Graves disease (GD) is the leading cause of hyperthyroidism in the paediatric population. It is an autoimmune disease characterised by the production of antibodies against the thyroid stimulating hormone receptor (TSHR) and progressive infiltration of the thyroid by T and B lymphocytes.1
There are 3 types of antibodies that bind TSHR, or thyroid receptor antibodies (TRAb): thyroid-stimulating antibodies (TSAb); TSH-stimulation blocking antibodies (TBAb) and so-called “neutral” TRAb.1 These antibodies can be detected by immunoassays with a sensitivity of up to 98% in third-generation binding assays,1,2 or by means of cell-based bioassays, which measure functional activity and may even be more sensitive.1–3
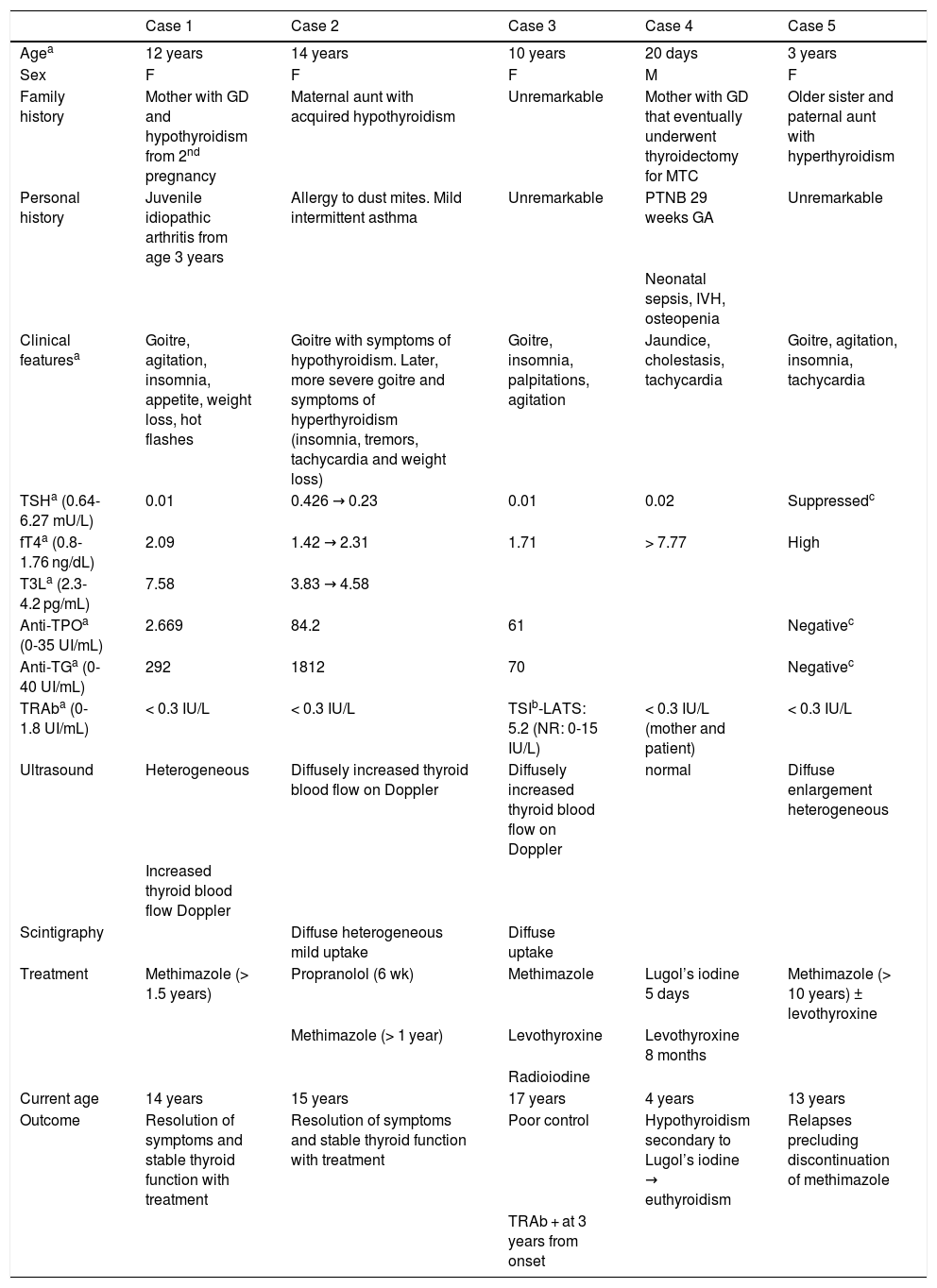
The diagnosis of GD is based on the detection of lower-than-normal levels of TSH and presence of TRAb.4 However, TRAb are not found in some patients that have clinical manifestations, a hormone profile and imaging features highly indicative of GD.3Table 1 summarises 5 paediatric cases of this clinical presentation that has yet to be thoroughly investigated and not well understood.
Summary of the clinical presentation, diagnostic test, treatment and outcomes of the cases.
| Case 1 | Case 2 | Case 3 | Case 4 | Case 5 | |
|---|---|---|---|---|---|
| Agea | 12 years | 14 years | 10 years | 20 days | 3 years |
| Sex | F | F | F | M | F |
| Family history | Mother with GD and hypothyroidism from 2nd pregnancy | Maternal aunt with acquired hypothyroidism | Unremarkable | Mother with GD that eventually underwent thyroidectomy for MTC | Older sister and paternal aunt with hyperthyroidism |
| Personal history | Juvenile idiopathic arthritis from age 3 years | Allergy to dust mites. Mild intermittent asthma | Unremarkable | PTNB 29 weeks GA | Unremarkable |
| Neonatal sepsis, IVH, osteopenia | |||||
| Clinical featuresa | Goitre, agitation, insomnia, appetite, weight loss, hot flashes | Goitre with symptoms of hypothyroidism. Later, more severe goitre and symptoms of hyperthyroidism (insomnia, tremors, tachycardia and weight loss) | Goitre, insomnia, palpitations, agitation | Jaundice, cholestasis, tachycardia | Goitre, agitation, insomnia, tachycardia |
| TSHa (0.64-6.27 mU/L) | 0.01 | 0.426 → 0.23 | 0.01 | 0.02 | Suppressedc |
| fT4a (0.8-1.76 ng/dL) | 2.09 | 1.42 → 2.31 | 1.71 | > 7.77 | High |
| T3La (2.3-4.2 pg/mL) | 7.58 | 3.83 → 4.58 | |||
| Anti-TPOa (0-35 UI/mL) | 2.669 | 84.2 | 61 | Negativec | |
| Anti-TGa (0-40 UI/mL) | 292 | 1812 | 70 | Negativec | |
| TRAba (0-1.8 UI/mL) | < 0.3 IU/L | < 0.3 IU/L | TSIb-LATS: 5.2 (NR: 0-15 IU/L) | < 0.3 IU/L (mother and patient) | < 0.3 IU/L |
| Ultrasound | Heterogeneous | Diffusely increased thyroid blood flow on Doppler | Diffusely increased thyroid blood flow on Doppler | normal | Diffuse enlargement heterogeneous |
| Increased thyroid blood flow Doppler | |||||
| Scintigraphy | Diffuse heterogeneous mild uptake | Diffuse uptake | |||
| Treatment | Methimazole (> 1.5 years) | Propranolol (6 wk) | Methimazole | Lugol’s iodine 5 days | Methimazole (> 10 years) ± levothyroxine |
| Methimazole (> 1 year) | Levothyroxine | Levothyroxine 8 months | |||
| Radioiodine | |||||
| Current age | 14 years | 15 years | 17 years | 4 years | 13 years |
| Outcome | Resolution of symptoms and stable thyroid function with treatment | Resolution of symptoms and stable thyroid function with treatment | Poor control | Hypothyroidism secondary to Lugol’s iodine → euthyroidism | Relapses precluding discontinuation of methimazole |
| TRAb + at 3 years from onset |
The normal range applied in our laboratory is presented in parenthesis along with the corresponding units of measure.
fT4, free thyroxine; GA, gestational age; GD, gestational diabetes; IVH, intraventricular haemorrhage; MTC, medullary thyroid cancer; NR, normal range; PTNB, preterm newborn; LATS, long-acting thyroid stimulator; TG, thyroglobulin; TPO, thyroid peroxidase; TRAb, TSH Receptor Antibody; TSH, thyroid-stimulating hormone; TSI, thyroid-stimulating immunoglobulin.
Case 1: pubertal patient with a personal and family history of autoimmune disease presenting with clinical hyperthyroidism with low levels of TSH and levels of free thyroxine (T4) in the upper limit of normal in successive laboratory tests in the 2 months that followed. The levels of anti-thyroid peroxidase (TPO) antibodies and anti-thyroglobulin (TG) antibodies were high, and the findings of the ultrasound examination were compatible with thyroiditis. The disease is currently controlled with antithyroid drugs.
Case 2: adolescent aged 14 years presenting with manifestations characteristic of hypothyroidism at onset: asthenia, malaise, somnolence, abdominal pain, constipation and decreased appetite. The relevant findings of blood tests were a low level of TSH with an initially normal level of free T4, with progression within a month to a presentation more characteristic of hyperthyroidism: palpitations, agitation, insomnia, palpebral retraction, goitre and elevation of free T4.
Case 3: girl aged 10 years with clinical and biochemical features compatible with hyperthyroidism. During the follow-up, the patient exhibited hypothyroidism at low doses of methimazole, leading to discontinuation of treatment after 1.5 years, upon which the patient relapsed and was finally treated with radioiodine. The TRAb detection tests were mildly positive using first-generation assays at 3 years from onset, and later became clearly positive with second-generation binding assays.
Case 4: newborn infant that developed transient neonatal hyperthyroidism with a family history of GD in the mother, who had undergone thyroidectomy for treatment of papillary thyroid cancer. The results of second-generation binding assays for detection of TRAb were negative in both mother and child.
Case 5: patient presenting with early-onset persistent hyperthyroidism with a family history of hyperthyroidism and negative TRAb results. The results of gene testing for TSHR-activating mutations were negative. The patient is scheduled to receive radioiodine for curative treatment.
Although there are few studies in the paediatric population, it appears that patients with hyperthyroidism compatible with GD and undetectable levels of TRAb exhibit thyrotoxicosis with milder clinical manifestations and biochemical abnormalities.3 In this regard, our findings were consistent with the existing literature: none of the 5 patients had thyroid eye disease or pretibial myxoedema, and the levels of free T4 at diagnosis were not very high.
In cases 2 and 3, with a mostly silent course, we could hypothesise the coexistence of TSAb and TBAb in the disease process. Recent studies have found evidence of coexistence and changes in the relative proportions of TSAb and TBAb in a single patient, mainly during pregnancy and in up to 10% of patients with GD treated with antithyroid drugs.4 For this reason, in addition to their higher sensitivity, some authors recommend using bioassays in the diagnosis of patients expected to have low antibody levels, pregnant women and cases of neonatal hyperthyroidism.2
If a patient presents with hyperthyroidism and tests negative for TRAb, the first step would be to make a differential diagnosis with the thyrotoxic phase of Hashimoto thyroiditis (ultrasound findings and compatible antibodies with a reduction in free T4 levels in a few weeks). Although they are infrequent (4.5% of patients with hyperthyroidism, diffuse goitre and negative TRAb5), in cases with early onset, a relevant family history and a poor response to antithyroid drugs (case 5), the possibility of TSHR-activating mutations should be contemplated. Other causes of thyrotoxicosis can be ruled out through the history-taking, physical examination and sonography.
Once the alternative diagnoses have been ruled out, one possible explanation to negative results of tests for detection of TRAb is that they may not be sensitive enough to detect low antibody concentrations. Another possible explanation is that the production of TRAb is restricted to the thyroid and the antibodies never enter the systemic circulation. This hypothesis is based on evidence that lymphocytes isolated from the thyroid of a patient with autoimmune thyroiditis in whom TRAb were not detected in blood could produce antithyroid autoantibodies.3,6
In conclusion, GD cannot be ruled out in patients with a clinical presentation compatible with hyperthyroidism and negative TRAb. It is important to be aware of this potential presentation in order to initiate treatment with antithyroid agents as soon as possible.
Please cite this article as: Scatti Regàs A, Pujol Borrell R, Ferrer Costa R, Puerto Carranza E, Clemente León M. Enfermedad de Graves con autoanticuerpos contra el receptor de la TSH negativos: a propósito de 5 casos. An Pediatr (Barc). 2020;93:417–419.