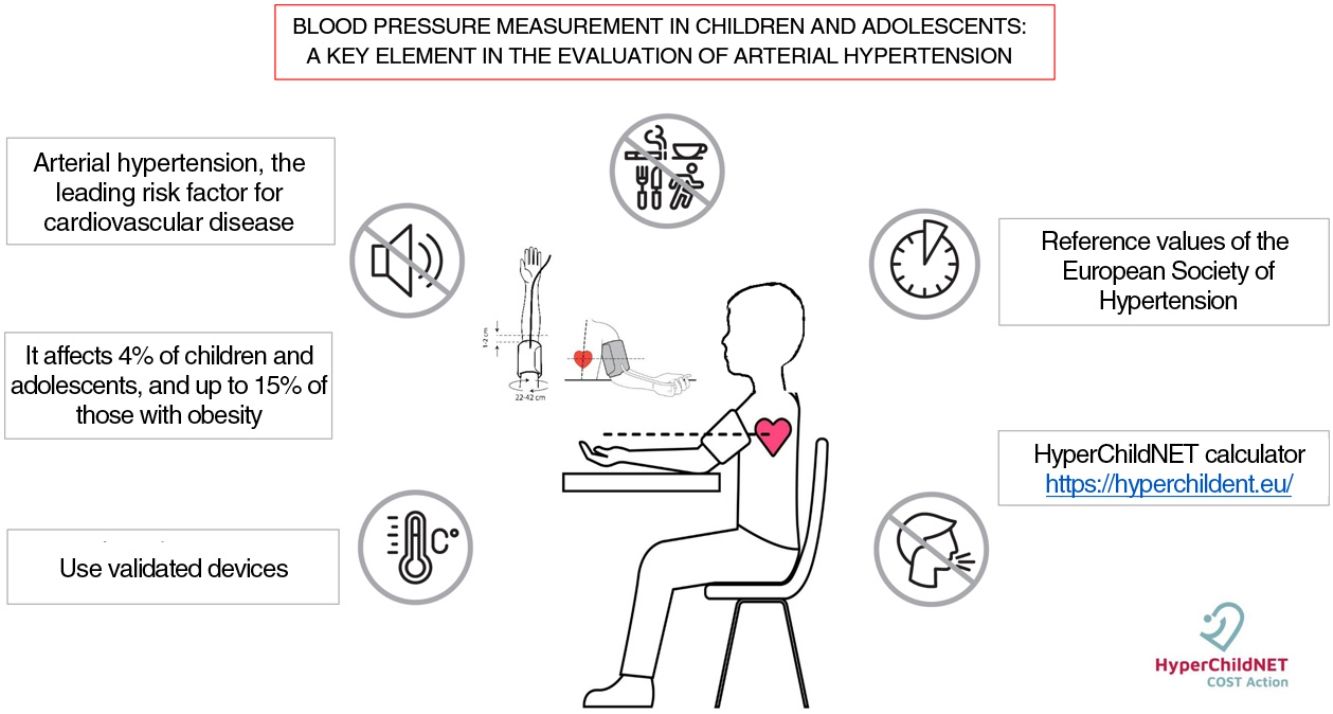
Arterial hypertension is the main modifiable risk factor for cardiovascular disease, occupying the first place among the causes of loss of life years adjusted for disability. In recent years, arterial hypertension in children and adolescents has gained ground in cardiovascular medicine thanks to progress made in several areas, fundamentally in pathophysiological and clinical research. Despite the advances that have been made in recent years, the prevention, diagnosis and treatment of high blood pressure in children and adolescents still have room for improvement. In this sense, the correct measurement of blood pressure is especially important, since it includes a series of essential elements such as the measurement devices, the regulated procedure and the interpretation of the results based on percentiles according to age, gender and height. The availability of a free access calculator facilitates the diagnosis and monitoring of arterial hypertension https://hyperchildnet.eu/.
La hipertensión arterial es el principal factor de riesgo modificable para la enfermedad cardiovascular ocupando el primer lugar entre las causas de pérdida de años de vida ajustados por discapacidad. En los últimos años la hipertensión arterial en niños y adolescentes ha ganado terreno en la medicina cardiovascular gracias a los avances en diversas áreas de la investigación fundamentalmente fisiopatológica y clínica. A pesar de los avances que se han llevado a cabo en los últimos años, la prevención, diagnóstico y tratamiento de la hipertensión arterial en niños y adolescentes todavía son susceptibles de mejorar. En este sentido cobra especial relevancia la medida correcta de la presión arterial que contempla una serie de elementos indispensables como son los dispositivos de medición, el procedimiento reglado y la interpretación de los resultados en base a percentiles según edad, sexo y talla. La disponibilidad de una calculadora de acceso libre facilita el diagnóstico y seguimiento de la hipertensión arterial https://hyperchildnet.eu/.
Arterial hypertension (HTN) is the main modifiable risk factor for cardiovascular disease, which is the leading cause of loss of disability-adjusted life-years.1 In recent years, HTN in children and adolescents has gained ground in the field of cardiovascular medicine due to advances in several areas of research, chiefly pathophysiological and clinical. The recommendation of HTN guidelines for children and adolescents of measuring arterial blood pressure (BP) from age 3 years2–4 and longitudinal studies have evinced that mild elevation of BP early in life is much more common than previously believed and that HTN in adults has its roots in adolescence and childhood.5–7 Before age 3 years, BP should be measured in the presence of factors that increase the risk of HTN, such as preterm birth, low birth weight, neonatal disease requiring intensive care, congenital heart disease, renal disease, treatment with drugs that raise BP, oncological or haematological disease, solid organ or bone marrow transplantation or increased intracranial pressure.2
Although numerous studies have assessed the prevalence of HTN in children and adolescents, it is difficult to determine due to mainly 3 reasons: (i) There are physiological changes in BP associated with growth and development, which means that there are no fixed thresholds to define elevation of systolic or diastolic BP. This complication has led to the application of percentiles for age, sex and height, defining HTN as a BP value at the 95th percentile (P95) or higher. (ii) Variation in the definition of HTN used by the 3 most recent clinical guidelines, published in Europe,2 United States3 and Canada.4 (iii) Considering the variability of BP from beat to beat, it was necessary to require that the systolic and/or diastolic BP be persistently above established thresholds on 3 separate occasions for diagnosis of HTN. As a result, many cross-sectional studies with a single measurement of BP could not determine the prevalence of HTN.
A recently published meta-analysis that included data for 185 000 children and adolescents aged 19 years or younger found an overall prevalence of HTN of 4%.8 This prevalence varies within the paediatric age group, with HTN detected in 4.3% of children at age 6 years and 7.9% at 14 years, subsequently dropping to 3.3% at 19 years. In agreement with other studies, the prevalence of HTN was higher in the presence of obesity (15%), compared to overweight (5%) and normal weight (1.9%). The review also noted a 75% increase in the prevalence of HTN from 2000 to 2015, which can be explained in part by the increase in obesity in the paediatric population.
At present, it is well known that in children and adolescents, the prevalence of secondary HTN is of 1%, and that primary HTN is the most frequent type of HTN in this age group, especially in adolescents.9 Primary HTN is usually asymptomatic or, in some cases, may cause mild symptoms such as headache, epistaxis or changes in behaviour and academic performance, and therefore the association between HTN and these symptoms may often be overlooked, which is why it is important to start measuring BP at age 3 years, as recommended by every guideline.2–4 Detecting abnormal BP values in the early stages of life can allow implementation of corrective measures to reduce the burden of cardiovascular disease.
Despite the advances made in recent years, the diagnosis and treatment of HTN can still be improved. Correct measurement of BP is particularly important in this regard.
Methodology for blood pressure measurementBlood pressure measurement is considered one of the most important assessments in clinical practice, but, as Professor Thomas G. Pickering already wrote in 2005, “Blood pressure determination continues to be one of the most important measurements in all of clinical medicine and is still one of the most inaccurately performed.”10 There are a series of indispensable elements that need to be taken into account for the correct measurement of BP.
Devices for BP measurementThe European Society of Hypertension (ESH) guidelines for the management of high blood pressure in children and adolescents), the American Academy of Pediatrics (AAP) for management of high BP and, recently, the Hypertension Canada guidelines, dictate that the auscultatory technique is the method of choice for diagnosis of HTN.2–4 However, due to restrictions to the use of mercury sphygmomanometers and advances in oscillometric devices, the oscillometric methods is currently most widely used for measurement of BP.
To establish the correct methodology for the use of these devices, in 2021 the ESH published practice guidelines for office and out-of-office blood pressure measurement.11 This guideline contemplates the use of automated BP measuring devices for clinical practice as long as the monitors used have been validated in children and adolescents. There are websites that provide updated lists on the devices that are appropriate for each population. With these concerns in mind, the ESH and the International Society of Hypertension have developed the initiative known as STRIDE BP (www.stridebp.org). A list of devices validated in the paediatric population is also available at www.dableducational.org. Devices that take triplicate readings automatically are preferred. It is worth noting that none of the automated devices for measurement of BP at the wrist have been validated in this age group.
If none of the validated devices are available, it is possible to use a manual (hybrid) electronic auscultatory device with an LCD or LED mercury column-like display or an aneroid sphygmomanometer. The latter require calibration at least once a year. Once the cuff is inflated, it must be deflated at a rate of 2–3 mm Hg/s, using Korotkoff sound 1 for determination of systolic BP (SBP) and Korotkoff sound 5 for the diastolic blood pressure (DBP). For the latter, Korotkoff sound 4 should be used if sounds are still present at full cuff deflation or below the 40 mm Hg point.
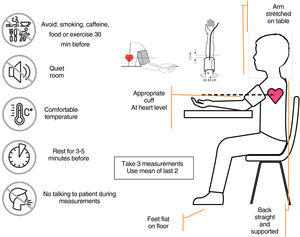
Blood pressure measurement procedureBased on the recommendations of the ESH,10 the following steps are required to correctly obtain BP measurements:
Verify that the child/adolescent has not consumed any stimulant substances (cocoa/cola), smoked or exercised in the 30 min prior to the measurement of BP.
Select the appropriate cuff based on the mid-upper arm circumference, measured at the midpoint between the elbow and shoulder.
Place the cuff on the arm above the antecubital fossa and sit the patient on a chair in a quiet environment at a pleasant temperature, with minimum interaction with staff, with the back straight and supported, the feet flat on the floor and the arm resting on a table
After 3−5 min of rest, make an initial BP measurement and then make 2 more measurements, with 1-minute intervals between readings. The ambulatory BP value will be calculated as the mean of the last 2 measurements.
Arm selectionIn the first visit, the BP should be measured in both arms. A difference greater than 10 mmHg should be confirmed with repeated measurements. If the difference is confirmed, the measurements of BP will be made in the arm with the highest values. In the case of a difference in BP greater than 20 mmHg, a more thorough investigation is required to rule out vascular stenosis.
Cuff selectionWith the patient in the seated position, measure the mid-arm circumference (between shoulder and elbow). Record the circumference and choose the appropriate cuff (one in which the range printed on the cuff itself includes the measured circumference). The most common cuff sizes in the paediatric age group are: 17–22, 22−32 and 32−42 cm. Correct selection of the cuff is crucial, as a smaller-than-needed cuff will overestimate BP values, and vice versa. Only the cuffs provided by the manufacturer for any given monitor model should be used for BP measurement.
The cuff must be placed with the artery mark positioned in the anterior surface of the arm (2−3 cm above the antecubital fossa) with the arm resting on the table and its midpoint at the level of the heart (Fig. 1). The cuff should be equally tight at the top and bottom edges, and it should be possible to fit a finger under the cuff at both edges.
Blood pressure measurement procedure (modified from a poster published by the European Society of Hypertension11). (Images used after obtaining license from Shutterstock).
In patients with severe obesity (arm circumference >42 cm), consider using special conical cuffs, as rectangular cuffs may overestimate BP values. If these cuffs are not available, a validated electronic wrist-cuff device may be used.
Table 1 summarises the most common errors that may be made in measuring BP in children and adolescents.
Main sources of error in blood pressure measurement in children and adolescents.
| Source of error | Problem |
|---|---|
| Patient | Nervous or crying (infant)Recent consumption of stimulant substances (cocoa, cola…)Not long enough resting period before BP measurement |
| Equipment | Use of device that has NOT been validatedUse of device that has NOT been calibratedWrong cuff sizeCuff not recommended by device manufacturerCuff or tubing in poor condition |
| Technique | Inadequate positioning of patientIncorrect cuff placement (position/tightness)Incorrect placement of stethoscope (for auscultation)Taking fewer than 3 BP measurements |
Contrary to the adult population, as previously noted, the definition of HTN in children and adolescents in based on the normal distribution of BP in healthy children and not in the cardiovascular morbidity and mortality associated to specific BP values.
In 2016, the ESH published its most recent recommendations,2 maintaining the values published in the Fourth Report as reference for the population up to 16 years of age.12 A year later, the AAP modified the reference values of the Fourth Report,12 excluding participants with overweight or obesity.3 The discrepancy between published reference values is a subject that has attracted considerable interest and sparked debate. A study conducted by Lurbe et al.13 that compared how paediatric patients in different age groups would be classified based on the application of different reference values found that the use of the APP criteria13 led to classification of a greater proportion of children as having HTN or high-normal BP compared to the ESH criteria.2 To assess the impact that these two standards have in clinical practice, studies have analysed the presence of manifestations characteristic of HTN, such as an increased left ventricular mass index,2,3 in children classified according to the criteria established in these 2 guidelines. One such study14 and a recently published meta-analysis15 concluded that the use of the AAP criteria compared to the ESH criteria resulted in the identification of HTN in a higher proportion of patients, but that this did not result in a more accurate prediction of left ventricular hypertrophy.14,15 In consequence, the ESH has maintained the classification criteria established in the 2016 guidelines.2
To facilitate the detection of high BP values in children and adolescents, we attach a simplified version of the reference value tables (Table 2). This table presents the values of the 90th percentile for age for the 5th percentile for height. If the systolic and/or diastolic BP value of the child under study is below the values for sex and age presented in this table, the child is normotensive and does not require further assessment other than the BP measurements performed as part of the routine care of healthy children. If the BP values are higher, the reference values published by the ESH should be applied, in addition to following the recommendations for management provided in the guidelines of this society.2 Recently, thanks to the work of the COST Action HyperChildNET, funded by the European Union (reference CA 19115),16 the first online calculator has been made available that applies the reference values proposed by the ESH for children and adolescents.2 This tool can be accessed for free at https://hyperchildnet.eu/.
Table for screening of high BP values based on the European Society of Hypertension guidelines for the management of high blood pressure in children and adolescents2.
| Age (years) | Blood pressure (mm Hg) | |||
|---|---|---|---|---|
| Male | Female | |||
| SBP | DBP | SBP | DBP | |
| 1 | 94 | 49 | 97 | 52 |
| 2 | 97 | 54 | 98 | 57 |
| 3 | 100 | 59 | 100 | 61 |
| 4 | 102 | 62 | 101 | 64 |
| 5 | 104 | 65 | 103 | 66 |
| 6 | 105 | 68 | 104 | 68 |
| 7 | 106 | 70 | 106 | 69 |
| 8 | 107 | 71 | 108 | 71 |
| 9 | 109 | 72 | 110 | 72 |
| 10 | 111 | 73 | 112 | 73 |
| 11 | 113 | 74 | 114 | 74 |
| 12 | 115 | 74 | 116 | 75 |
| 13 | 117 | 75 | 117 | 76 |
| 14 | 120 | 75 | 119 | 77 |
| 15 | 122 | 75 | 120 | 78 |
| ≥16 | 135 | 85 | 135 | 85 |
DBP, diastolic blood pressure; SBP, systolic blood pressure.
The diagnosis of HTN is based on BP percentile distributions for age, sex and height up to age 16 years.
From this age, the definition of HTN is based on the criteria established by the guidelines developed collaboratively by the European Society of Cardiology and the ESH, or 140/90 mm Hg.17Table 3 presents the percentiles used to establish the diagnosis in children aged less than 16 years and the BP thresholds used in adolescents aged 16 years or older.
Definition and classification of hypertension in children and adolescents.2
| SBP and/or DBP | ||
|---|---|---|
| <16 years | ≥16 years and adults | |
| Normal | <130/85 | |
| Normal-high | ≥P90 y < P95 | 130−139/85−89 |
| Hypertension | ||
| Stage 1 | ≥P95 to P99 and 5 mm Hg | 140−159/90−99 |
| Stage 2 | >P99 plus 5 mm Hg | 160−179/100−109 |
| Isolated systolic HTN | SBP ≥ P95 and DBP < P90 | SBP ≥ 140 and DBP < 90 |
DBP, diastolic blood pressure; HTN, hypertension; P90, 90th percentile; P95, 95th percentile; P99, 99th percentile; SBP, systolic blood pressure.
Adapted from the European Society of Hypertension guidelines for the management of high blood pressure in children and adolescents.2
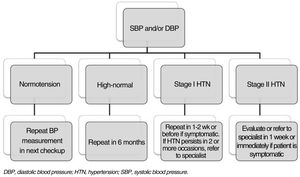
Blood pressure values in children and adolescents may vary from visit to visit. Thus, there is evidence that the prevalence of elevated BP values (above the P95) decreases by 53% in the second visit and by up to 77.7% in the third visit compared to the first visit when BP is measured.12 Therefore, HTN should never be diagnosed based on values obtained in a single visit, unless office BP values are compatible with symptomatic HTN, stage 2 HTN in patients under 16 years, or above 180/110 mm Hg in patients aged 16 years or older. To confirm the diagnosis of HTN based on office BP, at least 2 or 3 additional office assessments of BP must be made in a 1- to 4-week period (depending on BP values and the risk of underlying disease).
All guidelines2–4 recommend confirmation of the HTN diagnosis with 24 -h ambulatory or home BP monitoring to rule out white-coat HTN.
Fig. 2 presents the hypertension diagnosis algorithm proposed by the ESH2 for follow-up of patients after office BP measurement.
Hypertension diagnosis algorithm based on the European Society of Hypertension guidelines.2
Neonatal hypertension is uncommon, but has been detected with increasing frequency. Blood pressure should be measured in the right arm, and oscillometric BP measurement with a device validated in newborns is the most widely used method. The length of the cuff bladder should span 80%–100% of the arm circumference. The published data are limited as regards reference values, and the risks, treatment and long-term results. There are no clinical practice guidelines and the management is based on clinical judgment and expert opinion. The available reference values are those published by et al. in 2012, which include BP values in infants from 26 to 44 weeks of postconceptional age.18
In the case of infants, current recommendations contemplate measurement in the right arm, a cuff with a bladder width of approximately 50% of the mid-arm circumference, using a validated oscillometric device and with performance of 3 measurements 2 min apart.19 The reference values applied to infants aged 1 month to 1 year continue to be those published in 1987.20
In both cases, the approach to diagnosis is similar to the one employed in older children.
Beyond office blood pressureAt present, there are methods available to obtain BP readings outside the office. They include:
- a)
24-h ambulatory blood pressure monitoring (ABPM). Ambulatory BP monitors are portable devices that allow collection of more than 80 BP readings outside the office while the child or adolescent is engaged in usual everyday life. The values obtained by ABPM have proven to be more reproducible and more strongly correlated with target-organ damage compared to office BP values.2 Four different BP phenotypes have been established based on the combination of office BP and ABMP values. When there is agreement between both, BP values may be normal with both methods, which is known as normotension, or high, which is known as sustained HTN. If there is disagreement between office and ambulatory values, the possible phenotypes are white-coat HTN (high office BP values and normal ambulatory BP values) or masked HTN (normal office values and high ambulatory values). In consequence, the ESH recommends performance of ABPM in every patient with a diagnosis of HTN based on office BP measurement, especially if prescription of antihypertensive medication is contemplated, in order to prevent initiation of antihypertensive treatment in patients with white-coat HTN.2 This technique must be carried out in centres experienced in the diagnosis and treatment of HTN. The reference values for ABPM and the indications for its use are detailed in the ESH guideline.2
- b)
Home BP monitoring. This approach has also proven useful, as there is evidence of superior reproducibility and a higher correlation with target organ damage in home BP monitoring values compared to office BP values.2–4 It requires minimal training of the family, explaining the importance of making 3 consecutive BP measurements, in the morning as well as in the evening, at least 3 or 4 days in one week (although 7 consecutive days is preferable), always prior to taking any antihypertensive drugs (if applicable). The readings should be made following the procedure recommended above (Fig. 2) and with monitors validated in children and adolescents. The values must be recorded in a form to be evaluated at a later time by the paediatrician in charge. To interpret values, the mean of all readings is calculated, excluding values recorded the first day, followed by calculation of the corresponding percentile based on the reference values published in the ESH guideline.2 Home BP monitoring is indicated for follow-up of patients with a diagnosis of HTN, whether or not they are receiving antihypertensive medication.
- c)
Other BP measurement approaches. New devices for estimation of BP values based on emerging technologies are entering the market. These include cuffless BP measuring devices, based on (among other variables) the calculation of the pulse wave velocity. These devices, shaped as a wristwatch or wristband, could be useful, as they allow continuous monitoring of BP values. However, none of them have been properly validated in the paediatric population, so their use is not currently recommended.
In order to facilitate the interpretation of measured BP values for diagnosis and follow-up of children and adolescents, HyperChildNET has developed a free-access calculator that allows quick assessment of office BP values. Its use facilitates the diagnosis and follow-up of HTN (https://hyperchildnet.eu/).
FundingThis publication is based on the work of the COST Action HyperChildNET (CA19115), with the support of COST (European Cooperation in Science and Technology) and the Horizon 2020 Framework Programof the European Union.
Please cite this article as: Álvarez J, Aguilar F and Lurbe E, La medida de la presión arterial en niños y adolescentes: elemento clave en la evaluación de la hipertensión arterial, Anales de Pediatría. 2022;96:536.