Point-of-care ultrasound (POCUS), also known as bedside ultrasound, refers to the use of ultrasound in the clinical assessment of the patient at the point of care. It is unquestionably useful in primary care by supplementing the assessment of the patient in real time, helping answer specific questions as they arise during the examination. This allows establishing a better and more accurate working diagnosis and quicker and more appropriate decision-making.
For primary care paediatricians, contrary to what may be expected from the implementation of an additional technique, the use of ultrasound streamlines care delivery by improving the accuracy of diagnosis and preventing the performance of other diagnostic tests, which is directly beneficial to the patient. Furthermore, when the paediatrician is adequately trained its use does not significantly increase the duration of the visit.
The application of POCUS in emergency and intensive care settings is one of the strongest examples of how this technique has revolutionised medical care by providing diagnostic information in situations that require immediate decisions. This tool, which is harmless, portable and cost-effective, allows the visualization of abnormalities in real time at the point of care and does not require moving the patient.
Lung ultrasound is probably the most important application of POCUS. It also offers the advantage of a rapid learning curve.1 There are 2 aspects that contribute to this. One is that it does not require a thorough knowledge of anatomy, as knowing the location of the lungs and the structures of the chest wall is all that is needed. The other is that this assessment is based on the analysis of sonographic artifacts and/or the presence or absence of abnormal changes in these features to draw conclusions.
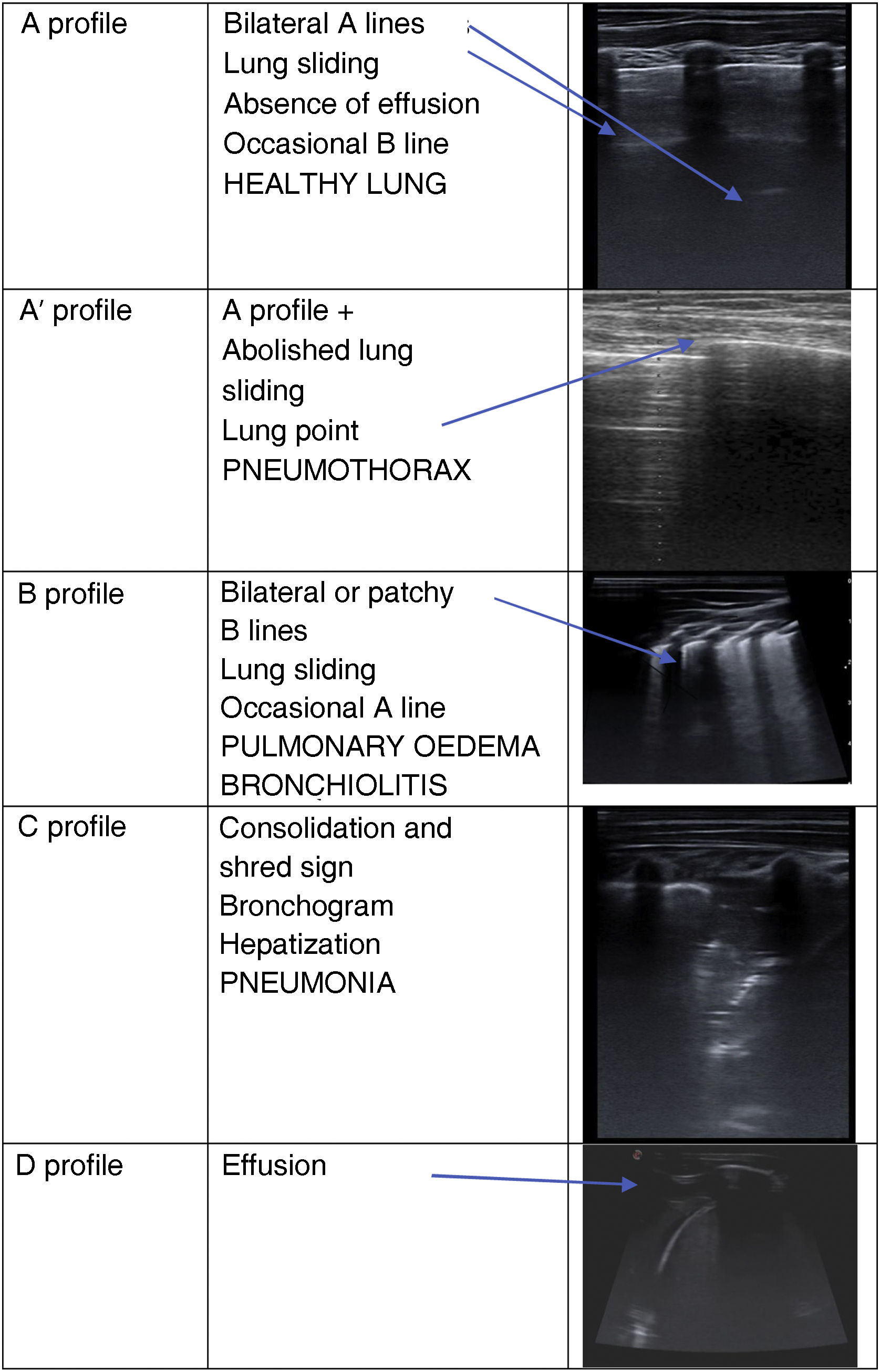
The lung ultrasound is based in the interpretation of a reverberation artifact, known as A lines, produced by the differences in acoustic impedance between air and body tissues. When the normal appearance is replaced by other sonographic features (because the gas in the lungs has been replaced by liquid or solid substances that allow transmission of sound), this is interpreted as the presence of disease. Thus, it is possible to observe different sonographic patterns, such as A lines (normal), B lines (interstitial oedema), consolidation or effusion, in addition to the presence or absence of lung sliding (movement between the pleural layers). This is an oversimplification of what lung ultrasound is, but it serves as a starting point for its study2 (Fig. 1).
Lung ultrasound patterns based on the methodology described by Lichtenstein D. (BLUE-protocol and FALLS-protocol: Two applications of lung ultrasound in the critically ill. Chest. 2015; 147: 1659-1670) and the most frequent paediatric diseases associated with these patterns with the corresponding images.
Whenever the use of lung ultrasound is considered, it must be approached in the framework of a given clinical presentation, or else it will be of limited value. In a patient with bronchiolitis, the ultrasound may show a patchy B-line pattern or a normal pattern, but in the future it may be possible to establish prognostic factors with the help of this technique. In a child with heart disease and breathing difficulty, it may help identify the cause of the latter.
If what is found is consolidation, the clinician needs to go back to the patient and consider whether, given the clinical manifestations, it may be a case of viral pneumonia, in which it is possible to find some B lines and subpleural consolidations (often multiple and of limited depth), or whether the consolidation is or not accompanied by effusion. In any case, the age, presence of fever and time from onset need to be taken into account to determine whether the patient has typical or atypical pneumonia. The one exception may be pneumothorax, in which sonography has a specificity near 100% if the lung point is present.
The history of lung sonography started with Daniel Lichtenstein, an intensive care specialist in France who described the first sonographic images in 1997.3 Since then, and especially in recent years, the number of ultrasound assessment protocols and the knowledge on the practical application of lung sonography have grown continuously, which promises a bright future for this diagnostic technique. But there are still plenty of challenges to undertake, such as the prognostic significance of the different images.
It may be worth considering how many ultrasound examinations need to be performed to achieve sufficient skill in lung ultrasound examinations. The number may vary depending on several factors, like the baseline skill of the physician, the quality of the training received, the frequency of practice and the exposure to different clinical scenarios. According to various authors, as many as 50–100 supervised examinations may be necessary, followed by regular practice.4 On the other hand, training in lung ultrasound improves diagnostic skills and is associated with a high diagnostic accuracy in the evaluation of lung diseases.
Numerous studies have demonstrated the high diagnostic accuracy of POCUS in a variety of medical conditions. The lung ultrasound offers a sensitivity of 94% and a specificity of 96% for detection of pleural effusion compared to the chest X-ray.4 When it comes to pneumothorax, POCUS has demonstrated a similar or superior accuracy compared to plain radiography. The specificity reaches 100% when the lung point is identified.5 And in the diagnosis of pneumonia in children, a sensitivity of 95% and a specificity of 96% have been reported.6,7 We must keep in mind that the few cases of pneumonia in which the disease does not reach the pleura cannot be detected by ultrasound.
The accuracy of the lung ultrasound increases with the experience of the provider that performs it. Therefore, we need to start considering whether we could not obtain more information by performing an ultrasound scan rather than a radiograph. In addition, the lung ultrasound is faster (in experienced hands, the assessment can be completed and a diagnosis made in 5 min), establishes the exact location and dimension of the lesion, does not involve exposure to radiation and can guide interventional procedures.
Another question we must ask from the collective of Spanish paediatricians is whether we are using the lung ultrasound in everyday practice. Although there is no evidence from actual studies, there are some data obtained through surveys of paediatricians in Spain. In 2018, in a sample of 273 respondents, while 47% reported having been trained in the technique, only 18% used it in their everyday practice. (https://www.congresoaep.org/static/upload/ow28/events/ev190/Site/files/Comunicaciones-y-Posteres-2018) In another survey that is scheduled for publication this year, of the 212 surveyed paediatricians that reported access to an ultrasound machine, only 28% stated they would use it if they suspected pneumonia. Given the participation bias inherent in such surveys, we may conclude that the use of ultrasound, and specifically lung ultrasound, despite its value, continues to be infrequent.
To conclude, many other ultrasound examinations can be directly useful in the primary care setting. Among others, the ultrasound skin imaging, which can offer greater accuracy in diagnosis and prevent the performance of some biopsies. Or the musculoskeletal ultrasound, chiefly due to the easy diagnosis of nondisplaced fractures without exposure to ionising radiation.
In conclusion, given the high yield, ease of use and increasing availability of this technique, we must strive to ensure that it is integrated in everyday paediatric practice, which requires the training of paediatricians, whether hospital-based or in primary care, and, needless to say, its inclusion in medical residency curricula. This, combined with the increasing availability of ultrasound machines and the growing knowledge in this technique, will allow us to make the most of it in a few years.
Conflicts of interestThe authors have no conflicts of interest to declare.