Orthopaedic treatment of developmental dysplasia of the hip (DDH) has a high success rate in cases that are diagnosed early. However, the outcomes of these patients are not really known when they are subsequently diagnosed with some type of cerebral impairment.
Materials and methodsA retrospective observational study was conducted on cases of DDH with a poor outcome after orthopaedic treatment, being unknown if they had any type of psychomotor disorder. The patients were clinically and radiologically assessed, and afterwards received neurological valuation by the Child Neurology Unit.
ResultsOf the 325 cases of DDH diagnosed in 293 patients, 10 patients (3%) with 16 hips with DDH were diagnosed of any cerebral impairment. All of them were initially treated orthopedically. Clinical and radiologically evolution was succesful only in 4 cases (25%) being necessary any surgical procedure in the remaining 12 cases. After surgical treatment we got an improvement in the Acetabular Index (p=0.005) and Reimers Extrusion Index (p=0.042). Neck-shaft angle and Wiberg CE angle also improved but this difference was not statically significant. Cerebral impairment was diagnosed at 2.5 years of age and the begining of walking was delayed at 2.4 years of age.
ConclusionsCerebral impairment can lead to an unfavourable outcome in the treatment of DDH, with the relative risk of a poor outcome being 7.2 times higher in these patients.
An unfavourable outcome with conventional treatment of DDH must make us suspect the presence of some type of neurological disorder, particularly if there is a delay in walking.
El tratamiento ortopédico de la displasia del desarrollo de la cadera (DDC) presenta un alto porcentaje de éxito en casos diagnosticados precozmente o en los primeros meses de vida. Sin embargo, se desconoce qué resultados presentan estos pacientes cuando posteriormente son diagnosticados de un trastorno psicomotor.
Material y métodosSe realiza un estudio observacional retrospectivo de los casos de DDC con mala evolución tras tratamiento ortopédico, desconociéndose si presentaban algún tipo de trastorno psicomotor. Los pacientes fueron valorados clínica y radiológicamente, y por la Unidad de Neurología Infantil.
ResultadosDe los 325 casos de DDC diagnosticados en 293 pacientes, 10 pacientes (3%) con 16 caderas con DDC fueron diagnosticados de algún tipo de trastorno psicomotor. Todos los casos inicialmente fueron tratados ortopédicamente. La evolución tanto clínica como radiológica en estos casos fue favorable sOlo en 4 (25%). En los 12 restantes se indicó quirúrgica para su resolución (75%). Hubo mejoría tras tratamiento quirúrgico en el índice acetabular (p = 0,005) y en el índice de extrusión de Reimers (p = 0,042). El ángulo cÉrvico-diafisario y el ángulo CE de Wiberg también mejoraron, pero su diferencia no fue estadísticamente significativa. El diagnóstico del trastorno psicomotor se realizó a los 2,5 años de edad. El inicio de la deambulación de estos pacientes estaba retrasado, iniciándose a los 2,4 años.
ConclusionesEl trastorno psicomotor puede condicionar una tórpida evolución en el tratamiento conservador de la DDC; el riesgo relativo de presentar un mal resultado es 7.2 veces mayor en estos pacientes.
Ante una mala respuesta al tratamiento convencional de una DDC, debe sospecharse la existencia de un posible trastorno neurológico de base, especialmente si hay un retraso en la deambulación.
The treatment of developmental dysplasia of the hip (DDH) has been highly standardised for many years, but its failure can lead to the development of major sequelae. At present, the routine performance of neonatal examinations combined with the knowledge of risk factors and the use of ultrasonography allow its early diagnosis, which is crucial for the early initiation of treatment in order to achieve the best possible outcomes. Outcomes are satisfactory in a high percentage of patients (between 80% and 92% of cases) irrespective of the method chosen for its treatment (Pavlik harness, abduction brace, etc.), and depending on the degree of hip stability.1,2
Avascular necrosis is possibly a complication that develops most frequently during treatment of hip dysplasia, although its incidence has decreased significantly (2.38% of cases treated with conservative approaches).2 The developed complications are usually related to the type of treatment used or the difficulty of hip stabilisation. Many studies in the literature have found factors that influence the prognosis of conservative treatment and the development of complications, such as delayed diagnosis, bilaterality, hip luxation versus preluxation, teratologic dislocations, adduction contracture of the hip or the initial position of the femoral head.3–7 However, few studies in the literature have analysed the impact of comorbidities such as psychomotor delays, behavioural disorders or cerebral palsy on DDH.
The aim of this study was to analyse the cases of DDH that did not respond well to conservative treatment and the possible influence of psychomotor disorders, which could be risk factors contributing to these poor outcomes. To do so, we conducted a retrospective study of patients that received a diagnosis of psychomotor disorder when treatment for DDH had already started.
Materials and methodsWe conducted a retrospective observational study of the cases of DDH treated in our hospital between January 2002 and December 2012 (325 cases of DDH in 293 patients). Orthopaedic treatment failed in 44 of the cases under study (13.5%), with failure defined as not achieving concentric reduction of the hip or the persistence of a residual hip dysplasia with an acetabular index (AI) greater than 30° that did not resolve after the patient began walking. Psychomotor delays were detected in 10 of these patients (16 hips), months after treatment of DDH had been initiated.
Of the total cases of DDH that we found, 309 (283 patients) were free of psychomotor comorbidity, and the initial orthopaedic treatment failed in 34 cases (10%).
Of the 16 cases (10 patients) with a psychomotor comorbidity, 75% (12 cases) were refractory to treatment, while the outcome of conservative treatment of DDH was successful in the remaining 25% (4 cases).
We collected data for the following variables for the 10 patients included in the analysis: sex, side involved, gestational age at birth, type of delivery (caesarean or vaginal), birth weight, age at diagnosis of DDH, type of treatment received, and complications. These patients were evaluated on the basis of clinical features and/or magnetic resonance imaging by the Paediatric Neurology Unit to confirm the presence of brain lesions or behavioural disorders. We collected data on the age at diagnosis, neurologic disease, ability to walk, and age at which patients began walking.
The radiologic followup consisted of anteroposterior pelvis radiographs and axial hip radiographs. In cases treated with spica casts or with a high degree of hip instability, the followup also included a computed axial tomography scan in the early postoperative period to confirm the correct reduction of the dislocated hip. The radiographic parameters that were documented were the location of the ossification centre in the femoral head based on the Ombredanne quadrants (Fig. 1) and the AI before and after orthopaedic treatment. These values were measured in digital radiographs using the Centricity application developed by General Electrics.
We analysed the data using SPSS version 18. We conducted a descriptive study, expressing quantitative variables as medians and qualitative variables as absolute frequencies and percentages (%). We determined the statistical significance of qualitative variables by means of the chi square test.
ResultsOf the 325 cases treated conservatively in our hospital, 44 had poor outcomes (failure to achieve concentric reduction of the hip or evidence of residual dysplasia with an AI greater than 30°) on follow-up imaging tests that did not resolve fully after the patient began walking). Psychomotor disorders were diagnosed in 16 cases of DDH (36%) that corresponded to 10 patients.
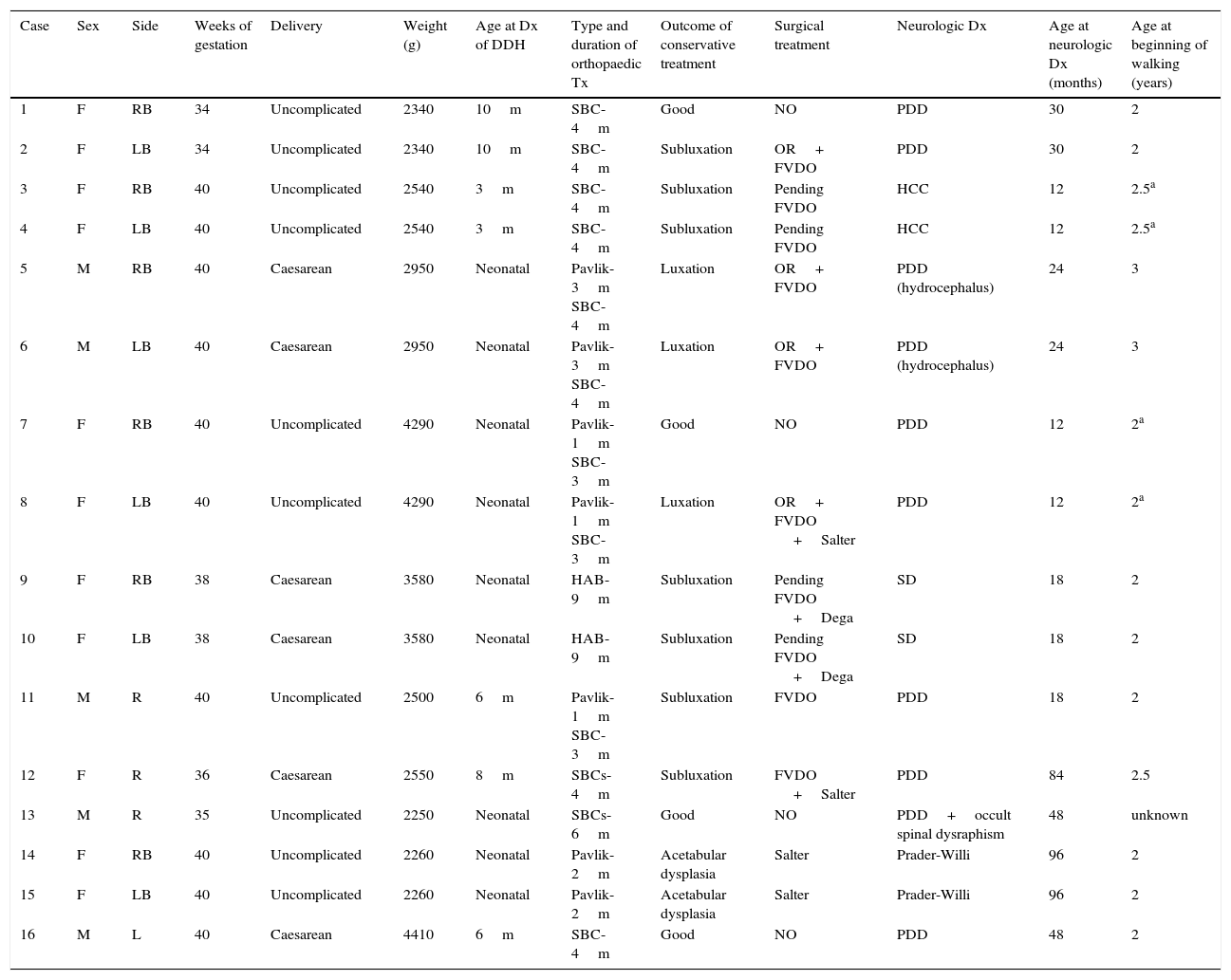
Sixty percent of the patients (6 cases) were female, and 40% male. As for laterality, six patients had bilateral involvement (60% of patients), three had unilateral involvement of the right hip (30% of patients) and one had unilateral involvement of the left hip (10% of patients). Four patients (40%) were delivered by caesarean section, three due to breech presentation and one due to foetal distress. Three patients (30%) were born preterm (before 38 weeks’ gestation). The mean birth weight for the 10 patients was 2967g (range, 2250–4410) (Table 1).
Summary of cases.
| Case | Sex | Side | Weeks of gestation | Delivery | Weight (g) | Age at Dx of DDH | Type and duration of orthopaedic Tx | Outcome of conservative treatment | Surgical treatment | Neurologic Dx | Age at neurologic Dx (months) | Age at beginning of walking (years) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | F | RB | 34 | Uncomplicated | 2340 | 10m | SBC-4m | Good | NO | PDD | 30 | 2 |
| 2 | F | LB | 34 | Uncomplicated | 2340 | 10m | SBC-4m | Subluxation | OR+ FVDO | PDD | 30 | 2 |
| 3 | F | RB | 40 | Uncomplicated | 2540 | 3m | SBC-4m | Subluxation | Pending FVDO | HCC | 12 | 2.5a |
| 4 | F | LB | 40 | Uncomplicated | 2540 | 3m | SBC-4m | Subluxation | Pending FVDO | HCC | 12 | 2.5a |
| 5 | M | RB | 40 | Caesarean | 2950 | Neonatal | Pavlik-3m SBC-4m | Luxation | OR+ FVDO | PDD (hydrocephalus) | 24 | 3 |
| 6 | M | LB | 40 | Caesarean | 2950 | Neonatal | Pavlik-3m SBC-4m | Luxation | OR+ FVDO | PDD (hydrocephalus) | 24 | 3 |
| 7 | F | RB | 40 | Uncomplicated | 4290 | Neonatal | Pavlik-1m SBC-3m | Good | NO | PDD | 12 | 2a |
| 8 | F | LB | 40 | Uncomplicated | 4290 | Neonatal | Pavlik-1m SBC-3m | Luxation | OR+ FVDO +Salter | PDD | 12 | 2a |
| 9 | F | RB | 38 | Caesarean | 3580 | Neonatal | HAB-9m | Subluxation | Pending FVDO +Dega | SD | 18 | 2 |
| 10 | F | LB | 38 | Caesarean | 3580 | Neonatal | HAB-9m | Subluxation | Pending FVDO +Dega | SD | 18 | 2 |
| 11 | M | R | 40 | Uncomplicated | 2500 | 6m | Pavlik-1m SBC-3m | Subluxation | FVDO | PDD | 18 | 2 |
| 12 | F | R | 36 | Caesarean | 2550 | 8m | SBCs-4m | Subluxation | FVDO +Salter | PDD | 84 | 2.5 |
| 13 | M | R | 35 | Uncomplicated | 2250 | Neonatal | SBCs-6m | Good | NO | PDD+occult spinal dysraphism | 48 | unknown |
| 14 | F | RB | 40 | Uncomplicated | 2260 | Neonatal | Pavlik-2m | Acetabular dysplasia | Salter | Prader-Willi | 96 | 2 |
| 15 | F | LB | 40 | Uncomplicated | 2260 | Neonatal | Pavlik-2m | Acetabular dysplasia | Salter | Prader-Willi | 96 | 2 |
| 16 | M | L | 40 | Caesarean | 4410 | 6m | SBC-4m | Good | NO | PDD | 48 | 2 |
DDH, developmental hip dysplasia; Dx, diagnosis; F, female; FVDO, femoral varus derotation osteotomy; HAB, hip abduction brace; HCC, hypoplasia of the corpus callosum; L, left; LB, left bilateral; M, male; m, months; OR, open reduction; PDD, pervasive developmental disorder; R, right; RB, right bilateral; SBC, spica body cast; SD, spastic diplegia; Tx, treatment.
Developmental dysplasia of the hip was detected during the physical examination of the newborn in five patients, and late in the other five (at ages 6–10 months), although it was detected before the diagnosis of psychomotor disorder in all. The mean age at diagnosis of DDH was 3.3 months (range, 0–10 months).
Table 1 shows the treatments received by each patient with their duration and outcomes. Conservative treatment was only successful in four cases, while in the remaining cases, the persistence of luxation or subluxation or an elevated AI called for surgical intervention (surgery has already been performed in eight of these cases).
The changes in the documented radiologic parameters showed improvement after treatment, with the average AI changing 38.2–30.6° (IAs were greater than 30° in seven cases).
As for the position of the centres of ossification before treatment, they were located in the lower inner quadrant in four cases, in the lower outer quadrant in eight cases, and in the upper outer quadrant in four cases. After conservative treatment, the position of the centres had shifted, with ten of them located in the lower inner quadrant and the remaining six in the lower outer quadrant. The hips that were positioned normally at the outset were treated due to the presence of marked acetabular dysplasia, with a mean AI of 38°, as they were not likely to correct spontaneously when the patient started walking.
The complications that developed during treatment included a femoral head fracture and three cases of avascular necrosis of the femoral head (18%), two of which were partial (of which one resulted in a residual coxa magna deformity) and one of which involved the entire epiphysis.
The mean age at which these patients started ambulating was 2–3 years, and eight of them succeeded in achieving independent walking (four patients are unable to walk unassisted). The patient with hypoplasia of the corpus callosum has achieved an assisted gait with double support, as has one of the patients with a pervasive developmental disorder, which in this case was secondary to hydrocephalus.
The evaluation in the Unit of Paediatric Neurology took place at a mean age of 2.5 years (range, 0.7–7 years). Table 1 presents the aetiological diagnoses of the patients. Pervasive developmental disorders were diagnosed in 80%.
In our series, poor outcomes occurred in 75% of patients with DDH and psychomotor comorbidities, compared to 10% of patients in whom such a comorbidity was not detected. The relative risk of a poor outcome was 7.2 times higher in patients with psychomotor disorders, and the difference was statistically significant (p<0.0001).
DiscussionAppropriate and early treatment of DDH succeeds in resolving 85% of cases with conservative approaches,1,2 but certain circumstances may be associated with poor outcomes. There are articles in the literature that refer to factors that may contribute to poor outcomes, such as hip luxation compared to subluxation, a delay in diagnosis or initiation of treatment, and others.3–7 However, few studies have mentioned psychomotor disorders as potential risk factors for poor outcomes of orthopaedic treatment.
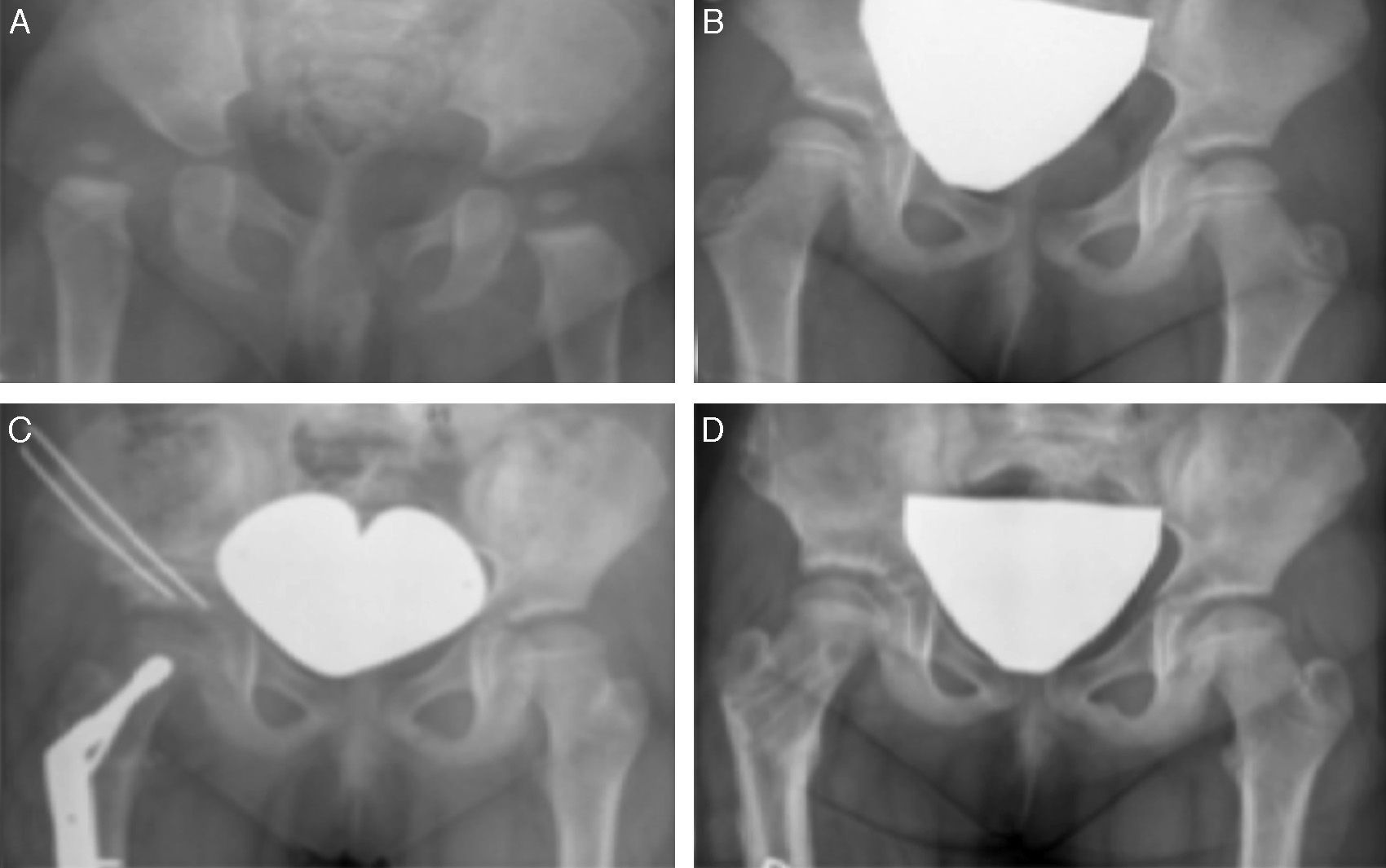
As we mentioned above, 16 (36%) of the total hips that were refractory to conservative orthopaedic treatment corresponded to patients with psychomotor disorders that had been detected after treatment initiation. In 75% of these cases (12 hips), there was residual dysplasia or hip migration after completion of conservative treatment that was an indication for surgery (Fig. 2). In our series, this amounted to a probability of poor outcome in patients with DDH and a psychomotor disorder of 75% compared to 10% in patients that did not have this comorbidity, with a relative risk that was 7.2 times greater, a difference that was statistically significant (p<0.0001). Despite the small number of cases, these findings seem to support the hypothesis that the psychomotor disorders observed in our study, which did not involve significant abnormalities in muscle tone that would hinder the restoration of the optimal biomechanical conditions to achieve adequate joint stability (as observed in patients with cerebral palsy or flaccid paralysis),8,9 contribute to the poor prognosis for treatment of DDH.
Clinical case number 12. (A) Diagnosis of DDH at age 8 months treated conservatively with a series of spica casts. (B) Outcome of conservative orthopaedic treatment at age 6 years, with acetabular dysplasia, a coxa valga deformity, and a disrupted Shenton's line. (C) Surgical treatment with a Salter osteotomy, combining transplantation of an allograft from a tissue bank with a femoral varus derotation osteotomy. (D) Final outcome at age 8 years.
It is important to differentiate between DDH and neuromuscular dislocation of the hip, as explained by Luther and Clarke.10 Developmental dysplasia of the hip has been thoroughly investigated and documented, and it characteristically presents with hip instability affecting both acetabular and femoral development. It is detected in the neonatal period, and usually responds well to early conservative treatment. Neuromuscular dislocation results from an imbalance in muscular forces across the hip joint, which gradually affects the position of the femoral head and subsequently impairs acetabular development in the growth period. This type of dislocation generally presents later and requires primary surgical treatment. Although the two are separate entities, DDH may also occur in patients with underlying neurologic disease.
Of the ten patients studied in our series, seven had a pervasive developmental disorder. This type of disorder is not usually accompanied by significant abnormalities in muscle tone that would predispose the individual to late-onset neuromuscular dislocations, although it is frequently associated with mild degrees of hypotonia and abnormalities in motor coordination that are detected in early childhood.11–13 Of the three remaining patients, one received a diagnosis of Prader-Willi syndrome, which is characterised by obesity, hypogonadism, cognitive delay and hypotonia, and in which DDH occurs up to 10 times more than in the general population,14 a fact that may be related to the reduced muscle tone. No studies have been published on the specific subject of the treatment and outcomes of hip dysplasia in these patients. In our study, despite early diagnosis and treatment, the poor outcome of orthopaedic treatment led to the surgical correction by osteotomy of both hips. Another of our patients received a diagnosis of spastic diplegia after the neonatal diagnosis of DDH. This patient is scheduled to undergo bilateral periacetabular osteotomy because the AIs and femoral head coverage have improved very little since the beginning of treatment. The patient in our series that had hypoplasia of the corpus callosum, which was diagnosed late (at age 11 months),15 had mild axial hypotonia with normal muscle tone in the extremities. Despite treatment with a series of spica body casts, there has been little improvement and the patient is currently awaiting surgery for bilateral hip subluxation. The purpose in delaying surgical treatment in the last two patients is to allow them to develop a stable unassisted gait before the procedure.
The diagnosis of DDH was made in the neonatal period in six of the patients in our study. The delay in the diagnosis of the remaining patients (after age 6 months) could be associated with a poorer prognosis of orthopaedic treatment,3,6 but in our series we did not observe any differences between patients with a delayed diagnosis compared to those with an early diagnosis. Of the 16 hips in our series, 12 required invasive intervention for complete resolution. As for the degree of coverage of the femoral head, six of the hips continued to show some degree of migration, although the position of the femoral head improved in all.
Wilkinson and Sedgwick reviewed a series of 130 hips with DDH in which primary surgical treatment had failed, and found that 11% of these patients had occult spinal dysraphism or mild joint laxity. These authors suggested that weakness of the internal rotators of the hip might have been the cause of the observed residual subluxation that was refractory to treatment.16 It may be possible to extrapolate these findings to our case series, although we would need to obtain electromyographic data to confirm it.
The complications that developed during conservative treatment in our patients included avascular necrosis of the femoral head in three cases—a patchy necrosis in two cases that progressed to coxa magna in one, and total avascular necrosis in one case—with the incidence of this complication reaching 18%, substantially exceeding the rates reported in other published studies, which are of approximately 2.4%.2 Another patient had a femur fracture during treatment with the Pavlik harness, which caused a significant deformity that hindered the reduction of the dislocation and the subsequent outcome.
Patients with DDH that receive conservative treatment tend to have mild delays in achieving unassisted walking compared to the general population.14 However, our cases reached this milestone with a considerable delay, at a mean age of 2.4 years, although earlier than the mean age in patients with cerebral palsy, many of whom reach it past age 5 years.17
Psychomotor disorders were diagnosed after initiation of treatment for DDH in all patients in our series at a mean age of 2.5 years. The main challenge in this type of disorders is the difficulty in making an early diagnosis. With the exception of those affected by Prader-Willi syndrome, these patients do not have distinctive features to guide the diagnosis, and exhibit normal psychomotor development at early ages in most cases, with the disorder manifesting gradually as they grow.
In our series of 325 cases treated for DDH we only found 16 hips (5%) in 10 patients that had a psychomotor disorder. While it would not be counterproductive to keep in mind this possibility in the early weeks of life of a patient with DDH, we do not think that families should be informed of it, as the presence or absence of neurologic disease in these patients is not known at the outset and it would create unnecessary alarm in most of the families.
Conversely, being aware of it may be useful if conservative orthopaedic treatment is completed and the outcome is not satisfactory, with the patient requiring surgery. We believe that it is when failure of treatment for DDH is accompanied by a delay in achieving motor or cognitive milestones (speech, crawling, walking…) that the child should be referred for evaluation by a paediatric neurologist and the family informed of this possibility.
The limitations of our study are those inherent in its retrospective design, the small number of patients that met the inclusion criteria, having different periods of followup, and lack of a standard protocol for imaging tests. However, it seems evident that the outcomes of conservative treatment in these patients are poor, which opens up a new line of research on the impact of psychomotor disorders as risk factors for a poor prognosis in DDH that could be subject to further study.
Conflict of interestsThe authors have no conflict of interests to declare
Please cite this article as: Pipa-Muñiz I, Rodríguez-Rodríguez ML, Felgueroso-Juliana MB, Riera-Campillo M, González-Herranz P. Displasia del desarrollo de la cadera en niños con trastorno psicomotor. ¿Factor de riesgo para un mal resultado?. An Pediatr (Barc). 2016;85:142–148.