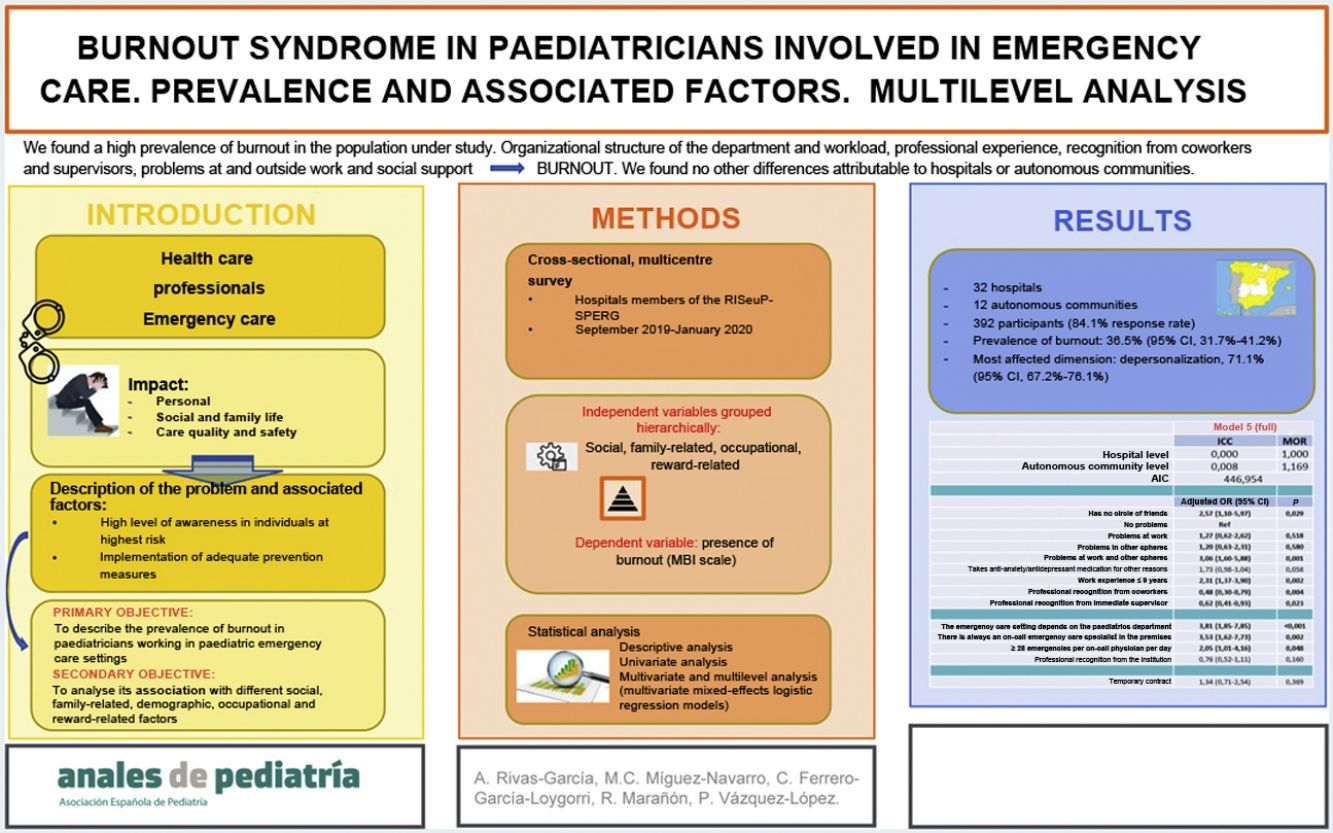
The aim of our study was to describe the prevalence of burnout syndrome (BOS) in paediatricians working in paediatric emergency care settings and to analyse its association with potential risk factors.
Material and MethodsMulticentre cross-sectional study through a survey of paediatricians working in paediatric emergency care settings in hospitals affiliated to the Research Network of the Spanish Society of Paediatric Emergency Medicine (SEUP) between September 2019 and January 2020. We analysed the association between social/family-related, demographic, occupational and satisfaction factors and the presence of BOS by means of multivariate and multilevel mixed-effects logistic regression models.
ResultsThe estimated prevalence of BOS was 36.5% (95% confidence interval [CI], 31.7 %–41.2%). In the multivariate analysis, lacking a stable group of friends (OR, 2.57; 95% CI, 1.10−5.97), problems in and out of the work setting (OR, 3.06; 95% CI, 1.60−5.88) and a work experience of 9 years or less (OR, 2.31; 95% CI, 1.37−3.90) were identified as individual factors that increased the risk of SBO, while feeling acknowledged by coworkers (OR, 0.48; 95% CI, 0.30−0.79) and acknowledged by one’s supervisor (OR, 0.62; 95% CI, 0.41−0.93) were protective factors. In relation to the hospital, the paediatric emergency unit being a subdepartment of the Department of Paediatrics (OR, 3.81; 95% CI, 1.85−7.85), the presence of an on-call emergency medicine specialist around the clock (OR, 3.53; 95% CI,1.62−7.73) and a volume of 28 or more paediatric emergency encounters a day to be managed per on-call physician (OR, 2.05; 95% CI, 1.01−4.16) were identified as independent risk factors for SBO. There was no variability in the prevalence of BOS attributable to differences between hospitals and autonomous communities, save for the described situations.
ConclusionsThe prevalence of SBO among these providers is high. There are modifiable factors that we can intervene on to address BOS, independently of the hospital or region.
El objetivo del estudio es describir la prevalencia de Síndrome de Burnout (SBO) entre pediatras con actividad en Urgencias Pediátricas (UP) y analizar su asociación con potenciales factores de riesgo.
Material y métodosEstudio de encuestas transversales multicéntrico, entre pediatras con actividad asistencial en UP, en Hospitales miembros de la Red de Investigación de la Sociedad Española de UP (RiSEUP-SPERG), entre septiembre 2019 y enero 2020. Se analizó la relación de factores sociofamiliares, demográficos, laborales y de satisfacción con la presencia de SBO mediante modelos mixtos de regresión logística multivariable y multinivel.
ResultadosLa prevalencia estimada fue 36,5% (IC95%:31,7–41,2%). Tras el análisis multivariable, no disponer de un círculo de amigos estable (OR:2,57; IC95%:1,10−5,97), tener problemas en el ámbito laboral y extralaboral (OR:3,06; IC95%:1,60−5,88) y llevar trabajando 9 años o menos (OR:2,31; IC95%:1,37−3,90) se presentaron como factores individuales que aumentaron el riesgo de SBO; sentirse reconocido por compañeros (OR:0,48; IC95%:0,30−0,79) y supervisor (OR:0,62;IC95%:0,41−0,93) parecieron actuar como protectores. En el ámbito hospitalario, que la Urgencia dependiera del Servicio de Pediatría (OR:3,81; IC95%:1,85−7,85), siempre hubiera un especialista en Urgencias de guardia (OR:3,53; IC95%:1,62−7,73) y que cada médico de guardia atendiera 28 episodios de urgencias/día o más (OR:2,05; IC95%:1,01–4,16), constituyeron factores de riesgo independiente para el SBO. No existió variabilidad en la presencia de SBO atribuible a la diferencia entre Hospitales y Comunidades Autónomas (CC.AA), al margen de las situaciones descritas.
ConclusionesLa prevalencia de SBO en estos profesionales es elevada. Existen factores sobre los que podemos incidir para modificar el SBO, independientemente del Hospital o CC.AA.
Burnout syndrome (BOS) can be interpreted as the extreme response of the chronic stress experienced in the workplace. The World Health Organization has recognised it as an occupational disease that has deleterious effects on physical and mental health and that can manifest with emotional, behavioural and psychosomatic symptoms.1
Historically, BOS has been associated with professions that involve close interaction with other people, especially those with a significant emotional burden. Therefore, health care professionals are a collective that is particularly vulnerable to this syndrome.2–4 Emergency care settings are stressful environments due to the heavy workloads, high patient expectations, long hours, lack of rest and significant responsibility for patients with severe disease.5 In addition, in the case of paediatrics, professionals do not only engage in the comprehensive care of the child, but also of the family, so the emotional burden may be even greater.6
There is no specific cause for the development of BOS, and it has been associated with psychological or psychiatric, sociodemographic, organizational and social factors.7,8
Characterising BOS in paediatric emergency care providers is of utmost importance, as its consequences can be devastating for them and their surroundings,8,9 and it has an impact on the quality of care, undermines the doctor-patient relationship and increases the risk of errors.9 Describing the problem and the associated factors makes it possible for individuals at risk to maintain a high level of awareness and to establish adequate prevention measures.
The primary objective of our study was to describe the prevalence of BOS in paediatricians involved in the delivery of paediatric emergency care (PEC).
The secondary objective was to analyse the association of BOS with different social, family-related, demographic and occupational factors and rewards.
MethodsWe conducted a multicentre, cross-sectional survey of paediatricians working in paediatric emergency care settings in hospitals members of the Research Network of the Sociedad Española de Urgencias de Pediatría (Spanish Society of Paediatric Emergency Medicine) (RiSeuP-SPERG) between September 2019 and January 2020.
SampleWe included all paediatricians who worked in PEC settings in any of the recruited hospitals who completed the questionnaire and consented to participate.
We defined paediatrician involved in PEC delivery as a doctor specialised in paediatrics employed in a hospital and working full time or part time in a PEC setting.
We defined PEC specialist as a doctor specialised in paediatrics that had worked exclusively in PEC for a minimum of 2 years.
ProtocolThe data collection period took place once the hospitals had been recruited, which was accomplished through the dissemination of the study protocol via the mailing list of the RISeuP-SPERG. Each participating hospital had a collaborating researcher appointed to distribute the survey (Appendix B1) to physicians involved in PEC delivery in that hospital, responsible for filling out a form with general information on the shared background of the participants from that centre (Appendix B2). Responses were accepted for a period of 16 weeks, and the principal investigator performed database quality reviews periodically to eliminate duplicate responses and identify inconsistencies or abnormal values.
Study variablesIndependent variablesWe collected data on social, family-related, demographic and occupational factors and rewards (Appendix B1-Part I and Appendix B2). We grouped these data hierarchically into 3 levels: baseline/individual, hospital and autonomous community (Appendix B3).
Given the complexity and heterogeneity of shift schedules, we defined on-call shift as an overnight shift in the emergency department with a minimum duration of 12 h.
We considered a paediatric emergency department independent if it was not a care setting administered as a dependent subdivision of another department, such as paediatrics or the general emergency department.
Dependent variablePresence of BOS, defined for the purpose of this study as intermediate to high levels of emotional exhaustion and depersonalization associated with low or intermediate levels of personal accomplishment in the Maslach Burnout Inventory (MBI).4
Measurement of the dependent variableWe used the validated Spanish translation of the MBI for medical personnel2 (Appendix B1-Part II). The MBI, the most widely used scale worldwide, has a high internal consistency and a reliability near 90%.10
It comprises 22 statements, each of which is rated on a scale from 0 to 6 based on the frequency with which it is experienced. The statements are distributed into 3 subscales: emotional exhaustion, depersonalization and personal accomplishment. High scores in the first two and a low score in the third one define BOS, with the level of burnout established based on the distribution shown in Table 1.11
Statistical analysisAfter performing a descriptive analysis of the independent variables, we estimated the prevalence of BOS as a percentage with the corresponding 95% confidence interval (CI).
To explore the factors associated with BOS, we started by performing a univariate analysis by means of the χ2/Fisher exact test for qualitative variables and the Student t test/analysis of variance (ANOVA) or the Mann-Whitney U/Kruskal–Wallis test for quantitative variables, depending on the number of categories and the shape of the distribution. We assessed the strength of the association using binary logistic regression, calculating odds ratios (ORs) with the corresponding 95% CIs. For qualitative variables with more than 2 categories, we assessed the risk relative to a reference category. We categorised quantitative variables with the purpose of facilitating interpretation, defining intervals based on the existing evidence, clinical experience or the graphical analysis of the data for the variable.
Later on, we conducted a multivariate multilevel analysis, establishing 3 hierarchical levels (individual, hospital and autonomous community).
We fitted different mixed effects logistic regression models, including covariates that have been found to be statistically significant or nearly significant in the univariate analysis. The models analysed the random effects and variance attributed to the hierarchical levels by means of the intraclass correlation coefficient (ICC) and the median odds ratio (MOR), as well as the fixed effects of the covariates through ORs and their 95% CIs. We assessed the quality of the models by means of the Akaike information criterion (AIC). We fitted the models with a stepwise approach, starting with the null model without covariates, which explored the variance as a function of the different levels and continuing with partial models until reaching the saturated full model. We adjusted each of the partial models with backward regression, excluding variables that were not near statistical significance and that did not modify the ICC of the model by more than 10%. Lastly, the full model included the variance explained by the levels and the covariates found to be statistically significant in the partial models.
We defined statistical significance as a P value of less than 0.05 and nearing statistical significance as a P value of less than 0.10.
The statistical analysis was conducted with the software packages SPSS version 20 and Stata version 14.
We calculated that to achieve the primary objective of the study with a precision of 7%, assuming a prevalence of 25%4 for a level of confidence of 95%, we needed to include a minimum of 147 valid responses.
Ethical considerationsThe study was approved by the ethics committee for research with medicines of the hospital to which the principal investigator was affiliated.
Participation in the survey, through an online questionnaire sent to participants, was anonymous, and started with a section that detailed the conditions of participation, actively seeking informed consent. Questionnaire data were dumped to a database under the custody of the principal investigator.
ResultsWe recruited 32 hospitals in 12 autonomous communities (Appendix B4) and submitted links to the survey to 466 physicians. We received 392 completed responses (none of which were excluded), which corresponds to a response rate of 84.1%.
Sample characteristicsThe mean age of the respondents was 39.2 years (standard deviation [SD], 7.9), with a range of 28–66 years, 296 were female (75.5%) and 96 male (24.5%). Of the total sample, 121 paediatricians reported exclusive dedication to emergency care (30.9%), and 112 (28.6%) that they fit the definition of PEC specialist.
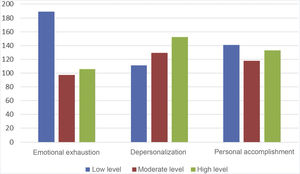
Prevalence of burnout syndromeThe scale identified BOS in 143 of the 392 participants, which corresponds to a prevalence of BOS of 36.5% (95% CI, 31.7 %–41.2%). The dimension that was in the pathological range most frequently was depersonalization (n = 281; 71.7%; 95% CI, 67.2 %–76.1%), followed by personal accomplishment (n = 259; 66.1%; 95% CI, 61.4 %–70.8%) and emotional exhaustion (n = 203; 51.8%; 95% CI, 46.8 %–56.7%) (Table 2 and Fig. 1). In 341 participants (87.0%), at least one dimension was in the pathological range.
Subscale levels in relation to burnout syndrome (392 submitted responses).
| Low n (%) | Moderate n (%) | High n (%) | Score mean ± SD | |
|---|---|---|---|---|
| Emotional exhaustion | 189 (48.2%) | 97 (24.7%) | 106 (27.0%) | 21.1 ± 10.6 |
| Depersonalization | 111 (28.3%) | 129 (32.9%) | 152 (38.8%) | 8.6 ± 5.0 |
| Personal accomplishment | 141 (36.0%) | 118 (30.1%) | 133 (33.9%) | 35.5 ± 8.0 |
Values expressed as absolute frequencies and percentages. The levels of each subscale that define burnout syndrome are presented in boldface.
The results of the univariate analysis on the association of BOS with different social, family-related, demographic, occupational and reward-related factors are shown in Appendix B5.
Multivariate analysis (Table 3)Random effects. The ICC showed that up to 10.4% of the variance in the development of BOS could be explained by differences between hospitals when controlling for individual-dependent factors (model 2). With the introduction of hospital-level covariates (model 3), the ICC dropped to 0, and it remained at 0 in the full model (model 5) (Table 3).
Analysis of random and fixed effects through different multivariate multilevel logistic regression models.
| Model 1 (null) | Model 2 | Model 3 | Model 4 | Model 5 (saturated) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| ICC | MOR | ICC | MOR | ICC | MOR | ICC | MOR | ICC | MOR | |
| Hospital level | 0.085 | 1.69 | 0.104 | 1.80 | 0.000 | 1.000 | 0.075 | 1.636 | 0.000 | 1.000 |
| Autonomous community level | 0.000 | 1.00 | 0.000 | 1.00 | 0.001 | 1.040 | 0.000 | 1.000 | 0.008 | 1.169 |
| AIC | 515.390 | 464.606 | 478.656 | 507.137 | 446.954 | |||||
| Adjusted OR (95% CI) | P | Adjusted OR (95% CI) | P | Adjusted OR (95% CI) | P | Adjusted OR (95% CI) | P | Adjusted OR (95% CI) | P | |
|---|---|---|---|---|---|---|---|---|---|---|
| Age < 40 years | 0.76 (0.29−1.96) | .566 | ||||||||
| Has children | 0.89 (0.51−1.57) | .697 | ||||||||
| Has regular living expenses | 1.11 (0.51−2.42) | .794 | ||||||||
| Lives with < 3 people | 1.72 (0.62−4.78) | .300 | ||||||||
| Has no circle of friends | 2.39 (1.03−5.59) | .044 | 2.57 (1.10−5.97) | .029 | ||||||
| Extroverted personality | Ref | |||||||||
| Ambivert personality | 1.00 (0.57−1.75) | .992 | ||||||||
| Introverted personality | 1.05 (0.47−2.35) | .896 | ||||||||
| Optimistic | Ref | |||||||||
| Neither optimistic nor pessimistic | 1.63 (0.97−2.74) | .064 | ||||||||
| Pessimistic | 1.75 (0.74−4.14) | .206 | ||||||||
| Feels content | 0.86 (0.37−1.98) | .715 | ||||||||
| No problems | Ref | Ref | ||||||||
| Problems at work | 1.21 (0.59−2.49) | .602 | 1.27 (0.62−2.62) | .518 | ||||||
| Problems in other spheres | 1.14 (0.59−2.20) | .699 | 1.20 (0.63−2.31) | .580 | ||||||
| Problems at work and other spheres | 3.00 (1.57−5.74) | .001 | 3.06 (1.60−5.88) | .001 | ||||||
| Takes anti-anxiety/antidepressant medication due to occupational stress | 1.10 (0.47−2.58) | .835 | ||||||||
| Takes anti-anxiety/antidepressant medication for other reasons | 1.95 (1.10−3.46) | .023 | 1.73 (0.98−3.04) | .058 | ||||||
| Takes medication for insomnia due to occupational stress | 1.27 (0.67−2.40) | .458 | ||||||||
| Takes medication for insomnia for other reasons | 1.44 (0.81−2.57) | .215 | ||||||||
| Work experience ≤ 9 years | 2.28 (1.35−3.85) | .002 | 2.31 (1.37−3.90) | .002 | ||||||
| Has received trainings | 0.71 (0.38−1.33) | .286 | ||||||||
| Professional recognition from coworkers | 0.50 (0.30−0.82) | .007 | 0.48 (0.30−0.79) | .004 | ||||||
| Professional recognition from immediate supervisor | 0.59 (0.39−0.91) | .016 | 0.62 (0.41−0.93) | .023 | ||||||
| Satisfied with relationship with coworkers | 0.93 (0.57−1.50) | .761 | ||||||||
| Satisfied with relationship with immediate supervisor | 1.08 (0.70−1.67) | .735 | ||||||||
| The emergency care setting depends on the paediatrics department | 3.74 (1.91−7.33) | <.001 | 3.81 (1.85−7.85) | <.001 | ||||||
| There is always an on-call emergency care specialist in the premises | 2.47 (1.21−5.06) | .013 | 3.53 (1.62−7.73) | .002 | ||||||
| ≥ 28 emergencies per on-call physician per day | 2.10 (1.12−3.96) | .021 | 2.05 (1.01−4.16) | .048 | ||||||
| Enough time in schedule for activities other than patient care | Ref | |||||||||
| 1.30 (0.24−7.01) | .758 | |||||||||
| No time in schedule for activities other than patient care | 1.93 (0.51−7.30) | .333 | ||||||||
| Enough time in schedule for activities other than patient care | 1.79 (0.45−7.02) | .406 | ||||||||
| Professional recognition from the institution | 0.49 (0.36−0.67) | <.001 | 0.76 (0.52−1.11) | .160 | ||||||
| Temporary contract | 2.19 (1.34−3.58) | .002 | 1.34 (0.71−2.54) | .369 |
AIC, Akaike information criterion; CI, confidence interval; ICC, intraclass correlation coefficient; MOR, median odds ratio; OR, odds ratio.
Model 1: model 1, influence of levels in the variance of burnout syndrome.
Model 2: includes covariates at the individual level.
Model 3: includes covariates at the hospital level.
Model 4: includes covariates at the autonomous community level.
Model 5: full model, random and fixed effects of the covariates with a significant association in models 2–4.
The results for variables included in the full model are presented in boldface.
The differences between autonomous communities were barely relevant, with an ICC of 0.008 in the full model. The full model turned out to be the one that offered the most precise information based on the AIC.
Fixed effects. After adjusting the different models, we found that not having a stable circle of friends, having problems both in and out of the workplace compared to not having any and a work experience of 9 years or less were independent risk factors at the individual level. In addition, feeling recognised as a professional by coworkers and the immediate supervisor were factors that appeared to have a protective effect.
At the hospital level, the operation of the PEC as a subdivision dependent on the department of paediatrics, the presence of an on-call emergency care specialist around the clock and the management of at least 28 emergency care episodes in 24 h by the on-call physician were also independent risk factors for BOS.
DiscussionOurs is the first multicentre study on BOS of nearly nationwide scope conducted in Spain in physicians specialised in paediatrics and to explore factors associated with BOS with a multivariate, multilevel approach. We were able to obtain a large sample with a very high response rate and included the largest number of variables potentially associated with BOS ever analysed in a published study.
Although the MBI is the scale used most widely in the literature for the assessment of BOS, many different criteria have been proposed to define it. As a result, there is substantial variation in the reported prevalence of BOS, ranging from 7.1% to 76.1%.12,13 We found a higher prevalence in our sample compared to most other studies, in which it ranges between 20% and 25%,14–16 including one conducted in a similar population that applied the same diagnostic criteria, although in the United States.4 In any case, it is alarming that more than one third of clinicians exhibited moderate to high levels of burnout in the 3 dimensions used by Maslach and Jackson to define BOS and that nearly 90% had at least one dimension indicating moderate to high levels of burnout.
Individual traits such as anxiety or depression, which could have an impact on the emotional exhaustion dimension,17 and introversion were identified as risk factors for BOS.3 Similarly, a low emotional stability, psychological tension, neuroticism, among other personality traits, and mental health in general have been repeatedly described as factors associated with BOS.18–20 Our findings suggest that living in a conflictive environment with stressors in different spheres and underlying mental health problems (requiring treatment with antidepressant or anti-anxiety medication) can set the framework for the development of BOS.
On the other hand, coping mechanisms, such as socialising and having the support of family and friends to manage stressors,12,14,18–20 free time for personal leisure,21 hobbies and regular physical activity12 could have a protective effect. Our findings support this hypothesis, although the effect of families, significant others or children did not seem as important as proposed by other authors12,19,20 compared to having a circle of friends to spend time with regularly. This source of social support reduces or eliminates stressful stimuli, modifies how stressors are perceived, enhances coping mechanisms and improves mood, motivation and self-esteem.22
Some meta-analyses have identified age—in terms of youth and professional inexperience—as a predisposing factor for professional burnout.19,20 Although this association is gradual, in the sample under study we found the highest decrease in BOS after 9 years of work experience. It is hypothesised that individuals are more motivated and dedicated in the early years of their careers, which can turn against them due to a lack of professional recognition and the distancing from the social support network. As years go by, in addition to growing professional skills that increase their effectiveness, they go through experiences and develop adaptive strategies to cope with challenging situations, which increases resilience and the ability to tolerate difficulties in the workplace.23,24
When it came to occupational variables, we did not find evidence of the previously described association with the number of worked hours or on-call shifts a month,19,20 probably because these were quite homogeneous among the surveyed providers; however, the data did show that a high workload, in terms of the number of managed patients, has a negative impact on clinicians.
In addition to their amount, the nature of the tasks that professionals are responsible for plays a significant role in BOS.22 In Spanish hospitals, PEC is not organised as an independent department or unit or staffed with dedicated specialists in paediatric emergency medicine, and the providers that deliver care in these settings tend to be specialists in other fields. This is not the case in independent emergency departments, which tend to have better human and material resources and where care delivery is probably better organised, both factors which are also associated with BOS.20
In our sample, in spite of the dissemination of the survey through the RISeuP-SPERG, only 9 out of 32 participating hospitals (28%) had an on-call emergency care specialist in the premises at all times. This probably occurs in hospitals that manage more complex patients, and this very need of highly qualified personnel may be one of the contributing factors to higher prevalence of BOS observed under these conditions.
Working conditions also affect the dimensions of emotional exhaustion and depersonalization.11,20,25 Our study found that receiving recognition for one’s efforts and work from the closest professional circle (coworkers and immediate supervisor) plays a more important role than the atmosphere at work, institutional recognition and even employment stability. Similarly, in a recently published study that proposes a predictive model, not feeling appreciated by patients and not feeling appreciated by supervisors were two of the independent risk factors for BOS.26
An aspect worth considering is the extent to which these factors can predict the presence of BOS in different work settings. The multilevel analysis contributed some information on the subject, and allowed us to conclude that, in our sample, the variance in the presence of BOS, after controlling for those factors, could not be attributed to other differences between hospitals or autonomous communities, so that BOS would be chiefly determined by other factors at the level of the individual. This is particularly useful for the purpose of developing strategies to prevent and treat BOS, as it suggests that they will have the same impact independently of where they are implemented, and their results will only vary based on other individual-dependent factors.
In light of these findings, strategies for the early detection of BOS should be developed by screening for personality traits related with a propensity to anxiety or depression, programmes implemented to combat occupational stress by providing workers with coping skills27,28 and work-life balance promoted to ensure that clinicians have time for themselves and to strengthen their interpersonal relationships. Furthermore, from an organizational standpoint, the acquisition and improvement of knowledge and skills to tackle challenges in care delivery, the optimization of human and material resources to prevent excessive workloads and giving professionals meaningful recognition would improve wellbeing in the workplace and help fight burnout.1,11,29,30
LimitationsOur study has relevant limitations, starting with the characteristics of the participants, since the distribution of the survey through a scientific society devoted to emergency medicine implies a stronger connection and commitment of these physicians compared to those in hospitals where none are affiliated to such a society. Similarly, there is a risk of voluntary-response bias and physicians experiencing burnout may have disproportionally chosen to participate, although the high response rate—of approximately 85%—may have minimised this risk.
The period when questionnaires were completed (October to January) is a time of year when there is a high demand for health care services, which may have affected the results. Furthermore, the study was conducted before the COVID-19 pandemic, so it does not reflect the impact this pandemic has had on providers.
Although the questionnaire included items that explored different personality traits of the respondents more or less explicitly, it is impossible to cover all the factors that may be involved in burnout. For the same reason, we did not explore specific aspects of the professional activity of clinicians who delivered emergency care on a part-time basis, aspects that could also contribute to explaining BOS, although the variables considered in the study were able to explain the variance at the centre and autonomous community levels.
ConclusionLevels indicative of moderate or high levels of burnout in all three dimensions of the MBI were frequent among doctors specialised in paediatrics who worked in paediatric emergency care in Spain, and practically all exhibited levels suggestive of a moderate or high level of burnout in at least one subscale. The organizational structure of the department and the workload were, along with professional experience, recognition by coworkers and supervisors, problems in and out of the workplace, symptoms of anxiety or depression and social support, the main factors associated with BOS in this collective. On the other hand, we did not find relevant differences in prevalence between different hospitals or autonomous communities, so universal measures should be implemented to ameliorate risk factors for BOS.
FundingThere was no remuneration for this study. None of the main or collaborating researchers have received any payment for their participation in the development of the study and data collection and processing. The study did not receive any public or private funding.
Conflicts of interestThe authors have no conflicts of interest to declare.
Annex C. Members of the Working Group for the Study of burnout of the para Research Network of the Sociedad Española de Urgencias Pediátricas (RISeuP-SPERG)Ana Pérez Villena (Hospital Universitario Infanta Sofía); Yordana Acedo Alonso (Hospital Universitario Cruces); Elvira González Salas (Hospital Universitario de Salamanca); Estefanía Romero Castillo (Hospital Universitario Puerta del Mar); Anna Orejuela Ribera (Hospital Universitario Joan XXIII); Ramón Fernández Álvarez (Hospital Universitario de Cabueñes); Maria Ángeles García Herrero (Hospital Universitario Príncipe de Asturias); Ana Muñoz Lozón (Hospital Universitario Infanta Leonor); Daniel de la Rosa Sánchez (Hospital Universitario Insular de Canarias); Patricia del Río Martínez (Hospital de Mendaro); Mariano Plana Fernández (Hospital Universitario de Barbastro); Virginia Gómez Barrena (Hospital Universitario Miguel Servet); Ana Isabel Mohedas Tamayo (Hospital Universitario de Fuenlabrada); Carmen Hinojosa Mateo (Hospital Universitario del Tajo); Roberto Velasco Zúñiga (Hospital Universitario Río Hortega); Clàudia Coderch Ciurans (Consorci Sanitari de Terrassa); José Antonio Ruiz Domínguez (Hospital Universitario La Paz); Sebastià González Peris (Hospital Universitario Vall d’Hebron); Carlos Miguel Angelats Romero (Hospital Francesc de Borja); Neus Pociello Almiñana (Hospital Universitario Arnau de Vilanova); Ana Pizá Oliveras (Hospital Universitario Mútua de Terrassa); José Antonio Alonso Cadenas (Hospital Universitario Niño Jesús); Cristina Parra i Cotanda (Hospital Universitario Sant Joan de Déu); Izaskun Olaciregui Echenique (Hospital Universitario Donostia); Sara Pons Morales (Hospital Universitario Doctor Peset); Carmen Baltasar Navas (Hospital Universitario Virgen del Rocío); Sandra Yáñez Mesía (Hospital Universitario de A Coruña); María Reyes Balcells (Hospital Universitario Sant Pau); Nuria Gilabert Iriondo (Hospital Universitario Son Espases); Juan Luis Santos Pérez (Hospital Universitario Virgen de las Nieves); Sara Moralo García (Hospital Universitario Virgen de la Arrixaca); Garazi Plaza Fraga (Hospital Universitario de Basurto).
Previous presentation: this study was presented as an oral communication at the XXVI annual meeting of the Sociedad Española de Urgencias de Pediatría (SEUP), June 2022. It presents the doctoral dissertation of the first author, which has yet to be defended.
El resto de autores integrantes del Grupo para el estudio del Burnout de la Red de Investigación de la Sociedad española de Urgencias Pediátricas (RISeuP-SPERG) se presentan en Anexo.