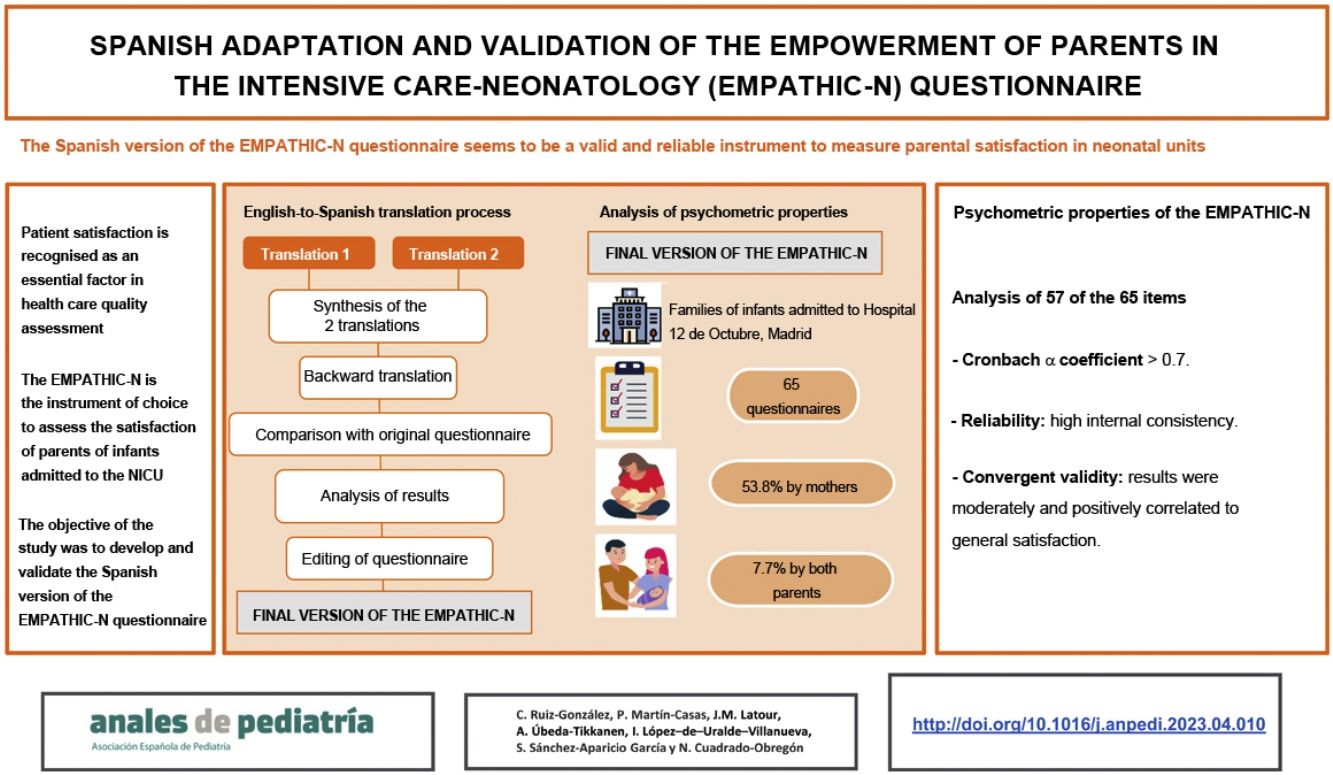
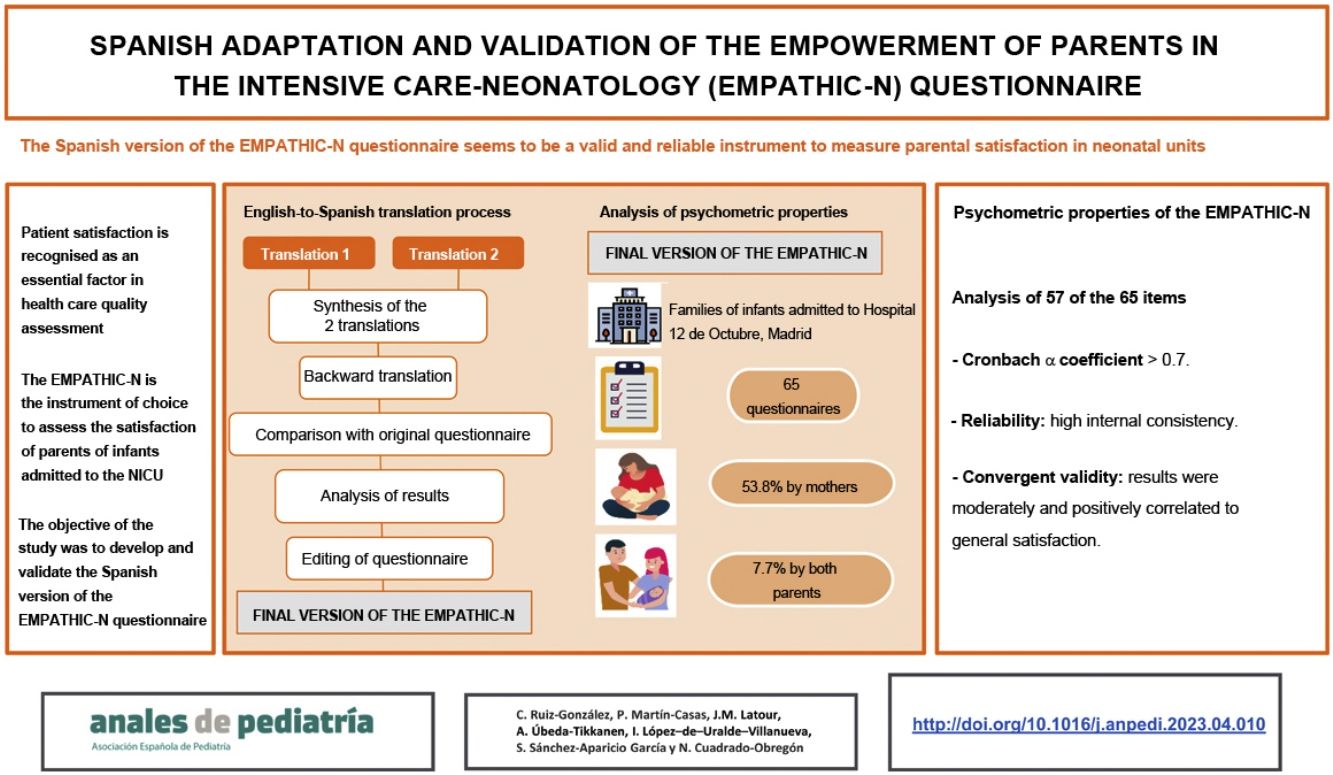
Parental satisfaction is rarely measured in the neonatal intensive care unit due to a lack of specific assessment tools. The Empowerment of Parents in The Intensive Care-Neonatology (EMPATHIC-N) questionnaire is an instrument to assess satisfaction in relation to family-centred care that has been validated in several countries, but not Spain.
ObjectivesTo perform the translation and cultural adaptation of the EMPATHIC-N to Spanish followed by its validation for the purpose of assessing satisfaction in parents with children admitted to the neonatal intensive care unit.
Material and methodsThe questionnaire first underwent forward and backward translation and transcultural adaptation by a panel of experts through a standardized process based on the Delphi method, followed by a pilot study in 8 parents and then a cross-sectional study in the neonatal intensive care unit of a tertiary care hospital to assess the reliability and converging validity of the Spanish version.
ResultsThe study proved the comprehensibility, validity, feasibility, applicability and usefulness of the Spanish version of the EMPATHIC-N in the field of paediatric health after being evaluated by 19 professionals and 60 parents. The content validity was found to be excellent (0.93). The reliability and convergent validity of the Spanish version of the EMPHATIC-N was analysed in a sample of 65 completed questionnaires. The Cronbach α for each domain was greater than 0.7, indicating a high internal consistency. We assessed validity by analysing the correlation of the 5 domains with the with the 4 general satisfaction items. The validity was found to be adequate (rs, 0.4−0.76; P < .01).
ConclusionsThe Spanish version of the EMPATHIC-N questionnaire is a comprehensible, useful, valid and reliable instrument to measure satisfaction in the parents of children admitted to neonatal care units.
La satisfacción de los padres de niños en Unidades de Cuidados Intensivos Neonatales (UCIN) apenas se evalúa por la carencia de herramientas específicas. El Empowerment of Parents in Tee Intensive Care Neonatology (EMPATHIC-N) es un cuestionario de satisfacción que evalúa los cuidados centrados en el desarrollo y la familia, validado en varios países pero no en España.
ObjetivosRealizar la adaptación y validación del EMPATHIC-N para la evaluación de la satisfacción de los padres de niños ingresados en UCIN.
Material y métodosPrimero, se realizó una traducción-retrotraducción y adaptación transcultural siguiendo un procedimiento estandarizado con un comité de expertos, mediante el método Delphi. Posteriormente, se realizó un estudio piloto con ocho padres y un estudio transversal en la unidad neonatal de un hospital terciario para analizar la fiabilidad y la validez convergente del cuestionario.
ResultadosLa versión española del EMPATHIC-N demostró su comprensibilidad, viabilidad, aplicabilidad y utilidad en el ámbito sanitario infantil, evaluado por 19 profesionales y 60 padres. Su validez de contenido global resultó excelente (0,93). La fiabilidad y validez convergente del EMPHATIC-N se analizaron en 65 encuestas. El α de Cronbach por dominios se situó por encima de 0,7, indicando una alta consistencia interna. La validez fue medida correlacionando los cinco dominios con los cuatro ítems de satisfacción general, demostrando una correlación adecuada (rs: 0,4–0,76; P < ,01).
ConclusionesLa versión española del cuestionario EMPATHIC-N es un instrumento comprensible, viable, aplicable, útil, válido y fiable para medir la satisfacción de los padres en las unidades neonatales.
Patient satisfaction is increasingly recognised as an important factor in the assessment of health care quality. At present, in the field of neonatal care, the family-centred developmental care (FCDC) approach is being implemented, defined by the World Health Organization as a broad category of interventions that is designed to minimize the physiological and neurological stress of infants in the neonatal intensive care unit (NICU) environment.1 Its goals are to optimise medical and neurobehavioural outcomes of infants and facilitate the active participation of the family in infant care. These interventions include the regulation of environmental stimuli (light, noise, humidity and temperature), appropriate infant positioning and handling, promoting sleep and recognising the family as a fundamental pillar in the hospital stay and life of the infant.1,2 The approach promotes practices such as skin-to-skin contact and the involvement of parents in patient care when their children are hospitalised in intensive care units, thus facilitating bonding before parents and the newborn.2
The implementation of FCDC does not only entail improvements in procedures, but also in the attitudes of health care workers in the care of children and their families.3 Thus, it is reasonable to expect an increase in parental satisfaction in units that apply this approach, as one of the core principles of FCDC is parental participation. There is also evidence that the satisfaction of the family increases if there is closer collaboration between parents and the health care team, in addition to a significant reduction in the length of stay, when parents are involved in infant care.4
Since parental perceptions are very relevant in the evaluation and improvement of interventions performed in children,5 assessing parental experiences and satisfaction is key to improve care delivery in the NICU on a day-to-day basis. Validated instruments are needed to collect data on the perception of family members during the NICU stay in order to compare and optimise FCDC models from a broader perspective,5–7 and to empower them in current NICU care delivery. Few validated instruments are available to assess parental satisfaction in this care setting that address every principle of FCDC: respect, information and education for parents, care coordination, physical and emotional support and parental involvement.4 Most were developed before the implementation of FCDC models in the NICU setting. Other instruments used in the past only assessed parental stress and did not consider parental satisfaction. Still, satisfaction is not the same as absence of stress.7,8
Based on recent studies,4 the EMpowerment of PArents in THe Intensive Care Neonatology (EMPATHIC-N) questionnaire, developed by Latour et al.,9 is the instrument of choice to measure the satisfaction of parents of infants admitted to the NICU, as it assesses a broad range of practices that are important in neonatal intensive care.4,10 It was developed in a 30-bed NICU in the Netherlands and has exhibited good reliability and validity,9,11 and, while the version used in the validation study was in Dutch, the authors have also made an English version available to other working groups. This version was used for adaptation and translation of the instrument for the Brazilian population12 in a study involving forward and back translation and transcultural adaptation involving a group of 55 experts and 2 successive groups of 8 and 5 mothers to assess its comprehensibility. The validation of the instrument in Ethiopia10 also involved translation of the English version to two local languages in a multicentre study conducted in 3 hospitals in a sample of 386 completed questionnaires, which allowed not only to analyse the psychometric properties of the instrument, but also identify differences in parental satisfaction in relation to parental educational attainment and place of residence, the length of stay and levels of care. The authors also added open-ended questions to collect comments or suggestions from parents and identify the main themes they brought up.
The EMPATHIC-N has not been translated to Spanish nor a Spanish version validated, so the aim of the study was to develop and validate the Spanish version of the EMPHATIC-N.
Material and methodsThe EMPATHIC-N comprises a total of 65 items, of which 57 focus on neonatal intensive care practices, structured into five domains: information, care and treatment, parental participation, organization and professional attitude. Each item is rated on a 6-point scale ranging from 1 (certainly no) to 6 (certainly yes) with an additional “not applicable” option (Appendix B).9 There are 2 demographic information items about the individual who is completing the questionnaire and their cultural background, 2 general items about the overall care episode10-point rating scale) and 4 open questions about the unit and hospital stay and the overall experience during the care episode.9
The forward translation, back translation and transcultural adaptation of the questionnaire adhered to the recommendations of the International Society for Pharmacoeconomics and Outcomes Research (ISPOR).13 The content validity of the translated version in Spanish14 was assessed by a panel of experts using the Delphi method.15 There were 2 rounds of questions, and the answers were used to calculate the content validity index for the item (I-CVI) and the total scale (S-CVI)16 and the probability of random agreement (pe), which reflects the probability that the interrater agreement observed in a given number of experts about the relevance of a given item is due to chance.17
At this point, we obtained the approval of the Ethics Committee of the Hospital 12 de Octubre in Madrid, Spain, to conduct an observational study of the questionnaire to assess its reliability and validity. We started by carrying out a pilot study with a print version of the questionnaire to assess comprehension in 8 parents, applying the methodology described by the authors of the original questionnaire,9,13 also used in the Ethiopian validation study.10 For the analysis of psychometric properties, we estimated that we needed a minimum sample of 59 for an α level of 0.05% and a power of 80% to detect a correlation coefficient of 0.40 or higher, assuming losses of 20%. We recruited parents of infants hospitalised in the NICU by consecutive convenience sampling until achieving a sample size of 60 parents. We included parents whose children stayed in the NICU or intermediate care unit (IMCU) for at least 24 h and who signed the informed consent form. We excluded parents of infants who died in the NICU or IMCU or required readmission as well as those who could not understand Spanish.
The statistical analysis was performed with the software SPSS version 22.0 (IBM Corp, Armonk, NY, USA). In the descriptive analysis, we calculated absolute frequencies and percentages for qualitative variables. For quantitative variables, we calculated the mean and standard deviation (SD) and median and interquartile range (IQR). For the descriptive analysis of expert responses and panel results we calculated absolute frequencies and percentages for qualitative variables, and the mean and range for quantitative variables. We calculated the S-CVI based on the arithmetic mean of the I-CVI for items given ratings of 3 or 4 points by the experts. We calculated the probability of random agreement (pe) with the following formula: pc = 0.5N.14 We assessed the reliability of the translated questionnaire by means of the Cronbach α, with values greater than 0.7 indicating adequate internal consistency. The assessed convergent validity by means of the Spearman correlation coefficient, comparing the scores for each of the 5 domains and the 4 general satisfaction items. Values of 0.4 to 0.7 indicate a moderate correlation and values greater than 0.7 a strong correlation. In all the analysis, we considered P values of less than .05 statistically significant.
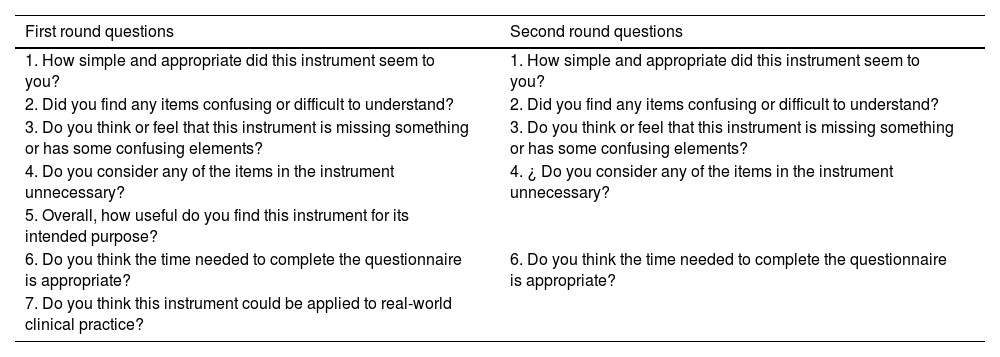
ResultsAfter obtaining permission from the authors of the original questionnaire, the latter was translated to Spanish and back translated9,13 with the standard procedure, giving rise to the preliminary draft of the EMPATHIC-N in Spanish (Appendix A). The main issues that arose had to do with specific terms and were resolved by consensus. The next step was the formation of the expert panel, for which we invited 22 professionals, of who only 13 agreed to participate; 9 more experts were invited in a second recruitment round, of who 6 accepted. Thus, the panel included 19 experts, of who 6 were nurses, 5 physical therapists, 3 physiatrists, 2 neonatologists and 2 occupational therapists, with a mean age of 44 years (range, 33–60), of who 89.4% were female. As for the response rate, 100% of the experts responded in the first round, while 18 (94.7%) completed the 2 rounds needed to achieve absolute consensus (Table 1).
Short-answer questions posed to experts.
| First round questions | Second round questions |
|---|---|
| 1. How simple and appropriate did this instrument seem to you? | 1. How simple and appropriate did this instrument seem to you? |
| 2. Did you find any items confusing or difficult to understand? | 2. Did you find any items confusing or difficult to understand? |
| 3. Do you think or feel that this instrument is missing something or has some confusing elements? | 3. Do you think or feel that this instrument is missing something or has some confusing elements? |
| 4. Do you consider any of the items in the instrument unnecessary? | 4. ¿ Do you consider any of the items in the instrument unnecessary? |
| 5. Overall, how useful do you find this instrument for its intended purpose? | |
| 6. Do you think the time needed to complete the questionnaire is appropriate? | 6. Do you think the time needed to complete the questionnaire is appropriate? |
| 7. Do you think this instrument could be applied to real-world clinical practice? |
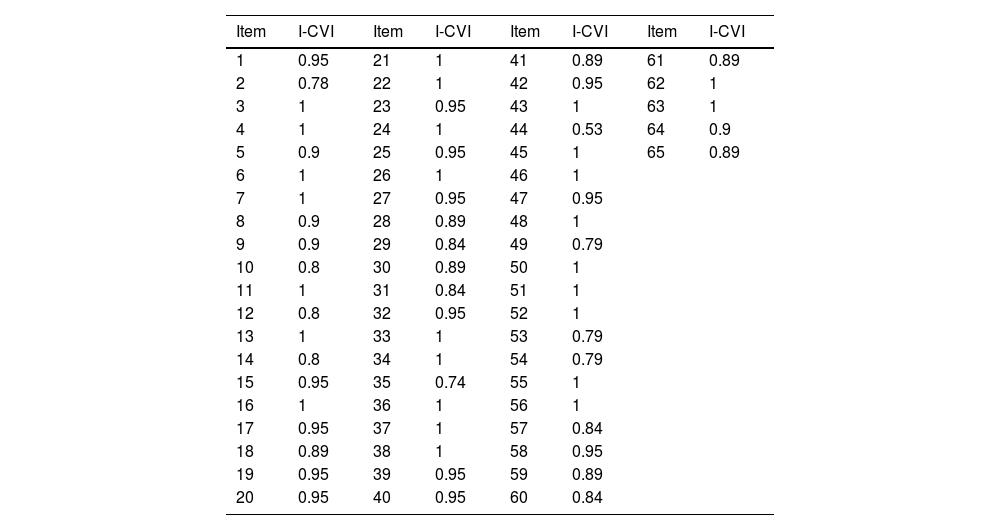
The I-CVI values were greater than 0.8 for most items, and only items 35, 53 and 54 had indices between 0.7 and 0.8 and item 44 an index of 0.53 (Table 2). The S-CVI for the overall questionnaire was 0.93. The probability of random agreement (pe) was 1.9 × 10−5, meaning that the probability of interrater agreement due to chance in the panel of 19 experts was close to zero. These results show that the Spanish version of the EMPATHIC-N has an excellent content validity. In addition, the experts proposed different modifications, such as including items to assess rehabilitation services, consolidating items and eliminating those with the lowest I-CVI values, but on consultation, the author of the original instrument indicated that the analysis of its psychometric properties had to be conducted on an instrument including the original items. The pilot study confirmed that the Spanish version was comprehensible and feasible for parents, as it required a mean of 12 min to fill out and perceived as clear, understandable and easy to complete.
Item content validity indices.
| Item | I-CVI | Item | I-CVI | Item | I-CVI | Item | I-CVI |
|---|---|---|---|---|---|---|---|
| 1 | 0.95 | 21 | 1 | 41 | 0.89 | 61 | 0.89 |
| 2 | 0.78 | 22 | 1 | 42 | 0.95 | 62 | 1 |
| 3 | 1 | 23 | 0.95 | 43 | 1 | 63 | 1 |
| 4 | 1 | 24 | 1 | 44 | 0.53 | 64 | 0.9 |
| 5 | 0.9 | 25 | 0.95 | 45 | 1 | 65 | 0.89 |
| 6 | 1 | 26 | 1 | 46 | 1 | ||
| 7 | 1 | 27 | 0.95 | 47 | 0.95 | ||
| 8 | 0.9 | 28 | 0.89 | 48 | 1 | ||
| 9 | 0.9 | 29 | 0.84 | 49 | 0.79 | ||
| 10 | 0.8 | 30 | 0.89 | 50 | 1 | ||
| 11 | 1 | 31 | 0.84 | 51 | 1 | ||
| 12 | 0.8 | 32 | 0.95 | 52 | 1 | ||
| 13 | 1 | 33 | 1 | 53 | 0.79 | ||
| 14 | 0.8 | 34 | 1 | 54 | 0.79 | ||
| 15 | 0.95 | 35 | 0.74 | 55 | 1 | ||
| 16 | 1 | 36 | 1 | 56 | 1 | ||
| 17 | 0.95 | 37 | 1 | 57 | 0.84 | ||
| 18 | 0.89 | 38 | 1 | 58 | 0.95 | ||
| 19 | 0.95 | 39 | 0.95 | 59 | 0.89 | ||
| 20 | 0.95 | 40 | 0.95 | 60 | 0.84 |
I-CVI, item content validity index.
For the analysis of its psychometric properties, we collected a total of 60 questionnaires completed by 35 mothers (53.8%) and 25 fathers (38.5%), in addition to 5 questionnaires completed by both parents (7.7%). As for the ethnic background of the family, 54 were of European ancestry (83.1%), 9 were Latin American (13.8%) and 2 parents reported other regions of origin, Asian or Middle Eastern (3.1%). The median length of stay in the neonatal unit was 18 days (4–93 days); 22 infants were in the NICU (33.9%) and 43 in the IMCU (66.1%). Seventeen babies stayed in individual rooms (26.2%) and 9 received mechanical ventilation (13.8%).
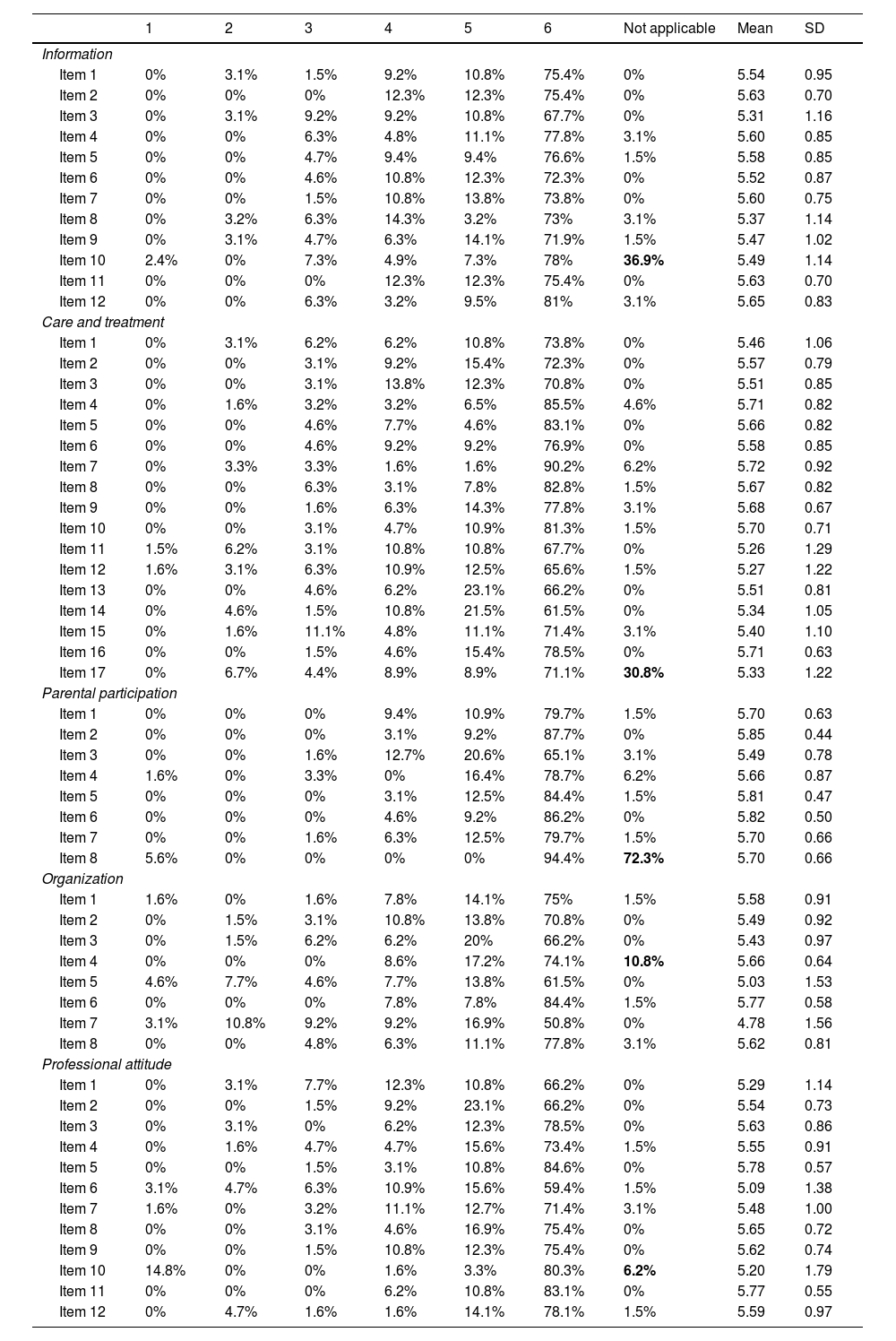
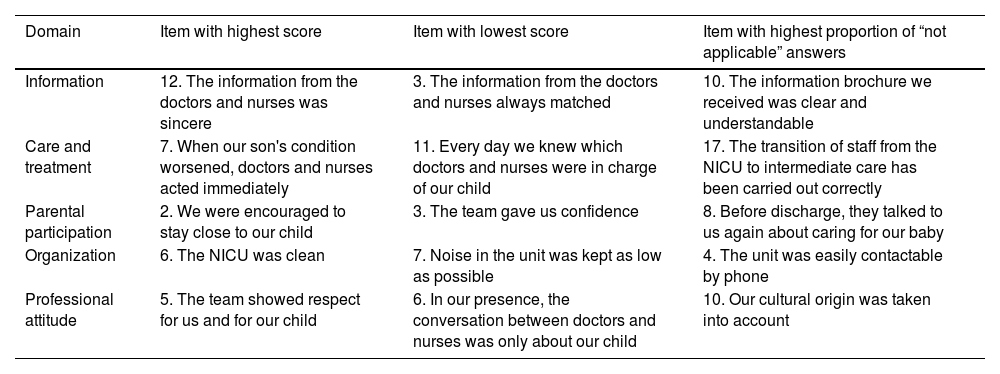
Table 3 presents the results of the questionnaires completed by the parents, and Table 4 summarises the results for each of the questionnaire domains, presenting the items with the highest and lowest scores, in addition to those with the highest proportion of “not applicable” answers. The items with the highest proportion of not applicable answers were those concerning the informational brochure (“El folleto de información que recibimos era claro y comprensible”), the handover of the patient from the NICU to the IMCU (“El paso del personal de la NICU a cuidados intermedios se ha desarrollado correctamente”) and the item regarding the information provided about infant care before discharge (“Antes del alta, volvieron a hablar con nosotros sobre el cuidado de nuestro bebé”). The mean score for each of the 57 items was greater than 5 (5.54), with the exception of item 7 in the organization domain regarding noise mitigation in the unit, with a mean of 4.78(SD, 1.56).
Percentage of answers for the item given a specific score, and mean score for each item in the Spanish version of the EMPHATIC-N.
| 1 | 2 | 3 | 4 | 5 | 6 | Not applicable | Mean | SD | |
|---|---|---|---|---|---|---|---|---|---|
| Information | |||||||||
| Item 1 | 0% | 3.1% | 1.5% | 9.2% | 10.8% | 75.4% | 0% | 5.54 | 0.95 |
| Item 2 | 0% | 0% | 0% | 12.3% | 12.3% | 75.4% | 0% | 5.63 | 0.70 |
| Item 3 | 0% | 3.1% | 9.2% | 9.2% | 10.8% | 67.7% | 0% | 5.31 | 1.16 |
| Item 4 | 0% | 0% | 6.3% | 4.8% | 11.1% | 77.8% | 3.1% | 5.60 | 0.85 |
| Item 5 | 0% | 0% | 4.7% | 9.4% | 9.4% | 76.6% | 1.5% | 5.58 | 0.85 |
| Item 6 | 0% | 0% | 4.6% | 10.8% | 12.3% | 72.3% | 0% | 5.52 | 0.87 |
| Item 7 | 0% | 0% | 1.5% | 10.8% | 13.8% | 73.8% | 0% | 5.60 | 0.75 |
| Item 8 | 0% | 3.2% | 6.3% | 14.3% | 3.2% | 73% | 3.1% | 5.37 | 1.14 |
| Item 9 | 0% | 3.1% | 4.7% | 6.3% | 14.1% | 71.9% | 1.5% | 5.47 | 1.02 |
| Item 10 | 2.4% | 0% | 7.3% | 4.9% | 7.3% | 78% | 36.9% | 5.49 | 1.14 |
| Item 11 | 0% | 0% | 0% | 12.3% | 12.3% | 75.4% | 0% | 5.63 | 0.70 |
| Item 12 | 0% | 0% | 6.3% | 3.2% | 9.5% | 81% | 3.1% | 5.65 | 0.83 |
| Care and treatment | |||||||||
| Item 1 | 0% | 3.1% | 6.2% | 6.2% | 10.8% | 73.8% | 0% | 5.46 | 1.06 |
| Item 2 | 0% | 0% | 3.1% | 9.2% | 15.4% | 72.3% | 0% | 5.57 | 0.79 |
| Item 3 | 0% | 0% | 3.1% | 13.8% | 12.3% | 70.8% | 0% | 5.51 | 0.85 |
| Item 4 | 0% | 1.6% | 3.2% | 3.2% | 6.5% | 85.5% | 4.6% | 5.71 | 0.82 |
| Item 5 | 0% | 0% | 4.6% | 7.7% | 4.6% | 83.1% | 0% | 5.66 | 0.82 |
| Item 6 | 0% | 0% | 4.6% | 9.2% | 9.2% | 76.9% | 0% | 5.58 | 0.85 |
| Item 7 | 0% | 3.3% | 3.3% | 1.6% | 1.6% | 90.2% | 6.2% | 5.72 | 0.92 |
| Item 8 | 0% | 0% | 6.3% | 3.1% | 7.8% | 82.8% | 1.5% | 5.67 | 0.82 |
| Item 9 | 0% | 0% | 1.6% | 6.3% | 14.3% | 77.8% | 3.1% | 5.68 | 0.67 |
| Item 10 | 0% | 0% | 3.1% | 4.7% | 10.9% | 81.3% | 1.5% | 5.70 | 0.71 |
| Item 11 | 1.5% | 6.2% | 3.1% | 10.8% | 10.8% | 67.7% | 0% | 5.26 | 1.29 |
| Item 12 | 1.6% | 3.1% | 6.3% | 10.9% | 12.5% | 65.6% | 1.5% | 5.27 | 1.22 |
| Item 13 | 0% | 0% | 4.6% | 6.2% | 23.1% | 66.2% | 0% | 5.51 | 0.81 |
| Item 14 | 0% | 4.6% | 1.5% | 10.8% | 21.5% | 61.5% | 0% | 5.34 | 1.05 |
| Item 15 | 0% | 1.6% | 11.1% | 4.8% | 11.1% | 71.4% | 3.1% | 5.40 | 1.10 |
| Item 16 | 0% | 0% | 1.5% | 4.6% | 15.4% | 78.5% | 0% | 5.71 | 0.63 |
| Item 17 | 0% | 6.7% | 4.4% | 8.9% | 8.9% | 71.1% | 30.8% | 5.33 | 1.22 |
| Parental participation | |||||||||
| Item 1 | 0% | 0% | 0% | 9.4% | 10.9% | 79.7% | 1.5% | 5.70 | 0.63 |
| Item 2 | 0% | 0% | 0% | 3.1% | 9.2% | 87.7% | 0% | 5.85 | 0.44 |
| Item 3 | 0% | 0% | 1.6% | 12.7% | 20.6% | 65.1% | 3.1% | 5.49 | 0.78 |
| Item 4 | 1.6% | 0% | 3.3% | 0% | 16.4% | 78.7% | 6.2% | 5.66 | 0.87 |
| Item 5 | 0% | 0% | 0% | 3.1% | 12.5% | 84.4% | 1.5% | 5.81 | 0.47 |
| Item 6 | 0% | 0% | 0% | 4.6% | 9.2% | 86.2% | 0% | 5.82 | 0.50 |
| Item 7 | 0% | 0% | 1.6% | 6.3% | 12.5% | 79.7% | 1.5% | 5.70 | 0.66 |
| Item 8 | 5.6% | 0% | 0% | 0% | 0% | 94.4% | 72.3% | 5.70 | 0.66 |
| Organization | |||||||||
| Item 1 | 1.6% | 0% | 1.6% | 7.8% | 14.1% | 75% | 1.5% | 5.58 | 0.91 |
| Item 2 | 0% | 1.5% | 3.1% | 10.8% | 13.8% | 70.8% | 0% | 5.49 | 0.92 |
| Item 3 | 0% | 1.5% | 6.2% | 6.2% | 20% | 66.2% | 0% | 5.43 | 0.97 |
| Item 4 | 0% | 0% | 0% | 8.6% | 17.2% | 74.1% | 10.8% | 5.66 | 0.64 |
| Item 5 | 4.6% | 7.7% | 4.6% | 7.7% | 13.8% | 61.5% | 0% | 5.03 | 1.53 |
| Item 6 | 0% | 0% | 0% | 7.8% | 7.8% | 84.4% | 1.5% | 5.77 | 0.58 |
| Item 7 | 3.1% | 10.8% | 9.2% | 9.2% | 16.9% | 50.8% | 0% | 4.78 | 1.56 |
| Item 8 | 0% | 0% | 4.8% | 6.3% | 11.1% | 77.8% | 3.1% | 5.62 | 0.81 |
| Professional attitude | |||||||||
| Item 1 | 0% | 3.1% | 7.7% | 12.3% | 10.8% | 66.2% | 0% | 5.29 | 1.14 |
| Item 2 | 0% | 0% | 1.5% | 9.2% | 23.1% | 66.2% | 0% | 5.54 | 0.73 |
| Item 3 | 0% | 3.1% | 0% | 6.2% | 12.3% | 78.5% | 0% | 5.63 | 0.86 |
| Item 4 | 0% | 1.6% | 4.7% | 4.7% | 15.6% | 73.4% | 1.5% | 5.55 | 0.91 |
| Item 5 | 0% | 0% | 1.5% | 3.1% | 10.8% | 84.6% | 0% | 5.78 | 0.57 |
| Item 6 | 3.1% | 4.7% | 6.3% | 10.9% | 15.6% | 59.4% | 1.5% | 5.09 | 1.38 |
| Item 7 | 1.6% | 0% | 3.2% | 11.1% | 12.7% | 71.4% | 3.1% | 5.48 | 1.00 |
| Item 8 | 0% | 0% | 3.1% | 4.6% | 16.9% | 75.4% | 0% | 5.65 | 0.72 |
| Item 9 | 0% | 0% | 1.5% | 10.8% | 12.3% | 75.4% | 0% | 5.62 | 0.74 |
| Item 10 | 14.8% | 0% | 0% | 1.6% | 3.3% | 80.3% | 6.2% | 5.20 | 1.79 |
| Item 11 | 0% | 0% | 0% | 6.2% | 10.8% | 83.1% | 0% | 5.77 | 0.55 |
| Item 12 | 0% | 4.7% | 1.6% | 1.6% | 14.1% | 78.1% | 1.5% | 5.59 | 0.97 |
SD, standard deviation.
Items with highest percentage of “not applicable” answers are presented in boldface.
Summary of the results for the different domains of the Spanish version of the EMPHATIC-N.
| Domain | Item with highest score | Item with lowest score | Item with highest proportion of “not applicable” answers |
|---|---|---|---|
| Information | 12. The information from the doctors and nurses was sincere | 3. The information from the doctors and nurses always matched | 10. The information brochure we received was clear and understandable |
| Care and treatment | 7. When our son's condition worsened, doctors and nurses acted immediately | 11. Every day we knew which doctors and nurses were in charge of our child | 17. The transition of staff from the NICU to intermediate care has been carried out correctly |
| Parental participation | 2. We were encouraged to stay close to our child | 3. The team gave us confidence | 8. Before discharge, they talked to us again about caring for our baby |
| Organization | 6. The NICU was clean | 7. Noise in the unit was kept as low as possible | 4. The unit was easily contactable by phone |
| Professional attitude | 5. The team showed respect for us and for our child | 6. In our presence, the conversation between doctors and nurses was only about our child | 10. Our cultural origin was taken into account |
NICU, neonatal intensive care unit.
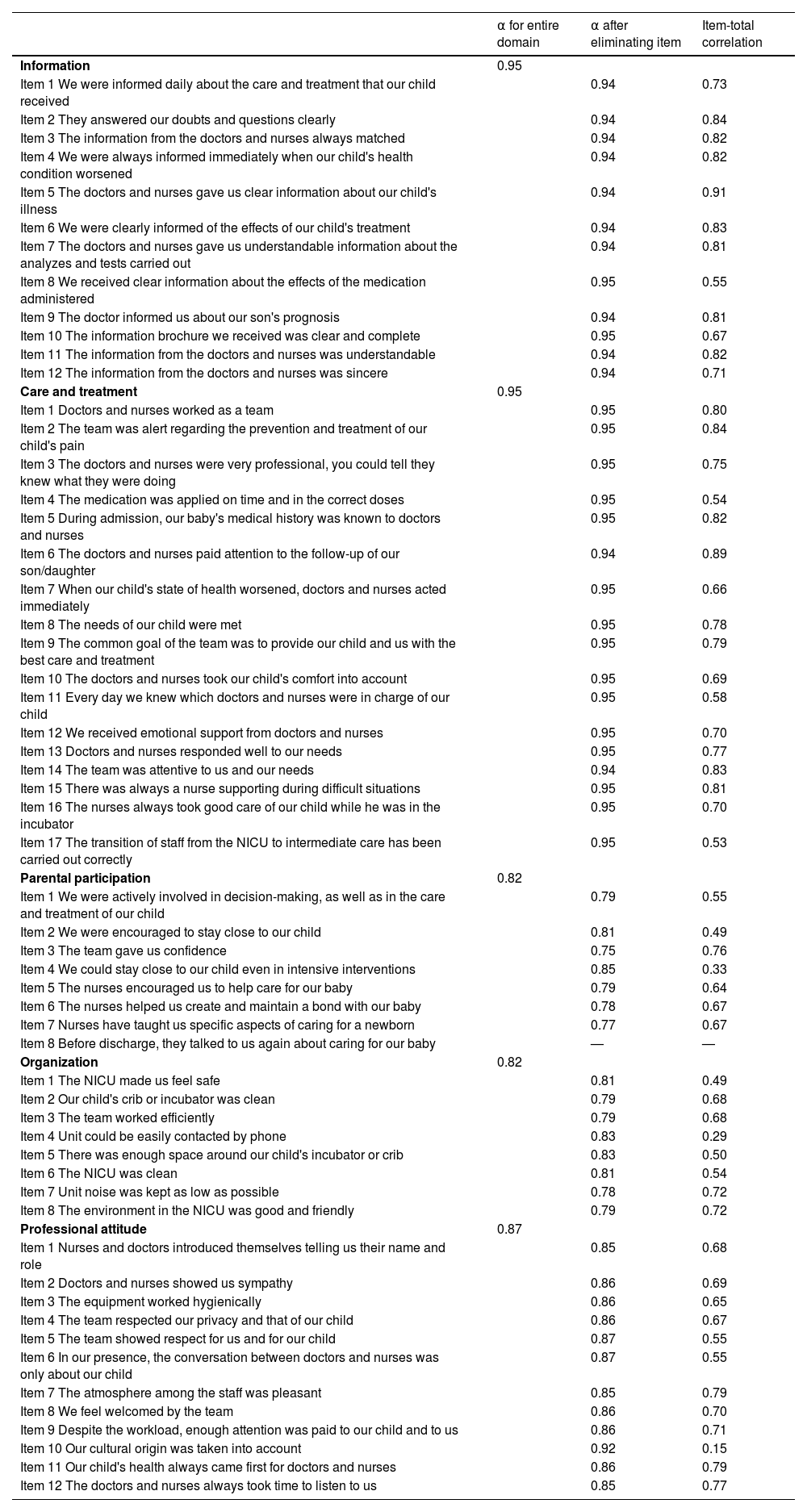
Table 5 presents the Cronbach α coefficient obtained by domain. The estimated reliability of the questionnaire for each dimension was fairly uniform, with values ranging from 0.82 (parental participation and organization domains) and 0.95 (information and care and treatment domains). The value for the professional attitude domain was 0.87, which indicates a high overall internal consistency for the EMPATHIC-N questionnaire.
Internal consistency of the Spanish version of the EMPATHIC-N.
| α for entire domain | α after eliminating item | Item-total correlation | |
|---|---|---|---|
| Information | 0.95 | ||
| Item 1 We were informed daily about the care and treatment that our child received | 0.94 | 0.73 | |
| Item 2 They answered our doubts and questions clearly | 0.94 | 0.84 | |
| Item 3 The information from the doctors and nurses always matched | 0.94 | 0.82 | |
| Item 4 We were always informed immediately when our child's health condition worsened | 0.94 | 0.82 | |
| Item 5 The doctors and nurses gave us clear information about our child's illness | 0.94 | 0.91 | |
| Item 6 We were clearly informed of the effects of our child's treatment | 0.94 | 0.83 | |
| Item 7 The doctors and nurses gave us understandable information about the analyzes and tests carried out | 0.94 | 0.81 | |
| Item 8 We received clear information about the effects of the medication administered | 0.95 | 0.55 | |
| Item 9 The doctor informed us about our son's prognosis | 0.94 | 0.81 | |
| Item 10 The information brochure we received was clear and complete | 0.95 | 0.67 | |
| Item 11 The information from the doctors and nurses was understandable | 0.94 | 0.82 | |
| Item 12 The information from the doctors and nurses was sincere | 0.94 | 0.71 | |
| Care and treatment | 0.95 | ||
| Item 1 Doctors and nurses worked as a team | 0.95 | 0.80 | |
| Item 2 The team was alert regarding the prevention and treatment of our child's pain | 0.95 | 0.84 | |
| Item 3 The doctors and nurses were very professional, you could tell they knew what they were doing | 0.95 | 0.75 | |
| Item 4 The medication was applied on time and in the correct doses | 0.95 | 0.54 | |
| Item 5 During admission, our baby's medical history was known to doctors and nurses | 0.95 | 0.82 | |
| Item 6 The doctors and nurses paid attention to the follow-up of our son/daughter | 0.94 | 0.89 | |
| Item 7 When our child's state of health worsened, doctors and nurses acted immediately | 0.95 | 0.66 | |
| Item 8 The needs of our child were met | 0.95 | 0.78 | |
| Item 9 The common goal of the team was to provide our child and us with the best care and treatment | 0.95 | 0.79 | |
| Item 10 The doctors and nurses took our child's comfort into account | 0.95 | 0.69 | |
| Item 11 Every day we knew which doctors and nurses were in charge of our child | 0.95 | 0.58 | |
| Item 12 We received emotional support from doctors and nurses | 0.95 | 0.70 | |
| Item 13 Doctors and nurses responded well to our needs | 0.95 | 0.77 | |
| Item 14 The team was attentive to us and our needs | 0.94 | 0.83 | |
| Item 15 There was always a nurse supporting during difficult situations | 0.95 | 0.81 | |
| Item 16 The nurses always took good care of our child while he was in the incubator | 0.95 | 0.70 | |
| Item 17 The transition of staff from the NICU to intermediate care has been carried out correctly | 0.95 | 0.53 | |
| Parental participation | 0.82 | ||
| Item 1 We were actively involved in decision-making, as well as in the care and treatment of our child | 0.79 | 0.55 | |
| Item 2 We were encouraged to stay close to our child | 0.81 | 0.49 | |
| Item 3 The team gave us confidence | 0.75 | 0.76 | |
| Item 4 We could stay close to our child even in intensive interventions | 0.85 | 0.33 | |
| Item 5 The nurses encouraged us to help care for our baby | 0.79 | 0.64 | |
| Item 6 The nurses helped us create and maintain a bond with our baby | 0.78 | 0.67 | |
| Item 7 Nurses have taught us specific aspects of caring for a newborn | 0.77 | 0.67 | |
| Item 8 Before discharge, they talked to us again about caring for our baby | — | — | |
| Organization | 0.82 | ||
| Item 1 The NICU made us feel safe | 0.81 | 0.49 | |
| Item 2 Our child's crib or incubator was clean | 0.79 | 0.68 | |
| Item 3 The team worked efficiently | 0.79 | 0.68 | |
| Item 4 Unit could be easily contacted by phone | 0.83 | 0.29 | |
| Item 5 There was enough space around our child's incubator or crib | 0.83 | 0.50 | |
| Item 6 The NICU was clean | 0.81 | 0.54 | |
| Item 7 Unit noise was kept as low as possible | 0.78 | 0.72 | |
| Item 8 The environment in the NICU was good and friendly | 0.79 | 0.72 | |
| Professional attitude | 0.87 | ||
| Item 1 Nurses and doctors introduced themselves telling us their name and role | 0.85 | 0.68 | |
| Item 2 Doctors and nurses showed us sympathy | 0.86 | 0.69 | |
| Item 3 The equipment worked hygienically | 0.86 | 0.65 | |
| Item 4 The team respected our privacy and that of our child | 0.86 | 0.67 | |
| Item 5 The team showed respect for us and for our child | 0.87 | 0.55 | |
| Item 6 In our presence, the conversation between doctors and nurses was only about our child | 0.87 | 0.55 | |
| Item 7 The atmosphere among the staff was pleasant | 0.85 | 0.79 | |
| Item 8 We feel welcomed by the team | 0.86 | 0.70 | |
| Item 9 Despite the workload, enough attention was paid to our child and to us | 0.86 | 0.71 | |
| Item 10 Our cultural origin was taken into account | 0.92 | 0.15 | |
| Item 11 Our child's health always came first for doctors and nurses | 0.86 | 0.79 | |
| Item 12 The doctors and nurses always took time to listen to us | 0.85 | 0.77 |
NICU, neonatal intensive care unit.
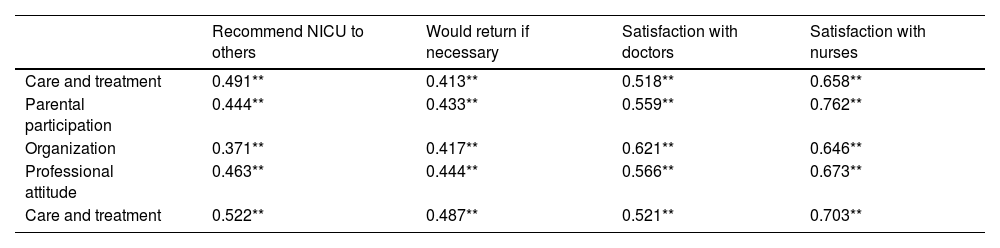
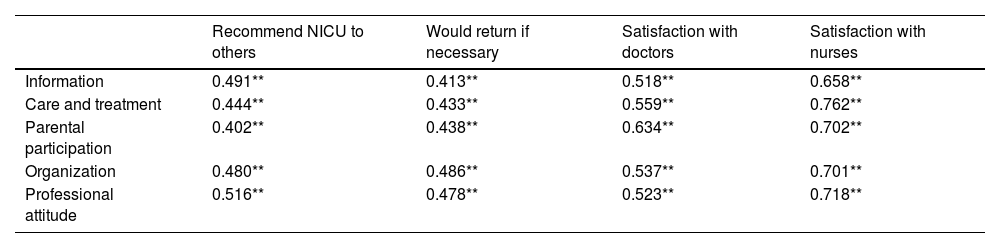
We assessed the convergent validity of the questionnaire by analysing the correlation between each of the five domains and the four general satisfaction items, with a separate analysis of the correlations obtained removing item 8 of the parental participation due to a high proportion of “not applicable” answers (Table 6), and the correlations obtained after removing the 3 problematic items identified in the internal consistency analysis of the questionnaire: item 4 in the parental participation domain concerning the ability to stay by the child even during intensive care interventions (“Podíamos permanecer cerca de nuestro hijo/a incluso en intervenciones intensivas”), item 4 in the organization domain regarding telephonic contact with the unit (“Se podía contactar fácilmente por teléfono con la unidad”) and item 10 in the professional attitude domain about taking into account the family’s cultural background (“Nuestro origen cultural se tuvo en cuenta”) (Table 7). In both cases, the domain with the weakest correlation with general satisfaction was the parental participation domain (0.371 and 0.402). Still, the results showed a moderate positive correlation. The mean scores for the items “I would recommend this NICU to other people” and “I would come back to this unit if it were necessary” were 5.77 (SD, 0.63) and 5.75 (SD, 0.63), respectively. The mean scores for the general satisfaction with doctors and nurses was 9.17 (SD, 1.64) and 9.3 (SD, 1.14), respectively.
Convergent validity of the different domains and general satisfaction after eliminating item 8 of parental participation on receiving information on infant care at the time of discharge (“Antes del alta, volvieron a hablar con nosotros sobre el cuidado de nuestro bebé”).
| Recommend NICU to others | Would return if necessary | Satisfaction with doctors | Satisfaction with nurses | |
|---|---|---|---|---|
| Care and treatment | 0.491** | 0.413** | 0.518** | 0.658** |
| Parental participation | 0.444** | 0.433** | 0.559** | 0.762** |
| Organization | 0.371** | 0.417** | 0.621** | 0.646** |
| Professional attitude | 0.463** | 0.444** | 0.566** | 0.673** |
| Care and treatment | 0.522** | 0.487** | 0.521** | 0.703** |
NICU, neonatal intensive care unit.
Convergent validity of the different domains and general satisfaction after eliminating the problematic items identified in the internal consistency analysis.
| Recommend NICU to others | Would return if necessary | Satisfaction with doctors | Satisfaction with nurses | |
|---|---|---|---|---|
| Information | 0.491** | 0.413** | 0.518** | 0.658** |
| Care and treatment | 0.444** | 0.433** | 0.559** | 0.762** |
| Parental participation | 0.402** | 0.438** | 0.634** | 0.702** |
| Organization | 0.480** | 0.486** | 0.537** | 0.701** |
| Professional attitude | 0.516** | 0.478** | 0.523** | 0.718** |
NICU, neonatal intensive care unit.
Most instruments designed to assess satisfaction in the NICU are in English, so new ones need to be developed or existing ones adapted and validated for the target language and culture.18–20 For this reason, we conducted a study to perform the transcultural adaptation and assess the psychometric properties of the resulting Spanish version of the EMPATHIC-N questionnaire, which may become an essential tool to assess the level of satisfaction of patients and their families, a key indicator of the quality of care in the NICU setting.16
Parents spent a mean of 12 min to complete the Spanish version of the EMPHATIC- N questionnaire, and the instrument appeared to be clear, comprehensible and easy to use. Our results were very similar to those of Orive et al., who reported a mean completion time of 10 min.21 This small difference in the completion time may have to do with the fact that the original questionnaire was submitted to parents by mail 2–3 weeks after discharge, whereas in our study parents were given the questionnaire during the stay of the infant in the NICU, before discharge. Similarly, in the validation studies of the Spanish version of the EMPATHIC questionnaire for the paediatric population21 and the Brazilian version12 and the Ethiopian version10 of the EMPHATIC-N, the questionnaires were administered at 24 and 48 h after admission, respectively. Completion in the unit could also have had an effect, as the professional that gave the paper questionnaire to the parent could answer any questions or doubts as they arose.10
Of the modifications proposed after the translation and transcultural adaptation to Spanish of the EMPATHIC-N,22 we only took into account those concerning the items present in the original version, as directed by its author9 and was done with the validation studies for other versions of the questionnaire.5,12,21 However, the Ethiopian validation study reduced the number of items to 38.10 As for the sample size, we analysed 65 completed questionnaires, so it was smaller compared to the samples used in the validation of the original instrument (282 questionnaires)9 the Italian version (162)5 or the recent validation study in Ethiopia (386).10 The validation study for the Brazilian version only included two successive groups of 8 and 5 mothers to assess the comprehensibility of the questionnaire.12 Thus, given the limited sample size in our study, the results need to be further validated in larger samples,9 as is also the case of the Brazilian version,12 using the validation study in Ethiopia as a model.10 As regards the characteristics of the sample, we collected data on the same variables regarding the participating parents and the hospitalised infants documented by Latour et al. for the original questionnaire.9 In the sample under study, the ethnic background of most parents was European, so there was little cultural diversity that could have affected how items were perceived. The studies for other versions have made different classifications of the sample, such as the study by Orive et al. for the Spanish paediatric population, which categorised participants as “Spanish” or “Other”,21 or the Ethiopian study, which divided the sample into “rural” and “urban”.10 The median length of stay of infants was similar to the one reported for the Spanish paediatric version21 and longer than the stays reported in the study of the original questionnaire9 and the Brazilian version12 (2, 7 and 9 days, respectively).
Of the 57 items in the questionnaire, 38 had scores of more than 5.5 out of 6 possible points. The item with the best mean score (5.85 points) concerned the encouragement to stay near the child (“Nos animaban a permanecer cerca de nuestro hijo/a”). The neonatal unit in our hospital has a 24 h a day open door policy for parental visits, so that parents can actively participate in the care of the infant at any time. Several studies have demonstrated that continuous parent-infant contact during the stay improves bonding and promotes interaction.23,24 Another of the items with the best scores in our Spanish sample was the one concerning the promptness of the response of the care team when the condition of the infant deteriorated (“Cuando el estado de salud de nuestro hijo/a empeoraba, médicos y enfermeras actuaban de forma inmediata”), with a mean score of 5.72, similar to what was observed in the Brazilian study.12 The multicentre study conducted in Ethiopia also assessed parental satisfaction based on the level of care of the NICU, and found better scores for all items in parents whose infants stayed in level II units; furthermore, the domain that was perceived most positively was organization, with scores nearing 6 points.10 Of the 57 items of the EMPATHIC-N questionnaire concerning neonatal intensive care services, only one was given scores below 5 points and concerned the level of noise in the unit (“El ruido en la unidad se mantenía tan bajo como fuera posible”), with a mean score of 4.78; this item also received the lowest scores in the study of the Spanish version of the paediatric questionnaire conducted by Orive et al.21 In the original study by Latour et al., there were 7 items with a mean score under 5 points.9 In preterm infants, continued exposure to high noise levels causes short-term physiological changes (increased blood pressure, apnoeic episodes and sleep disturbances) and long-term neurobehavioural and developmental changes.25 Orive et al. attributed this result to the health care staff speaking loudly and the low ceilings of the unit, which amplified sound.21 Our own findings suggest that the architectural changes made to the neonatal unit (individual rooms, adequate ceiling height…) did not suffice to guarantee a quiet environment. The loudest noises result from the movement of health care staff, especially in shift changes and during patient admissions, so the installation of noise metres to record sound levels could be a useful intervention to try to reduce the noise level.26
We found several similarities in the results of the statistical analysis between our study and the Brazilian version validation study.12 In both, there was a high proportion of “not applicable” answers for the item concerning the informational brochure provided to parents (“El folleto de información que recibimos era claro y completo”) and the consideration of the family’s cultural background (“Nuestro origen cultural se tuvo en cuenta”). The high proportion of “not applicable” answers in both studies can be explained by the low availability of this material in the unit. Although in the Brazilian study the possibility of removing this item was contemplated,12 the decision was made to keep it after the second round to maintain the total number of items present in the original version, as this is a method used in many countries to introduce the NICU to the parents, providing important information about their future stay in the unit. Thus, what is needed is the provision of this type of material in every neonatal unit. The high proportion of “not applicable” answers in the Brazilian12 and our own study in Spain of the item concerning the consideration of the family’s cultural background could be explained by a limited comprehension of the item by participants, as the populations under study had little cultural diversity. As was done in the Brazilian version,12 these 2 items were maintained in the Spanish version, thus keeping the 57 items of the original version of Latour et al.9 to facilitate its future application in culturally diverse populations. In the Ethiopian version, the item concerning the provision of a printed brochure with clear and thorough information was eliminated, in addition to another 18 items of the original questionnaire, due to the lack of those resources in the hospitals.10
To assess reliability, as Latour et al. did for the original questionnaire,9 we calculated the internal consistency of each domain as if it were a stand-alone questionnaire. In agreement with the studies conducted for the Italian version,5 the Spanish version for the paediatric intensive care setting21 and the Amharic version in Ethiopia,10 the highest reliability (0.95) corresponded to the care and treatment domain (in the Spanish sample, in addition to the information domain) and the lowest reliability to the organization and parental participation domains. The coefficient for the professional attitude domain was 0.87. Overall, in our sample, we found a high internal consistency with coefficients similar to those obtained for the Dutch (0.82−0.95),9 Italian (0.72−0.92),5 Ethiopian (0.74−0.95)10 and Brazilian (0.70–1)12 versions.
We assessed the convergent validity of the questionnaire by analysing the correlation between the scores in the four general satisfaction items and the 5 domains of the questionnaire, obtaining similar results to those reported for the original version9 and inferior to those reported for the Italian version.5 The lowest correlation corresponded to the parental participation domain, with a coefficient of 0.37, in agreement with the correlation found for the original version.9 In the validation study in the paediatric population conducted by Orive et al.,21 the lowest correlation corresponded to the information given to parents, with a coefficient of 0.41. Other validation studies did not carry out this analysis, but the Ethiopian study also analysed the association between parental answers regarding their overall experience and impressions and the domains of the EMPHATIC-N, in addition to a quantitative analysis of these answers.10
When it comes to the limitations of the study, we ought to highlight that it was carried out in a particular neonatal unit in Spain, which is not representative of all such units in Spain. It would be interesting to obtain a larger sample of questionnaire responses from different neonatal units in Spain, as was done in the validation studies of the Italian5 or Ethiopian10 versions of the EMPATHIC-N. Furthermore, since there are no other validated instruments in Spanish, we were unable to complete the convergent validity analysis of the EMPATHIC-N questionnaire comparing it with other instruments, and could not assess the test-retest reliability of the questionnaire, as we ruled out the possibility of repeating the assessment on account of the characteristics of the sample and the unit, as recommended by other authors,27 even by analysing two cohorts at different time points.9
Clinical implications and future lines of researchThe validation study of the Spanish version of the EMPATHIC-N questionnaire, as was the case with the English,9 Italian,5 Brazilian Portuguese12 and Ethiopian10 versions, was conducted in parents of infants admitted to neonatal intensive care units, so this instrument is mainly applicable in this care setting. The use of questionnaires to assess parental satisfaction in neonatal care units can help identify interventions that can improve care quality and contribute to humanize care delivery. The validation of the Spanish version of the EMPATHIC-N and its future dissemination and application in neonatal units in Spain will facilitate the development of future studies in larger and multicultural samples.13,16 The performance of multicentre studies, like those conducted in Italy5 or Ethiopia,10 with a quantitative and qualitative analysis of parental responses to open-ended questions10 could yield essential information for improving the quality of FCDC, in addition to detailed insight into the factors that contribute to satisfaction in families.
ConclusionThe Spanish version of the EMPATHIC-N questionnaire is a comprehensible, useful, valid and reliable instrument to measure satisfaction in the parents of children admitted to the NICU. Multicentre studies in larger samples are needed to corroborate these results and to improve the quality of family-centred developmental care.
FundingThis research did not receive any external funding.
Conflicts of interestThe authors have no conflicts of interest to declare.
We thank the parents of the patients for completing the questionnaires, the staff of the units and the colleagues that participated in the expert panel.