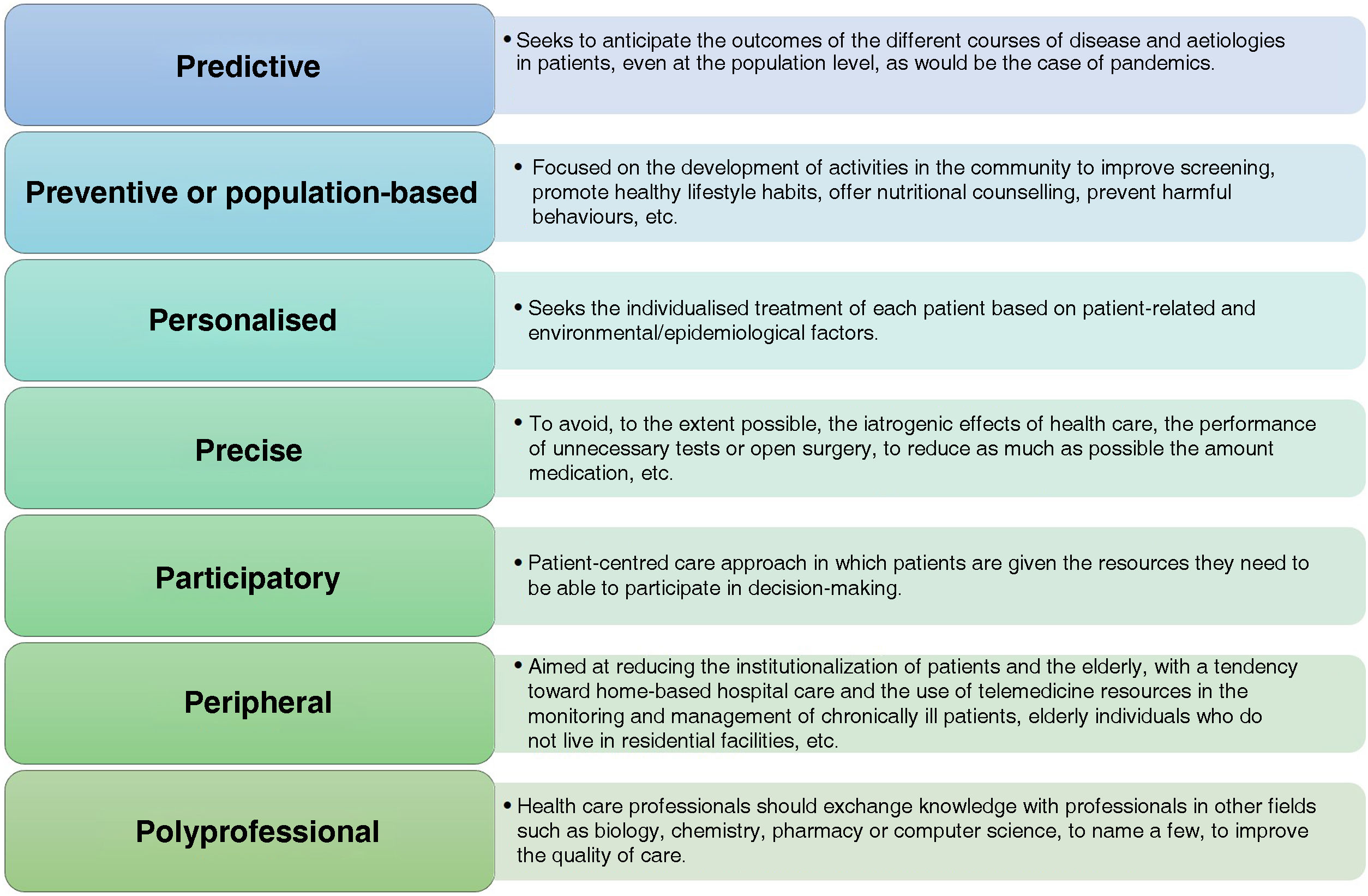
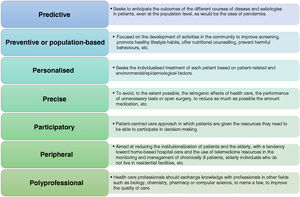
In recent years, it has become increasingly clear that changes need to be made to current health care delivery models. The emerging paradigm, rooted in what Sunarti termed the 4P model of medicine (preventive, personalized, participatory and population-based)15 that we would like to expand to a 7P model of medicine, in which each P covers a specific function, as can be seen in Fig. 3.
The aim of our review article is to cover the most recent advances in AI in the field of paediatrics in the framework of the 7P model of medicine. We will discuss different applications of AI for the diagnosis and treatment of paediatric diseases and analyse their contribution to health care delivery, both present and future, and in the efficient management of health care resources.
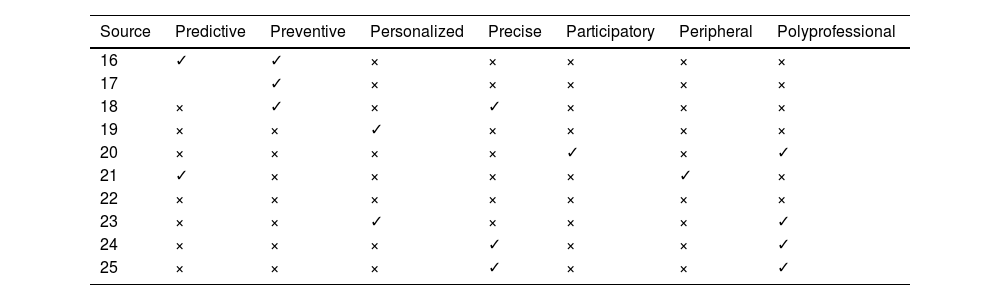
Applications and researchTable 1 presents a summary of the most relevant characteristics of each scientific article analysed in the review. The articles were selected based on their perceived relevance in the context of the proposed 7P model (Figura 3). We took into account different factors, such as the number of citations of the articles, their dates of publication and the degree to which they fit the perspective of the 7P model of medicine, among others.
Areas of the 7P medicine model addressed in the publications included in this review. All areas are interconnected, but one or two of them were most relevant in each of the articles. To illustrate this, we used the × symbol to indicate a weaker fit and the ✓ symbol to indicate a greater fit of the article with the given area.
In recent years, numerous AI applications have been developed in the field of paediatrics. Some of the most relevant advances focus on the early detection of disease in children, for instance, autism spectrum disorder.16,17 These applications use magnetic resonance imaging data. The data are processed by a deep neural network18 and finally, a support vector machine19 estimates with a high reliability the probability of the patient developing autism. The model was validated with 179 patterns. The validation study found a precision of 94%, a specificity of 88% and a sensitivity of 95%.
Another important application is the detection of neonatal jaundice. A system developed by Aydin et al.20 used advanced image processing and machine learning techniques to attempt to detect jaundice and estimate bilirubin levels. They compared the results of the system with those of conventional blood tests and found a success rate of 85%. The data for the system can be captured with a smart phone using a colour calibration card placed on the abdomen of the patient.
Imaging is another of the fields in which AI tools are being used in paediatric care (robotic surgery and diagnostic imaging). The latest version of the BoneXpert software was recently launch for the routine evaluation of bone age in paediatric endocrinology.21
There are diseases in which the susceptibility of the pathogen to the different antimicrobials, as well as its early determination, are of utmost importance. This is the case of severe bacterial infections (SBIs) in febrile infants. In a study focused on this particular aspect, Ramgopal et al.22 developed a random forest model t with very promising results in terms of both sensitivity (99%) and specificity (75%), so its application could achieve a reduction in the number of unnecessary procedures.
In 2013, Ivy proposed an intelligent system for the detection of paediatric pulmonary hypertension. The article by Patel et al.23 presents an exhaustive data collection process that takes into account various demographic and clinical factors. These models can improve the use of resources and the triage of paediatric patients. The best one was a gradient boosting model that achieved an area under the curve (AUC) in the receiver operating characteristic curve analysis of 0.85 in the prediction of the need of hospital admission.24
There are also publications of a more general nature, like the one by Liang et al.,25 who attempted to detect a broad range of diseases using methods like deep neural networks and logistic regression classifiers. The data, information and knowledge processed by the developed system are heterogeneous and comes from diverse sources, ranging from electronic health records to physical examination or laboratory reports. The authors found that the system achieved a precision of 0.95 in the diagnosis of upper respiratory tract infection and sinusitis and of 0.97 in the diagnosis of acute asthma exacerbations, among other diseases.
Different AI tools have also been developed to carry out behavioural assessments. We ought to highlight the cases described by Guthold et al.,26 who found that 80% of adolescents did not achieve the minimum recommended physical activity level. This could change. Tools such as Tess,27 a chatbot used in paediatric care to assess for obesity and prediabetes in children, may be helpful. This tool can offer support and guidance to promote healthy behaviours, including diet and physical activity, through automated chats with users. It also offers evidence-based interventions and responds to the emotions and concerns expressed by users. A study conducted in several universities in the United States28 found that patients were satisfied with its use and were appreciative that this tool could offer support around the clock.
There are also applications to estimate the effect of treatment on a given patient. For instance, Fang et al.29 used machine learning to try to predict the outcome of treatment with orthokeratology in children. In their analysis, they identified factors such as age, lens wearing time, the time spent out of doors or corneal measurements among others. They developed a logistic regression model with least absolute shrinkage and selection operator (LASSO), and the results demonstrated that this model could be useful to ophthalmologists in decision-making and to predict treatment outcomes.
Another relevant publication is the study conducted by Hernandez et al.30 analysing the development and testing of an AI application to automate the treatment planning process for paediatric craniospinal irradiation therapy. This tool uses a deep learning model to generate autocontours and guide planning. The application successfully generated treatment plans for paediatric patients with medulloblastoma. The authors concluded that both the autocontouring model and the autoplanning tool were effective and could be used in the planning of craniospinal irradiation in paediatric patients.
Furthermore, as reflected by the article published by Shah et al.,31 the generation of natural language models (large language models [LLMs] using generative networks like GPT) is one of the most important fields of AI at the moment. Some studies have assessed the ability of different large language models to follow natural language for electronic health records.32 The authors found that GPT-4 based models performed better than Vicuña or MPT-7B-Instruct models. They also assessed the correlation between the automated metrics and human classifications, and found the strongest correlation with COMET. The considerable volume of language resources of a medical nature makes the development of these models possible.
Last of all, we ought to highlight the research focused on the length of stay, which can help with planning. For instance, Elrod et al.33 sought to estimate the length of stay of paediatric burn patients. These systems can be very useful in assessing the condition of the patient and offering outpatient treatment. They are not only beneficial in terms of care quality, but also for the management of health care resources. Predicting length of stay allows an estimation of when a bed will become available to offer to a different patient, which optimises the use of this resource. This research team in particular developed a random forest model that yielded improved results compared to the heuristic empirical rule. The model was consistent for patients with burns involving up to 20% of the total body surface area.
In conclusion, as can be surmised from the range of applications reviewed in this article, AI tools developed to improve health care are in line with the 7P model of medicine. Therefore, their use will contribute to improve care delivery by health care professionals and the sustainability of public health systems.
DiscussionIn this review we presented multiple examples of current research relevant for the field of paediatrics. These works are applicable to different care delivery areas of the 7P model of medicine. The overall aim is to improve health care quality and the sustainability of public health care systems.
Although there is a broad range of paediatric areas in which research is being carried out, there is also a large number that have yet to be studied with an AI approach. Some of the reasons for this may be the subjectivity of observations or the impossibility to obtain a large enough number of examples to train the AI system. This could be the case of sleep disorders, which affect a large proportion of the population34 and cause numerous disorders in subsequent stages of development, as demonstrated by the studies by d Kapoor et al.35 or Voci et al.36 According to the American Academy of Sleep Medicine (AASM), the use of AI in this field could be very beneficial.37 Artificial intelligence has the potential to improve the efficiency and precision of sleep scores and afford a greater understanding of sleep disorders. The AASM places particular emphasis on the fact that these tools should not under any circumstances replace the specialist, but rather guide the specialist in decision-making.
Novel Gemini-based AI tools24,38 could be very useful for diagnosis of low-prevalence syndromes associated with facial dysmorphic features. More than 2000 such syndromes have been described, and more often than not their detection and classification require assessment by experts in dysmorphia. The classification of these syndromes based on geometric morphometrics is observer-dependent and requires considerable time, and while there are some automated tools to locate these reference points, their application has thus far been limited to the adult population, analysing the photographic database of patients with Treacher Collins syndrome (mandibulofacial dysostosis) in Hospital Necker-Enfants Malades in Paris, defined a process to create automatic annotation models adapted to faces with congenital anomalies, a foundation required to be able to do research on dysmorphia.
One of the limitations that will inevitably arise in the development of AI in the field of paediatrics will be the limited amount of data derived from the small populations of ill children and the intrinsic challenges involved in the management of these patients’ sensitive health care data.
Type 1 diabetes is one of the diseases for which it could be useful to develop AI applications. Today, many paediatric patients with diabetes carry continuous glucose monitors that contribute a large amount of data, charts and trends that could be useful to clinicians and family members, who are often reluctant to make adjustments to prescribed treatment before visiting the doctor out of fear of making mistakes.
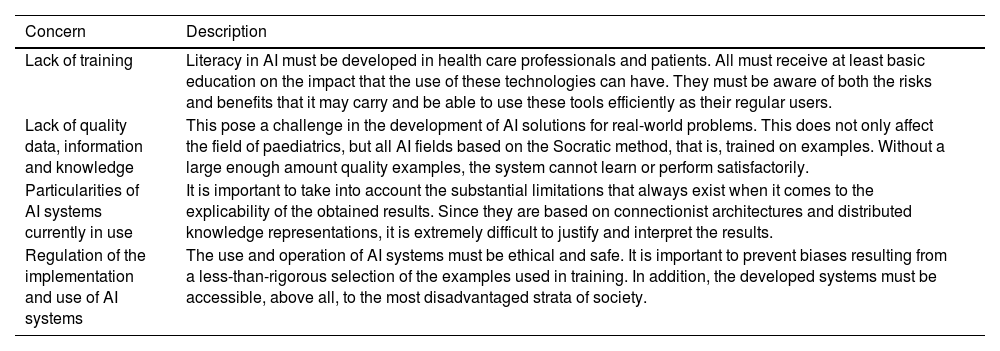
Taking into account what has been discussed this far, we must highlight the concerns discussed in Table 2.
Concerns to consider and address in the application of AI knowledge and methods.
| Concern | Description |
|---|---|
| Lack of training | Literacy in AI must be developed in health care professionals and patients. All must receive at least basic education on the impact that the use of these technologies can have. They must be aware of both the risks and benefits that it may carry and be able to use these tools efficiently as their regular users. |
| Lack of quality data, information and knowledge | This pose a challenge in the development of AI solutions for real-world problems. This does not only affect the field of paediatrics, but all AI fields based on the Socratic method, that is, trained on examples. Without a large enough amount quality examples, the system cannot learn or perform satisfactorily. |
| Particularities of AI systems currently in use | It is important to take into account the substantial limitations that always exist when it comes to the explicability of the obtained results. Since they are based on connectionist architectures and distributed knowledge representations, it is extremely difficult to justify and interpret the results. |
| Regulation of the implementation and use of AI systems | The use and operation of AI systems must be ethical and safe. It is important to prevent biases resulting from a less-than-rigorous selection of the examples used in training. In addition, the developed systems must be accessible, above all, to the most disadvantaged strata of society. |
If these four concerns are adequately addressed, there will be significant progress not only in the field of paediatrics, but also in medicine overall and society at large.
ConclusionArtificial intelligence has a strong presence in the field of paediatrics. It can be useful in different areas ranging from the detection of autism to the prediction of the outcomes of an orthokeratology treatment in in paediatric patients.
It is also clear that AI is closely related to the new paradigm of health care delivery, the 7P model of medicine, in each and every one of its branches.
Artificial intelligence is advancing exponentially. Right now, it is possible to interact with a chatbot, for example, Tess,27 that can offer support and assess different aspects such as childhood obesity or prediabetes. This is of vital importance, especially for patients who, due to their particular circumstances, cannot immediately travel to a hospital or show to a telephonic visit during business hours.
Final decisions must always rest with the clinician, whereas AI is a tool meant to support decision-making, supporting the clinician and the patients throughout care delivery, and thus facilitating progress in the 7P medicine model.
Lastly, we ought to comment on the remarkable number and diverse nature of the advances that have been made in AI within the field of paediatrics. Research has given rise to numerous possibilities that could be implemented in clinical practice and improve both the quality of patient care and the quality of work for health care providers. Lastly, we ought to underscore the need to continue advancing to offer new solutions and improve existing ones. Some examples of upcoming advances that will revolutionize these technologies in the future are the capability of incorporating images to large language models (LLMs) and generative AI applications (GPT, Gemini…).
Improvements in the following 4 aspects are considered among the goals that we should strive for:
- 1
Training of professionals and users on these technologies.
- 2
Quality of the examples in datasets used to train AI models.
- 3
Explainability of results.
- 4
Regulation of AI systems use.
The authors declare that they have no conflict of interest.