Haemophagocytic syndrome is characterised by an excessive systemic inflammatory response. This syndrome is classified into different subgroups based on its aetiology. Infections may trigger the inflammatory cascade, and viral infections in general, and infection by Epstein-Barr virus in particular, are the most frequent infectious triggers. However, other pathogens, including bacteria, fungi and parasites, can also trigger it. There are no published cases in the literature of haemophagocytic syndrome secondary to infection by Streptococcus pyogenes, or group A streptococcus (GAS), although cases associated with other streptococci have been described.1–3 In recent decades, there has been an increase in the incidence of streptococcal infections and, therefore, also of severe disease cause by these bacteria.4 There is a growing interest in understanding the virulence factors in GAS that lead to inflammation, including its ability to secrete superantigens5,6 that can trigger an excessive cell-mediated immune response. Here, we present a case of haemophagocytic-like syndrome disease secondary to infection by GAS.
The patient was a previously healthy girl aged 6 years admitted for evaluation of prolonged fever. She had fever with temperatures of up to 41 °C with frequent spikes with onset 7 days prior, had been assessed for this reason several times in the emergency department of the hospital and for the past 4 days had been receiving oral phenoxymethylpenicillin for treatment of streptococcal pharyngitis (following a positive result in the rapid strep test) without improvement. In the examination, the vital signs were in the normal range save for a temperature of 38.2 °C, and the patient presented with generalised pruritic erythematous exanthema with palmoplantar involvement, petechial enanthema in the pharynx and reactive cervical lymphadenopathy, with no evidence of organ enlargement on abdominal palpation.
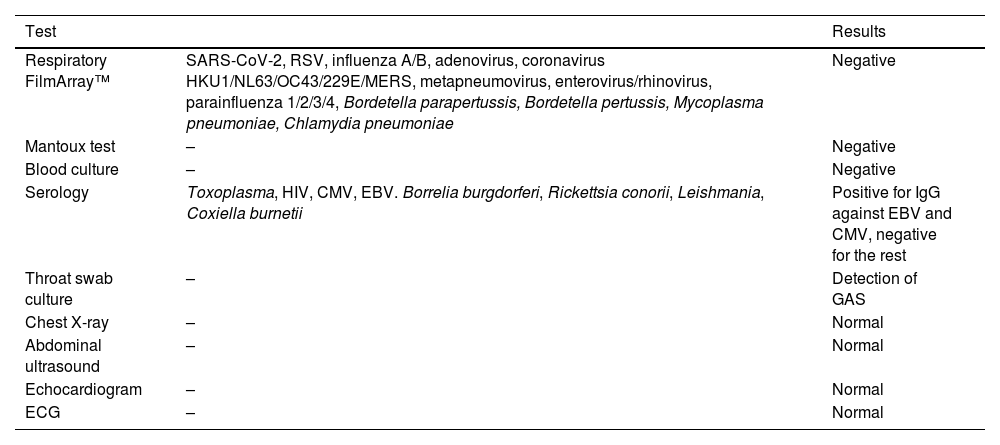
The salient findings of the blood panel were elevation of acute phase reactants (C-reactive protein [CRP], 37.32 mg/L; procalcitonin [PCT], 0.9 ng/mL; ferritin, 1469 ng/mL), liver enzymes (aspartate aminotransferase [AST], 103 U/L; alanine aminotransferase [ALT], 135 U/L; gamma-glutamyl transferase [GGT], 119 U/L) and lactate dehydrogenase (LDH, 555 U/L) and hypertriglyceridaemia (blood triglycerides, 242 mg/dL). The complete blood count evinced bicytopenia with decreased neutrophil (0.8 × 109 cells/L) and platelet (91 × 109/L) counts. In the coagulation tests, the level of D dimer was 6063 ng/mL. Different tests were performed for aetiological diagnosis (Table 1). To rule out incomplete Kawasaki disease, the evaluation was completed with an electrocardiogram and echocardiogram, the findings of which were normal. The levels of troponin T and N-terminal pro b-type natriuretic peptide (NT-proBNP) were also measured and found to be normal. There was no evidence suggestive of recent infection by SARS-CoV-2, so we did not suspect multisystemic inflammatory syndrome secondary to this infection.
Performed diagnostic tests and their results.
| Test | Results | |
|---|---|---|
| Respiratory FilmArray™ | SARS-CoV-2, RSV, influenza A/B, adenovirus, coronavirus HKU1/NL63/OC43/229E/MERS, metapneumovirus, enterovirus/rhinovirus, parainfluenza 1/2/3/4, Bordetella parapertussis, Bordetella pertussis, Mycoplasma pneumoniae, Chlamydia pneumoniae | Negative |
| Mantoux test | – | Negative |
| Blood culture | – | Negative |
| Serology | Toxoplasma, HIV, CMV, EBV. Borrelia burgdorferi, Rickettsia conorii, Leishmania, Coxiella burnetii | Positive for IgG against EBV and CMV, negative for the rest |
| Throat swab culture | – | Detection of GAS |
| Chest X-ray | – | Normal |
| Abdominal ultrasound | – | Normal |
| Echocardiogram | – | Normal |
| ECG | – | Normal |
CMV, cytomegalovirus; EBV, Epstein-Barr virus; ECG, electrocardiogram; GAS, group A Streptococcus pyogenes; HIV, human immunodeficiency virus; IgG, immunoglobulin type G; RSV, respiratory syncytial virus.
The chief suspected diagnosis, given the prolonged fever and the laboratory abnormalities with low counts in 2 out of the 3 blood cell lineages, hypertriglyceridaemia and increased ferritin levels, was secondary haemophagocytic syndrome. This led to measurement of the soluble interleukin 2 receptor (sCD25) level, which turned out to be elevated: 2904 U/mL (normal range < 623). To be accurate, the patient met 4 of the 5 clinical and laboratory criteria (HLH-2004 protocol) required for diagnosis. The fifth criteria is the level of triglycerides, and, while the patient did not have a level greater than 265 mg/dL, as specified in these criteria, she did have hypertriglyceridaemia (242 mg/dL). Therefore, we concluded that she had a haemophagocytic-like syndrome secondary to infection by GAS.
The patient received intravenous antibiotherapy with ampicillin through the hospital stay. Contrary to haemophagocytic syndromes of a viral aetiology, she exhibited progressive improvement without targeted therapy and became afebrile within 24 h of admission. The follow-up laboratory tests performed before discharge showed improvement of inflammatory markers, a decrease in ferritin levels to 923 ng/mL, less severe elevation of liver enzymes and normal blood counts. The patient was discharged 48 h after admission with scheduled follow-up at the outpatient clinics and with a prescription of oral amoxicillin for completion of a 10-days course. In the outpatient follow-up visit, all clinical and laboratory findings were normal.
It is known that GAS can secrete superantigens5,6 that stimulate cell-mediated immunity. In addition, activated T cells express the sCD25 antigens that act as mediators of the macrophage activation present in haemophagocytic syndrome. Therefore, we hypothesise that in our patient, the immune dysregulation caused by the systemic hyperinflammatory state was triggered by superantigens secreted by GAS, which can occur in association with other streptococcal species but had yet to be described in association with GAS, which is why we considered publishing this case relevant, given the evidence of the increased incidence of infection by GAS and the ongoing discussion about changes in GAS virulence.