The increase in recreational scuba diving in recent years, including children, involves risks and the possibility of accidents. While legislation, conditions and risks of scuba diving are well documented in adults, scientific evidence in scuba diving by children and adolescents is sparse and isolated. Furthermore, existing guidelines and recommendations for adults cannot be transferred directly to children.
MethodsThese circumstances have led to the Group on Techniques of the Spanish Society of Paediatric Pulmonology (SENP) to perform a literature search to review and update the knowledge about scuba diving in children.
ResultsPhysiological adaptations of the body are examined during the dive, as well as the anatomical and physiological characteristics of children that should be taken into account in scuba diving. The most common types of accidents and its causes, as well as the risks of scuba diving practice in children with previous diseases are discussed, along with details of the medical and psychological requirements for scuba diving to be considered in the assessment of child and adolescent.
ConclusionsA list of recommendations for scuba diving with compressed air in children is presented by a group of experts.
El gran auge de la práctica recreativa del buceo en los últimos años, incluyendo a los niños, comporta riesgos y la posibilidad de accidentes. Mientras que las normativas, los requisitos y los riesgos del buceo en adultos están bien fundamentados, la evidencia científica en niños y adolescentes es escasa. Asimismo, las guías y recomendaciones existentes dirigidas a los adultos no pueden ser aplicadas directamente a los niños.
MétodosEstas circunstancias han motivado al Grupo de Técnicas de la Sociedad española de Neumología Pediátrica (SENP) a realizar una búsqueda bibliográfica para revisar y actualizar los conocimientos sobre el buceo en la edad pediátrica.
ResultadosSe examinan las adaptaciones fisiológicas del organismo durante la inmersión, así como las características anatómicas y fisiológicas propias de los niños que deben considerarse con relación al submarinismo; se exponen las causas y tipos más frecuentes de accidentes, así como los riesgos de su práctica en niños con distintas patologías; y se detallan los requisitos médicos y psicológicos para el buceo que deben respetarse en la evaluación de niño y adolescentes.
ConclusionesFinalmente, se formulan unas recomendaciones de expertos para la práctica del buceo con aire comprimido en la edad pediátrica.
The number of children engaging in scuba diving has steadily increased in recent years, and now represents between 5 and 10%1,2 of recreational divers. The majority are between the ages of 12 and 17 years, but 1.5% of active divers are children under the age of 12 years.3,4 Despite this, Spanish regulations on children's diving are difficult to interpret and vary substantially between local jurisdictions.5 Likewise, although the medical risks of diving in adults are well-founded, scientific evidence available regarding children is scarce6,7 and recommendations are aimed at adults; there are none for the paediatric population.8,9
Considering this, the Group on Techniques of the Spanish Society of Paediatric Pulmonology decided to review the literature with the aim of establishing recommendations for scuba diving in children. In this article, we tackle the inherent issues regarding the practice of underwater activities for children, placing an emphasis on diving with compressed-air tanks. Taking into consideration anatomo-physiological, psychological and ergonomic aspects, data on children's diving is reviewed and updated, the most common types of accidents are presented, and the medical and psychological aspects to be considered when evaluating a child/adolescent who wishes to dive are discussed. Lastly, a few experts’ recommendations on scuba diving for children are summarised, in the absence of established facts on the subject.
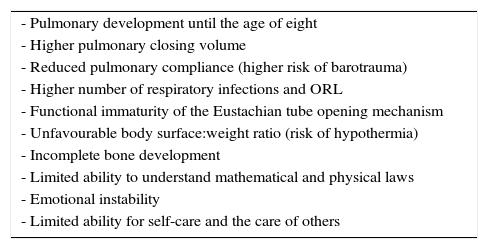
Physiological changes associated with divingWhen diving, the body must adapt to an environment with more pressure during immersion (compression) and then restabilise during ascent (decompression) and reach surface pressure conditions.10 An adequate knowledge of these adaptations and of the anatomophysiological characteristics of children (Table 1) will minimise the risks of diving.
Physiological and anatomical factors to be considered in children engaging in underwater activities.
| - Pulmonary development until the age of eight |
| - Higher pulmonary closing volume |
| - Reduced pulmonary compliance (higher risk of barotrauma) |
| - Higher number of respiratory infections and ORL |
| - Functional immaturity of the Eustachian tube opening mechanism |
| - Unfavourable body surface:weight ratio (risk of hypothermia) |
| - Incomplete bone development |
| - Limited ability to understand mathematical and physical laws |
| - Emotional instability |
| - Limited ability for self-care and the care of others |
When diving, pressure increases by 1 atmosphere for each 10m of descent.11 High pressure levels are relatively harmless and well tolerated by the body as long as they can be balanced or compensated. The increase in pressure during descent will compress the gas in the body's air cavities (lungs, middle ear, nasal sinus) and this gas will re-expand during ascent. In compressed-air diving, the main strategy used to avoid accidents is to maintain exhalation during ascent, avoiding pulmonary hyperinflation and the risk of pneumothorax.11
When diving with compressed-air tanks, breathing effort will increase due to both the need to transport larger quantities of air and to the increase in air density associated with depth. In addition, both inhalation and exhalation become active.10 Diving with intense effort can cause fatigue and risk of hypercapnia.11
As for respiratory gases, the increase in pressure due to depth disproportionately affects tissue diffusion rates, which are higher for O2 and CO2, and lower for N2.10 During immersion, tissue N2 uptake will take a long time to adjust to the depth. During ascent, N2 will be slowly released from the tissues.11 If ascent is performed too quickly, the rapid drop in pressure (decompression) will release N2 in the form of bubbles. Although most of the N2 bubbles are small and harmless, some can cause joint pain or, more severely, deafness, visual alterations or paresis/paralysis due to gas embolism.11 In addition, at depth both N2 and O2 can have toxic effects on the central nervous system. Under high levels of pressure (5atm–50m), N2 can cause euphoria, lack of co-ordination or even a coma; these effects are associated with its high solubility in fat. O2 can affect the central nervous system causing nausea, tinnitus, muscle spasms or seizures; these effects are associated with the release of inflammatory mediators.11 In recreational diving, the tanks used to breathe only have compressed ambient air.
In children, the effort of breathing during diving is even greater due to the smaller relative diameter of their airways and greater compliance, which predisposes their small airways to collapse and to the deterioration of gas exchange. In addition, respiratory infections in children are frequent, which increases the risk of airway obstruction. These elements, together with a higher closing volume in these ages, can contribute to a ventilation/perfusion mismatch and, during ascent, to an increase in trapped air and a risk of pulmonary barotrauma due to intrathoracic hypertension.12 Bronchial hyper-responsiveness can also be a risk due to elements usually present during immersion: exercise, breathing of dry, cold air, hyperventilation, a certain amount of anxiety, aspiration of small amounts of salt water. After immersion, even at swimming pool depth, FEV1, FEV1/FVC, MEF25 and MEF50 volumes decrease, although they are only significant (FEV1 reduction>10%) in 12–18% of children.13,14
Cardiovascular systemWhen diving, venous return increases due to atmospheric pressure and the vasoconstriction typical of cold environments, which increases cardiac output, systolic pressure volume and consequently, blood pressure.10 The increase in blood pressure heart rate and muscle activity, and the reduction in the secretion of ADH, triple urine production when diving.10
Patent foramen ovale (PFO) is more common in children and can be found in up to 40% of individuals. In PFO, right-to-left shunting can occur, and nitrogen bubbles can be ejected into the arterial circulation. Although accidents due to decompression are infrequent, their incidence and that of cerebral ischaemia disorders is higher (1/2000) in adult divers with PFO.15 In children, since there are no studies and PFO is more prevalent, a maximum depth limit for diving in which usually no micro-bubbles are generated (<10m)16 is recommended.
Inner ear and sinus problemsDuring descent, the diver will feel pain in the inner ears as pressure on the tympanic membrane increases. To balance this difference in pressure, the diver must be able to “compensate” by forcing air into the inner ear through the nasopharynx. The most common technique to balance pressure in the inner ears is the Valsalva manoeuvre,10 which is performed by attempting to exhale while closing the mouth and nostrils to increase and balance the pressure within the upper airways, Eustachian tubes and middle ear.
In children, the most common diving accidents involve otic lesions.17 The risk of suffering from otic barotrauma is higher in children18 since there are factors that hinder middle ear ventilation and pressure balance; an increase in inner ear infections, adenoid hypertrophy and a narrower, shorter and more horizontal Eustachian tube.
Locomotor systemThe articular cartilage in children and adolescents has been proposed as a vulnerable spot for gas micro-embolism due to its rich vascularisation and high metabolism.19 Although there is no evidence, it is recommended to limit the depth of immersion for children.18
Thermoregulation-metabolismWhile diving, the body's energy consumption triples or quadruples to compensate for the cold, the physical effort, increased demands on the lungs and heart, and the stress associated with the aquatic setting.
Children are much more vulnerable to heat loss than adults because their weight to body surface area ratio is higher. This is usually due to a lower body fat percentage. Taking into consideration that hypothermia can alter cognitive functions, it is advisable that children wear adequate neoprene suits, avoid diving in colder waters and limit their immersion time.18
Central nervous systemDiving requires our central nervous system to adapt constantly, combining adequate neuroendocrine regulation to deal with the increase in energy needs and stress, with a cautious and proportional emotional response when facing an underwater setting that is potentially hostile and where the ability to respond is restricted.
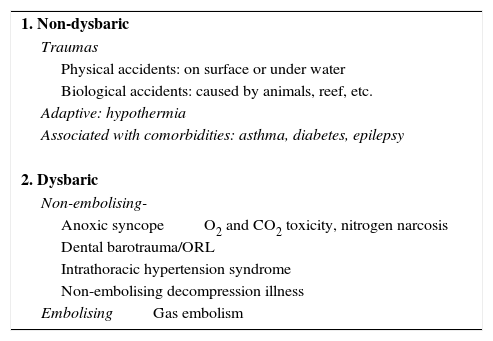
Diving accidentsRecreational diving involving children has a higher risk of accidents, even in shallow waters and swimming pools.20 The main causes of accidents are summarised in Table 2.
Causes for compressed-air diving accidents.
| 1. Non-dysbaric |
| Traumas |
| Physical accidents: on surface or under water |
| Biological accidents: caused by animals, reef, etc. |
| Adaptive: hypothermia |
| Associated with comorbidities: asthma, diabetes, epilepsy |
| 2. Dysbaric |
| Non-embolising- |
| Anoxic syncopeO2 and CO2 toxicity, nitrogen narcosis |
| Dental barotrauma/ORL |
| Intrathoracic hypertension syndrome |
| Non-embolising decompression illness |
| EmbolisingGas embolism |
It is difficult to determine the incidence of diving accidents due to the lack of prospective studies. Most of the data come from international notifications posted on the Divers Alert Network. It is estimated that the rate of fatal accidents ranges between 16–71/100,000 non-professional divers per year,21 and in children it is less than 3%.22 Most deaths involving children are caused by drowning or gas embolism. Some of the children/adolescents who have died had not even received a training course and many were performing high-risk immersions at great depth, in caves, or exploring sunken ships.23 Likewise, 50% of the diving accidents involved children with asthma, with a history of anxiety or with attention deficit hyperactivity disorder (ADHD), or children who made a quick ascent due to panic or O2 exhaustion.24
The only paediatric prospective study found was conducted on a sample of 205 children between the the ages of 8 and 13 years, with maximum immersions to a depth of between 5 and 10m and follow-up visits after five years.25 Four inner ear lesions and one hypoxic syncope caused by hyperventilation were observed. There were no alterations in their growth or hearing. However, these results must be interpreted with caution due to the high drop out rate (25%/year) and the bias of not including children with asthma, heart or neurological problems.
Diving accidents are classified depending on whether they are caused by pressure, or are dysbaric or non-dysbaric. Among non-dysbaric accidents, trauma, hypothermia and accidents associated with comorbidities are the most frequent. In compressed-air diving, dysbaric accidents include anoxic/hypoxic syncope, accidents associated with gas toxicity, otic/dental barotrauma, intrathoracic hypertension syndrome and decompression illness.
Anoxic syncope is a loss of consciousness during ascent in the course of prolonged immersions with apnoea. It is usually triggered by hypoxia and worsened by hyperventilation manoeuvres.
Gas toxicity. Severe oxygen toxicity is less frequent with the mixtures that are usually used in recreational diving. However, CO2 retention due to poor ventilation techniques can increase the risk of decompression illness. The risk of nitrogen narcosis increases with depth, and is negligible above 30m.
Otic barotrauma is triggered during descent or ascent due to an inadequate performance of compensation manoeuvres of the middle ear. Dental barotrauma occurs during ascent due to the expansion of the air retained in cavities or defective dental fillings.
Intrathoracic hypertension syndrome occurs during ascent, when the diver stops breathing or when exhalation is inadequate. When pressure decreases during ascent, the volume of air in the lungs increases and pneumomediastinum or pneumothorax can occur. It can be prevented by maintaining exhalation during the entire ascent and avoiding fast or uncontrolled ascents.
Decompression illness is defined as the group of symptoms and signs caused by the formation of inert gas bubbles in tissues due to inadequate decompression of the gases inhaled (mainly nitrogen) in a high-pressure environment. Bubbles can cause pruritus, erythema or pain due to tissue laceration at a subcutaneous or osseous cellular tissue level; or non-embolising neurological symptoms due to irritation or compression. They can also cause embolisation if they enter venous circulation, causing dyspnoea and retrosternal pain. If they reach the left cardiac cavities, they can cause arterial embolism with neurological clinical symptoms. Symptoms can appear a few minutes after coming out of the water or up to 12–24h later. They can even appear when diving at shallow depths, after immersions in swimming pools or after a first immersion.20,26 If decompression illness is suspected, initial treatment always consists of providing 100% oxygen with a bag-mask, and administering intravenous fluids to maintain perfusion and hydration. It is essential to organise an evacuation plan with immediate transfer to a centre with a hyperbaric chamber, avoiding referrals to secondary hospitals. Treatments with corticosteroids or anticoagulants have not proven to be beneficial and are not recommended.27,28 If the patient needs to be air-lifted, the maximum recommended height is 300m. In the case of ground transportation, roads with heights that exceed 300m should be avoided.
Recommendations for scuba diving in childrenGeneral indicationsThe lack of paediatric studies implies that most of the recommendations are based on experts’ opinions. In general, any pathology that predisposes to barotrauma, disorientation, worsening comorbidities or anxiety must be evaluated.
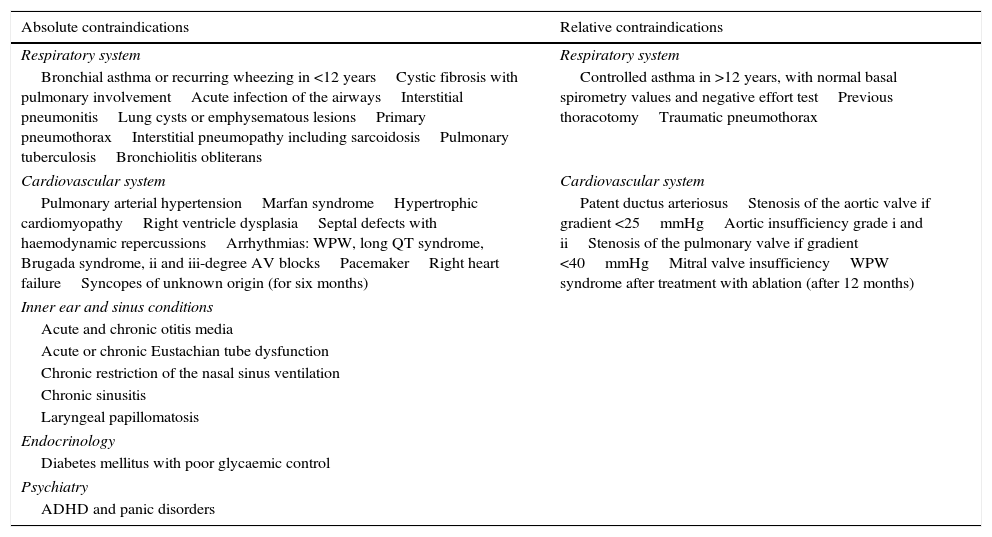
Medical indicationsMedical contraindications for scuba diving in children are listed in Table 3.
Medical contraindications for diving recommended for children and adolescents.
| Absolute contraindications | Relative contraindications |
|---|---|
| Respiratory system | Respiratory system |
| Bronchial asthma or recurring wheezing in <12 yearsCystic fibrosis with pulmonary involvementAcute infection of the airwaysInterstitial pneumonitisLung cysts or emphysematous lesionsPrimary pneumothoraxInterstitial pneumopathy including sarcoidosisPulmonary tuberculosisBronchiolitis obliterans | Controlled asthma in >12 years, with normal basal spirometry values and negative effort testPrevious thoracotomyTraumatic pneumothorax |
| Cardiovascular system | Cardiovascular system |
| Pulmonary arterial hypertensionMarfan syndromeHypertrophic cardiomyopathyRight ventricle dysplasiaSeptal defects with haemodynamic repercussionsArrhythmias: WPW, long QT syndrome, Brugada syndrome, ii and iii-degree AV blocksPacemakerRight heart failureSyncopes of unknown origin (for six months) | Patent ductus arteriosusStenosis of the aortic valve if gradient <25mmHgAortic insufficiency grade i and iiStenosis of the pulmonary valve if gradient <40mmHgMitral valve insufficiencyWPW syndrome after treatment with ablation (after 12 months) |
| Inner ear and sinus conditions | |
| Acute and chronic otitis media | |
| Acute or chronic Eustachian tube dysfunction | |
| Chronic restriction of the nasal sinus ventilation | |
| Chronic sinusitis | |
| Laryngeal papillomatosis | |
| Endocrinology | |
| Diabetes mellitus with poor glycaemic control | |
| Psychiatry | |
| ADHD and panic disorders | |
Nasal respiration, middle ear obstruction and adenoid hypertrophy must be assessed to ensure adequate ventilation.25 Absolute contraindications for diving are sinusitis, acute and chronic otitis media, and acute tubal ventilation disorders.29
Respiratory systemCystic adenomatoid malformations and pulmonary bullae constitute contraindications for diving, due to the high risk of pneumothorax. Likewise, recent pleural diseases must be evaluated: spontaneous pneumothorax is an absolute contraindication. If there is a history of pleural drainage, it is recommended to wait a minimum of six weeks.30
Asthma: In addition to the aforementioned decrease in pulmonary function after immersion,13,14 some published series show that asthma is a relatively common comorbidity in fatal accidents.24 Up to 50% of the children who needed treatment with a hyperbaric chamber after immersion had a history of asthma. Both results constitute absolute contraindications for diving for children under the age of 12 who suffer from asthma, and in general for all patients with a disease involving narrowing of the airways (cystic fibrosis, bronchiolitis obliterans and malacias, among others). According to the British Thoracic Society30 diving would be allowed in adults and children over the age of 12 with asthma as long as they have no symptoms, have normal basal spirometry values (FEV1>80% and FEV1/FVC ratio>70%) and a negative exercise test.
Diabetes mellitusPublished studies, however scarce, do not describe an increased risk in this group of patients.31 However, when at risk of hyperglycaemia during immersion, adequate glycaemic control and diving with a supervisor familiar with the disease must be ensured.
Patent foramen ovaleIt is not required to routinely rule out the existence of PFO prior to diving in all age groups. If it is known, it only represents an absolute contraindication when there is a significant shunt during spontaneous respiration32; but the existence of a higher risk of lesions in the case of a dysbaric accident must be made known.33
EpilepsyAccording to some authors, diving should only be undertaken if the child has not had any seizures for over four years with stable medication, if no sedative drugs are used and if the risks are adequately understood.34
Psychological abilitiesPsychological assessment is essential. The age of eight has been accepted as the lowest limit, since most children of that age have already acquired basic abilities for co-operation, concentration, self-control, logical thought, responsibility and risk awareness. However, psychological assessment must always be thorough and individualised, taking into account the following factors:
- •
Children get distracted more easily than adults, and are more likely to change their depth if something attracts their attention.
- •
They have a great sense of adventure, but lack of awareness regarding morbidity and risks. Their behaviour is more difficult to predict.
- •
Children use concrete thinking and they are less able to react adequately in situations that are different from those described by their instructors.
- •
There is no specific psychotechnical test to assess a child's ability to dive. Thus, a psychological evaluation must be carried out at every training stage.18
- •
It is important to establish that the child wants to dive, and is not doing so due to parental or peer pressure.3
The typical reduction in the ability to pay attention, hyperactivity and impulsiveness make this disorder incompatible with diving. In patients with ADHD there is an increased risk of decompression illness and ear and sinus problems.17
Ergonomic aspectsThe diving equipment must be adapted to the age and size of the child and must be checked regularly, adapting it to their growth:18 masks, flippers, suit and snorkel tank must be adequate for age and size; the regulator must be flexible and light, and small, lightweight tanks should be used.
RequirementsThe Spanish Federation of Underwater Activities (SFUA) regulates this activity nationally, usually following the standards of the World Confederation of Underwater Activities (WCUA).35
The training of children who want to dive follows a specific programme. The minimum age for diving has been set at 8 years. Between the ages of 8 and 14, the rules vary according to jurisdiction, and, from the age of 14, an adult programme is adopted. It is mandatory to have a medical certificate of fitness issued by a doctor trained in paediatric underwater medicine.9
Typical diving courses for children are35:
- •
Discovery activity (diving baptism): Minimal age is 8 years old. No medical certificate or national license is required. The maximum depth is 3m and no documentary proof is required.
- •
Beginners: Minimal age is also 8 years old. A medical certificate or national licence are not required, only proof of having performed a few compressed-air diving practices.
- •
Junior diver: At a national level, this requires children to be at least 12 years of age, although some regional variations are maintained. A medical certificate and national licence are required. This authorises immersion of up to 20m without decompression. The child must always be accompanied by a mentor diver.
The complete Spanish regulations and links to international standards can be found on the Spanish Federation of Underwater Activities webpage: www.fedas.es.
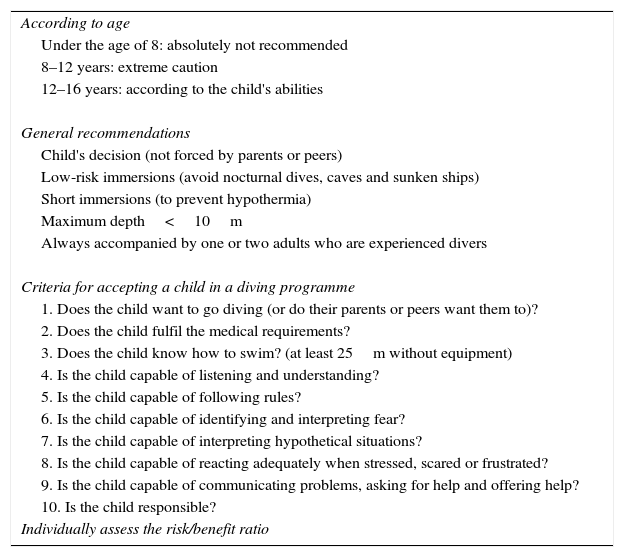
The recommendations for compressed-air diving at a paediatric age described in this review are summarised in Table 4 and have been endorsed by the Spanish Society of Paediatric Pulmonology. It is important to note that even when contraindications are not applicable and the corresponding medical evaluation has been performed, it is imperative that the child has the psychological abilities needed in diving.
Recommendations for underwater activities.
| According to age |
| Under the age of 8: absolutely not recommended |
| 8–12 years: extreme caution |
| 12–16 years: according to the child's abilities |
| General recommendations |
| Child's decision (not forced by parents or peers) |
| Low-risk immersions (avoid nocturnal dives, caves and sunken ships) |
| Short immersions (to prevent hypothermia) |
| Maximum depth<10m |
| Always accompanied by one or two adults who are experienced divers |
| Criteria for accepting a child in a diving programme |
| 1. Does the child want to go diving (or do their parents or peers want them to)? |
| 2. Does the child fulfil the medical requirements? |
| 3. Does the child know how to swim? (at least 25m without equipment) |
| 4. Is the child capable of listening and understanding? |
| 5. Is the child capable of following rules? |
| 6. Is the child capable of identifying and interpreting fear? |
| 7. Is the child capable of interpreting hypothetical situations? |
| 8. Is the child capable of reacting adequately when stressed, scared or frustrated? |
| 9. Is the child capable of communicating problems, asking for help and offering help? |
| 10. Is the child responsible? |
| Individually assess the risk/benefit ratio |
The authors declare that there are no conflicts of interest.
Please cite this article as: Cilveti R, Osona B, Peña JA, Moreno L, Asensio O, en representación del Grupo de Técnicas de la Sociedad Española de Neumología Pediátrica. Buceo en la edad pediátrica: fisiología, riesgos y recomendaciones. An Pediatr (Barc). 2015;83:410–416.