Poisonings are not an infrequent reason for pediatric emergency department visits, as they account for 0.2% to 0.3% of care episodes in this setting.1 To manage these cases, health care professionals in Spain have specific resources at their disposal, such as the Servicio de Información Toxicológica (SIT, Toxicology Information Service), affiliated to the Instituto Nacional de Toxicología y Ciencias Forenses (National Institute of Toxicology and Forensic Sciences), which can be reached for consultation 24 h a day.2 There are additional resources for reference, such as the TOXBASE online database of the United Kingdom3 and the poisoning handbook (PHB) (Manual de intoxicaciones) of the Sociedad Española de Urgencias de Pediatría (SEUP, Spanish Society of Pediatric Emergency Medicine).1 The aim of our study was to assess the adherence of current clinical practice to the recommendations provided by the SIT, TOXBASE and PHB in terms of observation, hospital admission and diagnostic tests.
We conducted a cross-sectional, observational and descriptive study in a secondary hospital analyzing the cases of exposure to potentially toxic substances in patients aged 0–14 years managed in the emergency department between January 2016 and December 2022. We retrieved the data through the Orion Clinic software, including information on demographic and clinical variables, the involved substance, diagnostic tests, treatments and discharge destination. We only included cases in which providers consulted with the SIT to guide the management of the case. The recommendations given by the SIT were compared with those provided by the TOXBASE and PHB to assess the agreement between these resources.
We assessed agreement by means of the Cohen κ, and established a level of significance of 0.05. The statistical analysis was performed with the R software.
Of the 99 023 pediatric emergency visits that took place during the study period, 0.49% (487 care episodes) corresponded to exposure to potentially toxic substances. Of this subset, 43.7% (213 care episodes) met the inclusion criteria, and we retrieved 321 recommendations provided by the SIT. The frequency of exposure to potentially toxic substances was highest in boys aged less than 6 years, and medications were the most frequently involved type of substance (53.5%).
The recommendations of the SIT, in order of decreasing frequency, were: treatment (38.3%; n = 123), observation/admission (34.3%; n = 110) and testing (14.3%; n = 46).
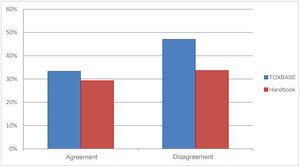
When we compared these recommendations to the TOXBASE recommendations, we found that 46.4% (n = 149) of the recommendations given by the SIT disagreed with the management recommended by this database. Similarly, in the comparison with the PHB, 33% (n = 106) of recommendations provided by the SIT diverged from those provided in the handbook (Fig. 1).
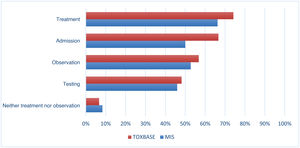
After classifying the SIT recommendations into categories, we found significant differences upon comparison with the other two resources (P < .001). In the comparison with the TOXBASE recommendations, the highest proportion of disagreement corresponded to the treatment (74.19%; n = 69), admission (66.67%; n = 12) and observation (56.76%; n = 42) categories. Similarly, in the comparison with the PHB, the proportion of disagreement was highest for the treatment (66.25%; n = 53), admission (50%; n = 6) and observation (52.73%; n = 29) categories (Fig. 2).
The concordance analysis showed a weak correlation between the SIT and TOXBASE recommendations (κ = 0.323) and the SIT and PHB recommendations (κ = 0.365). However, the agreement between the TOXBASE and PHB recommendations was considerably greater (κ = 0.691, which indicates substantial agreement).
Our study showed that there are significant discrepancies in the management approach recommended by the SIT compared to the TOXBASE and PHB recommendations. Specifically, the SIT tends to promote more conservative management with more frequent recommendation of therapeutic interventions. These differences could be due to the characteristics of the phone consultations with the SIP, in which the available information may be limited.3 In contrast, the TOXBASE and PHB are resources used directly by health care providers, who have access to the patient and can implement appropriate recommendations in real time.
Despite the observed discrepancies, we believe that the SIT is a key resource in the management of pediatric poisonings, as it offers initial guidance that may be essential in reducing morbidity and mortality. However, studies on this subject underscore the importance of a closer and ongoing collaboration of all guidance system/resources at play in the management of pediatric poisoning.4–6 The development of evidence-based protocols and ongoing updating of clinical practice guidelines can help standardize management and reduce the unnecessary use of resources.
There are discrepancies between the recommendations provided by the SIT and those provided in the TOXBASE and the PHB, particularly as regards the indication of treatment, observation/admission and testing. These discrepancies highlight the need to promote the ongoing and collaborative updating of pediatric poisoning resources with the ultimate goal of ensuring a standardized and efficient approach to the management of poisoning in the pediatric population.
Previous meeting: this study was presented as an oral communication at the 25th Meeting of the Sociedad Española de Urgencias Pediátricas (SEUP); June 2022; Pamplona, Spain.