The development of paediatrics as a medical speciality has achieved an increase in the survival of patients with complex chronic conditions (CCCs).1 Within this group is the subset that we refer to as complex chronic paediatric patients (CCPPs), for which there is no consensus-based definition, characterised by a greater vulnerability and dependence. However, delivering adequate care to these patients requires that they be correctly identified.2,3
In 2022, our research group published a study presenting the first version of a scale (PedCom) developed to identify CCPPs.2 After its publication, comprehension problems emerged for several items and the need to include new devices arose, so we decided to revise the scale to update and validate it. We also proposed translating it to English to facilitate its international diffusion.
The study was conducted in a tertiary care children’s hospital that has a paediatric palliative care and complex chronic disease unit after obtaining approval from the provincial research ethics committee. We applied the inclusion and exclusion criteria used in the pilot study.2 The scale was revised applying the guidelines for scale development proposed by Clark et al.4
To validate the resulting scale, we followed the same steps applied in the pilot study.2 For the sample size, we estimated we needed a minimum of 5 patients per item included in the analysis. We calculated the content validity ratio (CVR > 0.58), the overall content validity index (CVI > 0.58), the internal consistency coefficient (Cronbach α, 0.7−0.9) and intrarater and inter-rater agreement coefficients, and established the cut-off point by means of the receiver operating characteristic (ROC) curve. We also compared the patients classified as having complex chronic disease by the scale with the diagnoses contemplated in the Pediatric Complex Condition Classification System version 2.5
Two accredited translators translated the scale independently and then produced a single version by consensus. This was followed by reverse translation.
After the first revision, we obtained a version with 11 sections and 47 items; this resulted in a loss of internal consistency, so certain items were rewritten and grouped, for instance, the items pertaining to ventilatory support devices, vesicostomy, ureterostomy and bladder catheterization, to peritoneal dialysis and haemodialysis or the type of school. Changes were made to the scoring of items such as “hospital only” and home medication, pacemaker, ileostomy/colostomy, dialysis or haemodialysis and life expectancy. The section concerning hospitalizations was also removed.
These modifications yielded a final version with 10 sections and 42 items with an overall CVI of 0.92. Table 1 presents the final validated scale. We calculated a minimum sample size of 210 patients, and the final sample included 350 participants.
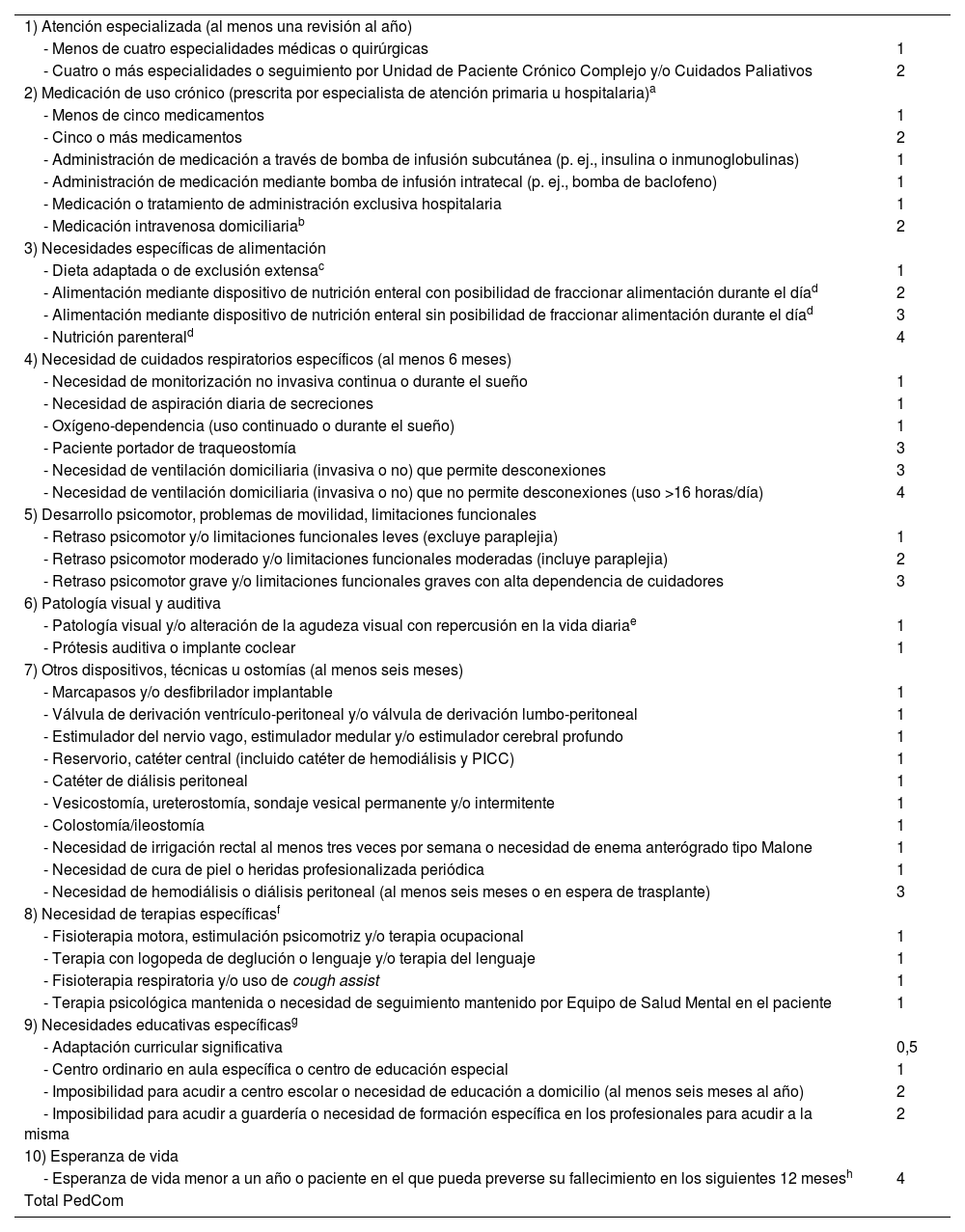
Escala para la identificación del paciente pediátrico crónico complejo (PedCom®). El ítem a evaluar debe haber durado o preverse que dure al menos 12 meses salvo otra especificación.
| 1) Atención especializada (al menos una revisión al año) | |
| - Menos de cuatro especialidades médicas o quirúrgicas | 1 |
| - Cuatro o más especialidades o seguimiento por Unidad de Paciente Crónico Complejo y/o Cuidados Paliativos | 2 |
| 2) Medicación de uso crónico (prescrita por especialista de atención primaria u hospitalaria)a | |
| - Menos de cinco medicamentos | 1 |
| - Cinco o más medicamentos | 2 |
| - Administración de medicación a través de bomba de infusión subcutánea (p. ej., insulina o inmunoglobulinas) | 1 |
| - Administración de medicación mediante bomba de infusión intratecal (p. ej., bomba de baclofeno) | 1 |
| - Medicación o tratamiento de administración exclusiva hospitalaria | 1 |
| - Medicación intravenosa domiciliariab | 2 |
| 3) Necesidades específicas de alimentación | |
| - Dieta adaptada o de exclusión extensac | 1 |
| - Alimentación mediante dispositivo de nutrición enteral con posibilidad de fraccionar alimentación durante el díad | 2 |
| - Alimentación mediante dispositivo de nutrición enteral sin posibilidad de fraccionar alimentación durante el díad | 3 |
| - Nutrición parenterald | 4 |
| 4) Necesidad de cuidados respiratorios específicos (al menos 6 meses) | |
| - Necesidad de monitorización no invasiva continua o durante el sueño | 1 |
| - Necesidad de aspiración diaria de secreciones | 1 |
| - Oxígeno-dependencia (uso continuado o durante el sueño) | 1 |
| - Paciente portador de traqueostomía | 3 |
| - Necesidad de ventilación domiciliaria (invasiva o no) que permite desconexiones | 3 |
| - Necesidad de ventilación domiciliaria (invasiva o no) que no permite desconexiones (uso >16 horas/día) | 4 |
| 5) Desarrollo psicomotor, problemas de movilidad, limitaciones funcionales | |
| - Retraso psicomotor y/o limitaciones funcionales leves (excluye paraplejia) | 1 |
| - Retraso psicomotor moderado y/o limitaciones funcionales moderadas (incluye paraplejia) | 2 |
| - Retraso psicomotor grave y/o limitaciones funcionales graves con alta dependencia de cuidadores | 3 |
| 6) Patología visual y auditiva | |
| - Patología visual y/o alteración de la agudeza visual con repercusión en la vida diariae | 1 |
| - Prótesis auditiva o implante coclear | 1 |
| 7) Otros dispositivos, técnicas u ostomías (al menos seis meses) | |
| - Marcapasos y/o desfibrilador implantable | 1 |
| - Válvula de derivación ventrículo-peritoneal y/o válvula de derivación lumbo-peritoneal | 1 |
| - Estimulador del nervio vago, estimulador medular y/o estimulador cerebral profundo | 1 |
| - Reservorio, catéter central (incluido catéter de hemodiálisis y PICC) | 1 |
| - Catéter de diálisis peritoneal | 1 |
| - Vesicostomía, ureterostomía, sondaje vesical permanente y/o intermitente | 1 |
| - Colostomía/ileostomía | 1 |
| - Necesidad de irrigación rectal al menos tres veces por semana o necesidad de enema anterógrado tipo Malone | 1 |
| - Necesidad de cura de piel o heridas profesionalizada periódica | 1 |
| - Necesidad de hemodiálisis o diálisis peritoneal (al menos seis meses o en espera de trasplante) | 3 |
| 8) Necesidad de terapias específicasf | |
| - Fisioterapia motora, estimulación psicomotriz y/o terapia ocupacional | 1 |
| - Terapia con logopeda de deglución o lenguaje y/o terapia del lenguaje | 1 |
| - Fisioterapia respiratoria y/o uso de cough assist | 1 |
| - Terapia psicológica mantenida o necesidad de seguimiento mantenido por Equipo de Salud Mental en el paciente | 1 |
| 9) Necesidades educativas específicasg | |
| - Adaptación curricular significativa | 0,5 |
| - Centro ordinario en aula específica o centro de educación especial | 1 |
| - Imposibilidad para acudir a centro escolar o necesidad de educación a domicilio (al menos seis meses al año) | 2 |
| - Imposibilidad para acudir a guardería o necesidad de formación específica en los profesionales para acudir a la misma | 2 |
| 10) Esperanza de vida | |
| - Esperanza de vida menor a un año o paciente en el que pueda preverse su fallecimiento en los siguientes 12 mesesh | 4 |
| Total PedCom |
PICC: catéter central de inserción periférica.
Si puntuación mayor o igual a 6,5 puntos el paciente es clasificado como Paciente Crónico Complejo.
Recordar siempre el criterio temporal a la hora de analizar cada ítem.
En pacientes con esperanza de vida menor a un año no se exige el tiempo mínimo para cada ítem. Debe evitarse aplicar la escala en situaciones de descompensación aguda o reagudización de la enfermedad de base salvo en casos en los que no se espere una recuperación a situación basal.
Observaciones.
Los únicos apartados excluyentes entre sí son el ítem uno y dos. Los pacientes que reciben hemodiálisis deben puntuar también en el apartado de medicación/tratamiento hospitalario.
Por ejemplo, transfusiones periódicas, antibioterapia intravenosa (mínimo dos ciclos en los últimos 12 meses).
Recordar el criterio temporal. Incluye: diabetes, enfermedad renal crónica y errores innatos del metabolismo que requieran de dieta específica, alergia alimentaria múltiple (tres o más grupos alimentarios), dieta cetogénica y trastornos de deglución o disfagia que requieran adaptación de dieta. Los casos no incluidos deben valorarse de forma individualizada.
Que haya durado o se prevea que dure al menos seis meses. Incluye todos los dispositivos de nutrición enteral. No debe sumarse el punto de alimentación especial. Un paciente con nutrición parenteral puede sumar por la nutrición enteral si realiza nutrición mixta.
No sumar en pacientes con patología neurológica moderada/grave en los que la alteración de la visión no genera repercusión sobre su actividad diaria o si las lentes correctoras permiten corregir/compensar el déficit.
Incluye fisioterapia profesionalizada o no profesionalizada (p.ej., realizada por familiar formado). Solo recoger terapias que estén indicadas debido a la patología del paciente.
Escoger solo un ítem. No deben puntuarse aquellos pacientes que no acuden a guardería o centro educativo por decisión de la familia sin que exista un criterio médico que lo justifique; en ese caso, elegir la opción que más se ajuste a la situación clínica del paciente.
Incluir pacientes en los que, dado su diagnóstico, evolución de su enfermedad, fragilidad o situación de inestabilidad; pueda ser previsible su fallecimiento en los siguientes 12 meses. Por ejemplo, paciente con parálisis cerebral grave, deterioro clínico en los últimos meses y reagudizaciones respiratorias frecuentes.
We obtained a Cronbach α of 0.73. The intraclass correlation coefficient in the test-retest analysis by means of 2-way mixed-effect ANOVA was 0.997 (95% confidence interval [CI], 0.996−0.997). In the analysis of interrater agreement, we obtained an intraclass correlation coefficient of 0.995 (95% CI, 0.994−0.996) in the 2-way random effects model.
The threshold to consider a patient as a CCPP was established at 6.5 points. This threshold had a sensitivity of 96% and a specificity of 97% with a positive predictive value of 97% and a negative predictive value of 96%. The Cohen kappa coefficient was 0.966 (P < 0.01) in the analysis of test-retest reliability and 0.954 (P < 0.01) in the analysis of interrater agreement.
When we compared the patients identified as CCPPs by the scale to the diagnostic codes contemplated in the CCC classification system published by Feudtner et al.5 we found that 247 of the 350 participants had at least one CCC (70.6%); of this total, only 171 (69.2%) met the criteria for classification as a CCPP.
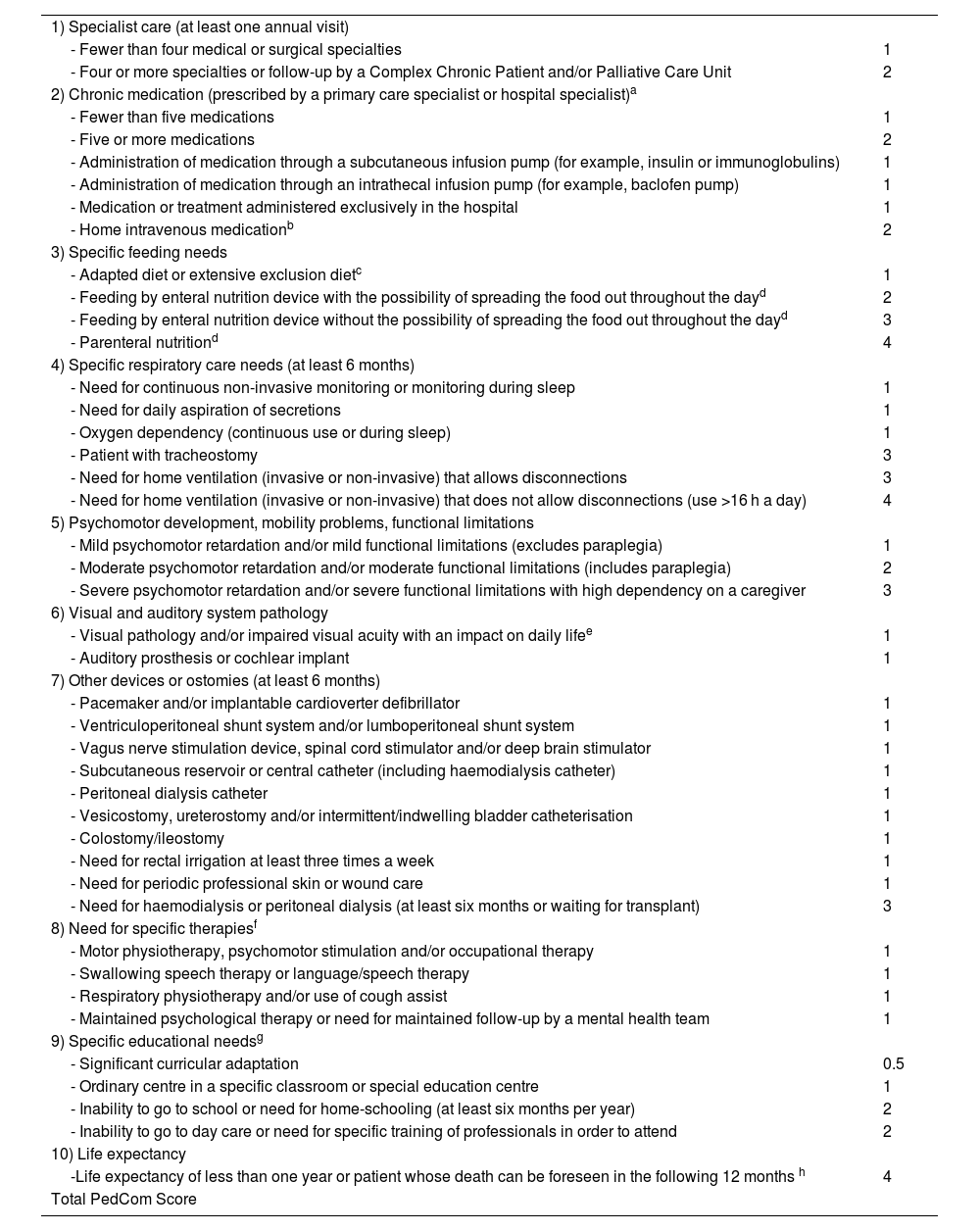
The translation of the scale to English can be found in Table 2.
Scale for the identification of the complex chronic paediatric patient (PedCom Scale®) The item to be evaluated must have lasted or be expected to last at least 12 months, unless specified otherwise.
| 1) Specialist care (at least one annual visit) | |
| - Fewer than four medical or surgical specialties | 1 |
| - Four or more specialties or follow-up by a Complex Chronic Patient and/or Palliative Care Unit | 2 |
| 2) Chronic medication (prescribed by a primary care specialist or hospital specialist)a | |
| - Fewer than five medications | 1 |
| - Five or more medications | 2 |
| - Administration of medication through a subcutaneous infusion pump (for example, insulin or immunoglobulins) | 1 |
| - Administration of medication through an intrathecal infusion pump (for example, baclofen pump) | 1 |
| - Medication or treatment administered exclusively in the hospital | 1 |
| - Home intravenous medicationb | 2 |
| 3) Specific feeding needs | |
| - Adapted diet or extensive exclusion dietc | 1 |
| - Feeding by enteral nutrition device with the possibility of spreading the food out throughout the dayd | 2 |
| - Feeding by enteral nutrition device without the possibility of spreading the food out throughout the dayd | 3 |
| - Parenteral nutritiond | 4 |
| 4) Specific respiratory care needs (at least 6 months) | |
| - Need for continuous non-invasive monitoring or monitoring during sleep | 1 |
| - Need for daily aspiration of secretions | 1 |
| - Oxygen dependency (continuous use or during sleep) | 1 |
| - Patient with tracheostomy | 3 |
| - Need for home ventilation (invasive or non-invasive) that allows disconnections | 3 |
| - Need for home ventilation (invasive or non-invasive) that does not allow disconnections (use >16 h a day) | 4 |
| 5) Psychomotor development, mobility problems, functional limitations | |
| - Mild psychomotor retardation and/or mild functional limitations (excludes paraplegia) | 1 |
| - Moderate psychomotor retardation and/or moderate functional limitations (includes paraplegia) | 2 |
| - Severe psychomotor retardation and/or severe functional limitations with high dependency on a caregiver | 3 |
| 6) Visual and auditory system pathology | |
| - Visual pathology and/or impaired visual acuity with an impact on daily lifee | 1 |
| - Auditory prosthesis or cochlear implant | 1 |
| 7) Other devices or ostomies (at least 6 months) | |
| - Pacemaker and/or implantable cardioverter defibrillator | 1 |
| - Ventriculoperitoneal shunt system and/or lumboperitoneal shunt system | 1 |
| - Vagus nerve stimulation device, spinal cord stimulator and/or deep brain stimulator | 1 |
| - Subcutaneous reservoir or central catheter (including haemodialysis catheter) | 1 |
| - Peritoneal dialysis catheter | 1 |
| - Vesicostomy, ureterostomy and/or intermittent/indwelling bladder catheterisation | 1 |
| - Colostomy/ileostomy | 1 |
| - Need for rectal irrigation at least three times a week | 1 |
| - Need for periodic professional skin or wound care | 1 |
| - Need for haemodialysis or peritoneal dialysis (at least six months or waiting for transplant) | 3 |
| 8) Need for specific therapiesf | |
| - Motor physiotherapy, psychomotor stimulation and/or occupational therapy | 1 |
| - Swallowing speech therapy or language/speech therapy | 1 |
| - Respiratory physiotherapy and/or use of cough assist | 1 |
| - Maintained psychological therapy or need for maintained follow-up by a mental health team | 1 |
| 9) Specific educational needsg | |
| - Significant curricular adaptation | 0.5 |
| - Ordinary centre in a specific classroom or special education centre | 1 |
| - Inability to go to school or need for home-schooling (at least six months per year) | 2 |
| - Inability to go to day care or need for specific training of professionals in order to attend | 2 |
| 10) Life expectancy | |
| -Life expectancy of less than one year or patient whose death can be foreseen in the following 12 months h | 4 |
| Total PedCom Score |
If the score is greater than or equal to 6.5 points, the patient can be classified as a Complex Chronic Patient.
Always remember the time criteria when analysing each item.
In patients with a life expectancy of less than one year, the minimum time for each item is not required. However, the scale should not be applied in case of acute decompensation or exacerbation of the underlying disease unless recovery to baseline is not expected.
Observations.
The only mutually exclusive sections are items one and two. Patients receiving haemodialysis should also score in the section of hospital medication/treatment.
For example: periodic transfusions, intravenous antibiotic therapy (minimum two cycles in the last twelve months).
Remember the time criteria. This includes diabetes, chronic kidney disease, inborn errors of metabolism that require a specific diet, multiple food allergies (three or more food groups), ketogenic diet and swallowing disorders or dysphagia that require diet adaptation. Those cases not included should be assessed on an individual basis.
That has lasted or is expected to last at least six months. Includes all enteral nutrition devices. The special diet point should not be added. A patient receiving parenteral nutrition can score for enteral nutrition if mixed nutrition is performed.
Do not add in patients with moderate/severe neurological disability in which the change in vision does not have an impact on their daily activity or if the corrective lenses correct/compensate for the deficit.
Includes professional or non-professional rehabilitation (for example, rehabilitation carried out by a trained family member). Only collect therapies indicated due to the patient’s pathology.
Only choose one item. Those patients who do not attend day care or an educational centre by decision of the family, without medical criteria justifying this, should not be scored; in this case, choose the option that best suits the patient’s clinical situation.
This includes patients in whom, given their diagnosis, the evolution of disease, extreme frailty or unstable situation, death may be foreseeable in the following 12 months. For example: patient with severe cerebral palsy, clinical deterioration in recent months and frequent respiratory exacerbations.
The PedCom scale is the first instrument designed and validated to identify CCPPs, and it has exhibited an adequate internal consistency, a good intrarater and inter-rater agreement and a good sensitivity and specificity. It contributes a new approach that is based on the limitations and needs of the patients, the sum of which determines the classification of the child as a complex, chronically ill patient, with no single diagnosis or characteristic allowing this classification.
This instrument fulfils a need in paediatric clinical practice, as it is simple to use and can be applied both in primary care and hospital settings, and its use will improve the care of these children and their families, the efficiency of care delivery and the allocation of available resources.
FundingThis project was funded through a grant from the Sociedad Pediátrica de Andalucía Oriental (SPAO 2020) for a total of Є5000.