Homecare (HC) is a service offering home medical and nursing care to the patient at home in equal quantity and quality as in the hospital. The aim of the article is to describe the changes in the HC of preterm and full-term low-birth-weight infants in our department from 2002 to 2014.
Material and methodsThe HC database is revised. The characteristics of the newborns and the social characteristics of the family in three consecutive time periods are analysed. A satisfaction survey of parents is also presented.
ResultsThe main changes in HC include a decrease in the weight at discharge (from 1880g in the 2002–2006 period to 1850g in the 2011–2014 period; P=.006) and at the end of HC (from 2187g to 2163g; P=.001), an increase in the duration of HC (from 10 to 11 days; P=.007) and a lower incidence of new hospitalisation (from 3.4% to 1.3%; P=.019) The social characteristics of the family show a higher maternal age with more previous alive children, a family context better suited with a more appropriate housing, and an increase in exclusive breastfeeding at hospital discharge (from 25.5% to 49.0%; P<.001). The overall assessment of the programme is ≥7/10 in 98.8% of responses.
ConclusionsThe results of the HC of preterm and low-birth-weight infants have improved over time, saving approximately 10–11 days of hospitalisation, and without compromising the quality of care or reducing family satisfaction.
La atención domiciliaria (AD) se caracteriza por ofrecer al paciente en su domicilio atención médica y enfermera en igual cantidad y calidad que en el hospital. El objetivo es describir los cambios en la evolución de la AD del neonato en nuestro servicio, desde 2002 hasta 2014.
Material y métodosSe revisa la base de datos de AD analizando las características propias de la AD y las características sociales de la familia en 3 periodos consecutivos. También se presenta una encuesta de satisfacción de los padres.
ResultadosEn la evolución de la AD en los 3 periodos cabe destacar una disminución del peso al alta hospitalaria (de 1.880g en el periodo 2002-2006 a 1.850g en el periodo 2011-2014; p=0,006) y al alta definitiva (de 2.187g a 2.163g; p=0,001), un aumento de la duración de la AD (de 10 a 11 días; p=0,007) y una menor incidencia de rehospitalizaciones (del 3,4 al 1,3%; p=0,019) Las características sociales de la familia muestran una mayor edad materna con más hijos vivos previos, un contexto familiar mejor adaptado en una vivienda más correcta y un aumento de la lactancia materna exclusiva al alta hospitalaria (del 25,5 al 49,0%; p<0,001). La valoración global del programa es ≥ 7/10 en el 98,8% de respuestas.
ConclusionesLos resultados de la AD del prematuro y recién nacido de bajo peso han ido mejorando a lo largo del tiempo, permitiendo ahorrar aproximadamente 10-11 días de ingreso hospitalario, sin menoscabar la calidad asistencial ni disminuir la satisfacción familiar.
Preterm birth and low birth weight for gestational age are associated with increased morbidity and length of stay in newborns, compared to those born to term with adequate weights. These circumstances lead to separation from the parents, hindering bonding.1 One of the goals of neonatal care is to put infants in the care of their parents as early as possible.
Family-centred care is a model of health care delivery that focuses on the acknowledgement of the family as a protective and vital factor in patient care.2 It is based on the participation and cooperation of family members in an atmosphere of dignity and respect, working collaboratively to improve neonatal outcomes during hospitalisation. The key elements of this model are communication, information and support. Family-centred care has progressively been integrated in neonatal intensive care settings, and home care (HC) programmes for preterm or low-birth-weight infants are an important means to achieve the earliest possible integration of the infant in the family.
Home care consists in offering the patient medical and nursing services at home in equal quantity and quality as those offered in the hospital, with the latter retaining clinical, logistic (medication, etc.), financial and legal responsibility over care. Home care is one of the emerging trends in neonatal care in developed countries3–5 such as the United States,6 countries in northern Europe7,8 and France.9 The first references to HC published in Spain, are from 1993 and 1997 and involve the Hospital 12 de Octubre de Madrid,10,11 which launched its programme in 1986. The pioneering hospital in Catalonia was the Hospital Clínic (Maternity Unit), which introduced HC in 2002.12,13
The HC programme improves the relationship with parents and their satisfaction, as it restores normalcy in the family,14 facilitates breastfeeding (BF),15 is associated with greater weight gain in the newborn (NB).16 It improves developmental outcomes17 and carries a lower risk of infection; it also allows a more individualised approach to health education18 and the reorganisation of health care resources in ways that are more satisfactory to the users.
The aim of this study was to describe any changes that may have taken place in the HC of preterm infants in our neonatal care department from its introduction to present, the social characteristics of the families, and a parental satisfaction survey.
Materials and methodsWe included all infants that received HC between 2002 and 2014 that met the following criteria during their hospital stay: postmenstrual age of 33 weeks or more, clinically stable, having overcome acute conditions in the early neonatal period, adequate thermoregulation, being free of apnoea without medication, and ability to feed by suckling. The parents had to be able to care for the NB, reside in the Barcelona metropolitan area and sign the informed consent form. During hospitalisation, parents underwent specific health care education and received an informational brochure about the HC programme. At discharge from hospital, they were given a phone number that they could call for consultations around the clock, which was staffed by the HC programme nurse during office hours and otherwise by the neonatal unit nurses or the on-call paediatrician. A nurse visited the NB at home two or three times a week. Whenever the patient needed to be seen by the paediatrician, the visit took place in the emergency department or the outpatient clinic, and a bed was reserved for the patient in the neonatal unit in case readmission was required. Once the infant reached a weight of 2100g, he or she was seen by the paediatrician, who produced the corresponding HC report, and referred to the primary care paediatrician.
The variables we analysed concerning HC were: neonatal status (preterm, low birth weight for gestational age based on the 10th percentile of the Catalonian neonatal curves19), sex, point of origin (neonatal care unit or maternity ward), weight at discharge from hospital, HC characteristics (nurse visits and their duration, time spent travelling and cost of taxi fares, medication given, weight increase in the week prior to hospital discharge and in the first week spent at home and their difference, weight at final discharge from the programme, duration of HC and total length of stay in the programme including the initial hospital stay), complications during HC (visits to emergency department or paediatrician, phone calls, hospital readmission and discontinuations of HC and the reasons for them) and level of satisfaction of the family.
The variables defining the social characteristics of the family were: maternal age, previous live births, ethnicity, educational attainment, parental occupation, family environment, housing conditions and type of nutrition at discharge.
To analyse the changes that have taken place in the HC over its twelve years of operation, we divided this time into three four-year periods: 2002–2006 (561 patients), 2007–2010 (515 patients) and 2011–2014 (398 patients). The neonates included in each period correspond to all admitted newborns that met the inclusion criteria for the HC programme, with no exceptions.
In this study, we also analysed a satisfaction survey that parents filled out on a voluntary basis and dropped in the mailbox after the last visit before discharge at the outpatient clinic. We collected responses to this survey between January 2004 and December 2012 for a total of 1142 newborns in HC belonging to 536 families, on account of the high proportion of multiple pregnancies. The survey explored the opinion of parents regarding the programme. It asked parents to rate their response to being offered HC, the informational brochure, the health education talks, the home visits, the outpatient clinic visits, and the programme overall.
In the statistical analysis, we determined that none of the quantitative variables was normally distributed using the Kolmogorov-Smirnoff test. Consequently, we analysed these variables by means of nonparametric tests, describing them with the median (50th percentile) and the interquartile range (25th–75th percentile) and conducting the bivariate analysis for each of them in relation to the three time periods with the Kruskal–Wallis test. We compared weight gain in the week preceding discharge to weight gain in the first week at home by means of the Wilcoxon test for paired samples. We described qualitative variables as percentages for each of the categories, and used the linear-by-linear association chi squared test for the bivariate analysis. We set the level of statistical significance at P<.05.
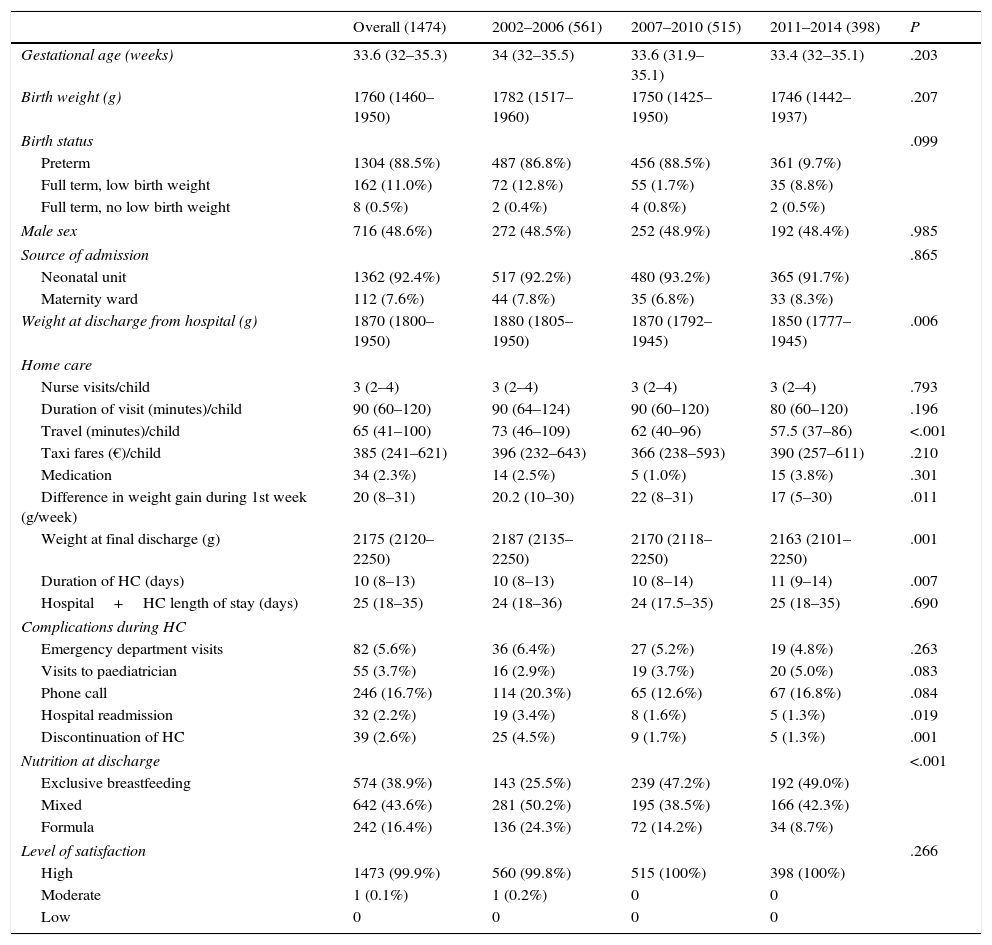
ResultsBetween December 1, 2002 and December 31, 2014, 7403 patients were admitted to the neonatal unit, and the parents of 1474 (20%) agreed to participate in the HC programme. Their general characteristics are summarised in the first column of Table 1. Of the patients in the sample, 51.6% were singletons, 42.7% were twins and 5.7% triplets. Fifty-six NBs had a weight of 2100g or more at discharge and were nevertheless included in the HC programme. These exceptions were made on account of being a twin (with a low-birth-weight twin) in 28, home monitoring in two (one had bronchopulmonary dysplasia), family anxiety due to previous morbidity in three (one had had hypoxic–ischaemic encephalopathy), antibiotic treatment in four, withdrawal syndrome in one, social problems in five, and current morbidity in three (positive respiratory syncytial virus test, suspected Hirschsprung disease, lung malformation). Neurologic followup was indicated in 485 of the 1385 (35%).
Characteristics of infants in homecare (HC).
| Overall (1474) | 2002–2006 (561) | 2007–2010 (515) | 2011–2014 (398) | P | |
|---|---|---|---|---|---|
| Gestational age (weeks) | 33.6 (32–35.3) | 34 (32–35.5) | 33.6 (31.9–35.1) | 33.4 (32–35.1) | .203 |
| Birth weight (g) | 1760 (1460–1950) | 1782 (1517–1960) | 1750 (1425–1950) | 1746 (1442–1937) | .207 |
| Birth status | .099 | ||||
| Preterm | 1304 (88.5%) | 487 (86.8%) | 456 (88.5%) | 361 (9.7%) | |
| Full term, low birth weight | 162 (11.0%) | 72 (12.8%) | 55 (1.7%) | 35 (8.8%) | |
| Full term, no low birth weight | 8 (0.5%) | 2 (0.4%) | 4 (0.8%) | 2 (0.5%) | |
| Male sex | 716 (48.6%) | 272 (48.5%) | 252 (48.9%) | 192 (48.4%) | .985 |
| Source of admission | .865 | ||||
| Neonatal unit | 1362 (92.4%) | 517 (92.2%) | 480 (93.2%) | 365 (91.7%) | |
| Maternity ward | 112 (7.6%) | 44 (7.8%) | 35 (6.8%) | 33 (8.3%) | |
| Weight at discharge from hospital (g) | 1870 (1800–1950) | 1880 (1805–1950) | 1870 (1792–1945) | 1850 (1777–1945) | .006 |
| Home care | |||||
| Nurse visits/child | 3 (2–4) | 3 (2–4) | 3 (2–4) | 3 (2–4) | .793 |
| Duration of visit (minutes)/child | 90 (60–120) | 90 (64–124) | 90 (60–120) | 80 (60–120) | .196 |
| Travel (minutes)/child | 65 (41–100) | 73 (46–109) | 62 (40–96) | 57.5 (37–86) | <.001 |
| Taxi fares (€)/child | 385 (241–621) | 396 (232–643) | 366 (238–593) | 390 (257–611) | .210 |
| Medication | 34 (2.3%) | 14 (2.5%) | 5 (1.0%) | 15 (3.8%) | .301 |
| Difference in weight gain during 1st week (g/week) | 20 (8–31) | 20.2 (10–30) | 22 (8–31) | 17 (5–30) | .011 |
| Weight at final discharge (g) | 2175 (2120–2250) | 2187 (2135–2250) | 2170 (2118–2250) | 2163 (2101–2250) | .001 |
| Duration of HC (days) | 10 (8–13) | 10 (8–13) | 10 (8–14) | 11 (9–14) | .007 |
| Hospital+HC length of stay (days) | 25 (18–35) | 24 (18–36) | 24 (17.5–35) | 25 (18–35) | .690 |
| Complications during HC | |||||
| Emergency department visits | 82 (5.6%) | 36 (6.4%) | 27 (5.2%) | 19 (4.8%) | .263 |
| Visits to paediatrician | 55 (3.7%) | 16 (2.9%) | 19 (3.7%) | 20 (5.0%) | .083 |
| Phone call | 246 (16.7%) | 114 (20.3%) | 65 (12.6%) | 67 (16.8%) | .084 |
| Hospital readmission | 32 (2.2%) | 19 (3.4%) | 8 (1.6%) | 5 (1.3%) | .019 |
| Discontinuation of HC | 39 (2.6%) | 25 (4.5%) | 9 (1.7%) | 5 (1.3%) | .001 |
| Nutrition at discharge | <.001 | ||||
| Exclusive breastfeeding | 574 (38.9%) | 143 (25.5%) | 239 (47.2%) | 192 (49.0%) | |
| Mixed | 642 (43.6%) | 281 (50.2%) | 195 (38.5%) | 166 (42.3%) | |
| Formula | 242 (16.4%) | 136 (24.3%) | 72 (14.2%) | 34 (8.7%) | |
| Level of satisfaction | .266 | ||||
| High | 1473 (99.9%) | 560 (99.8%) | 515 (100%) | 398 (100%) | |
| Moderate | 1 (0.1%) | 1 (0.2%) | 0 | 0 | |
| Low | 0 | 0 | 0 | 0 | |
Median (interquartile range). Absolute frequency (%).
Thirty-four infants received pharmacological treatment at home, including seven treated with erythropoietin and some that received shots of vaccines and palivizumab. We analysed weight gain in the hospital the week prior to discharge to HC and in the first week of HC, and the difference between them (weight gain difference in grams/week) was statistically significant (P=.011).
As for significant complications during HC, the programme had to be discontinued in 39 infants (2.65%), which was due to infection in 11 (3 cases of sepsis, 3 of urinary tract infection, 5 of respiratory infection), gastrointestinal problems in nine (7 cases of gastroesophageal reflux or choking, 2 due to vomiting), hyperbilirubinaemia requiring phototherapy in 10, sudden death in one, hypothermia of the newborn in one, inguinal hernia in one, social problems in one, and a change in residence in five.
Table 1 shows the changing trends in the HC variables under study during the three consecutive periods. The most salient changes involved a decrease in weight at the time of hospital discharge and at final discharge from the programme, an increase in the rate of exclusive BF, and a reduction in the rate of formula feeding at discharge from hospital, an increase in the duration of BF associated with a reduction in the time spent travelling, a lower comparative weight gain in the first week of HC, and a reduced rate of hospital readmission and HC discontinuation.
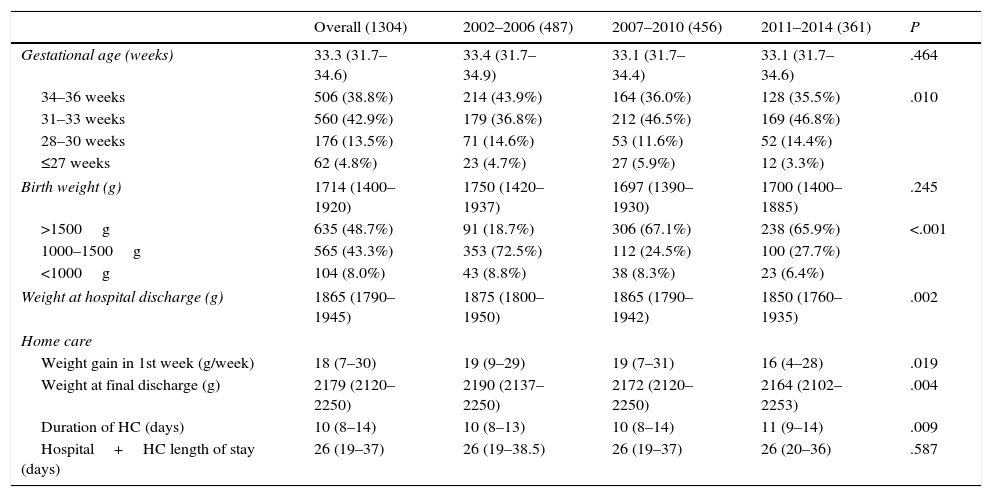
Table 2 summarises the main characteristics of the 1304 preterm infants admitted to the HC programme, who corresponded to 88.5% of the participants in the study. Due to this high percentage, the results obtained for this subset are practically the same as those for the overall sample. When we analysed the data for preterm infants in HC for each of the three time periods, we observed that over time, the infants were increasingly immature and weighed less at birth and at discharge from hospital, and that the duration of HC increased, although the total length of stay (hospital and home care) remained stable.
Characteristics of preterm infants in homecare (HC).
| Overall (1304) | 2002–2006 (487) | 2007–2010 (456) | 2011–2014 (361) | P | |
|---|---|---|---|---|---|
| Gestational age (weeks) | 33.3 (31.7–34.6) | 33.4 (31.7–34.9) | 33.1 (31.7–34.4) | 33.1 (31.7–34.6) | .464 |
| 34–36 weeks | 506 (38.8%) | 214 (43.9%) | 164 (36.0%) | 128 (35.5%) | .010 |
| 31–33 weeks | 560 (42.9%) | 179 (36.8%) | 212 (46.5%) | 169 (46.8%) | |
| 28–30 weeks | 176 (13.5%) | 71 (14.6%) | 53 (11.6%) | 52 (14.4%) | |
| ≤27 weeks | 62 (4.8%) | 23 (4.7%) | 27 (5.9%) | 12 (3.3%) | |
| Birth weight (g) | 1714 (1400–1920) | 1750 (1420–1937) | 1697 (1390–1930) | 1700 (1400–1885) | .245 |
| >1500g | 635 (48.7%) | 91 (18.7%) | 306 (67.1%) | 238 (65.9%) | <.001 |
| 1000–1500g | 565 (43.3%) | 353 (72.5%) | 112 (24.5%) | 100 (27.7%) | |
| <1000g | 104 (8.0%) | 43 (8.8%) | 38 (8.3%) | 23 (6.4%) | |
| Weight at hospital discharge (g) | 1865 (1790–1945) | 1875 (1800–1950) | 1865 (1790–1942) | 1850 (1760–1935) | .002 |
| Home care | |||||
| Weight gain in 1st week (g/week) | 18 (7–30) | 19 (9–29) | 19 (7–31) | 16 (4–28) | .019 |
| Weight at final discharge (g) | 2179 (2120–2250) | 2190 (2137–2250) | 2172 (2120–2250) | 2164 (2102–2253) | .004 |
| Duration of HC (days) | 10 (8–14) | 10 (8–13) | 10 (8–14) | 11 (9–14) | .009 |
| Hospital+HC length of stay (days) | 26 (19–37) | 26 (19–38.5) | 26 (19–37) | 26 (20–36) | .587 |
Median (interquartile range). Absolute frequency (%).
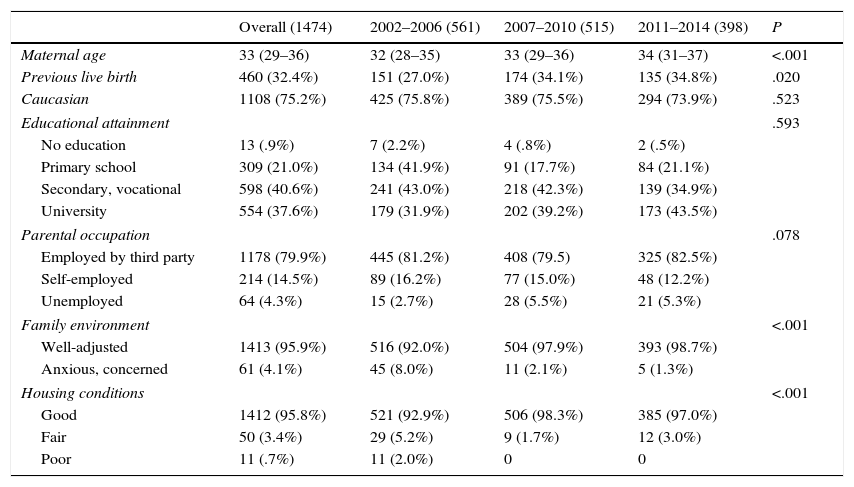
Table 3 summarises the social characteristics of the families of the NBs admitted to the HC programme, and also shows the changing trends during the three consecutive periods under study. The main changes include an increase in maternal age and in the number of previous live births, and better-adjusted families in more adequate housing.
Social characteristics of the families of the infants in home care (HC).
| Overall (1474) | 2002–2006 (561) | 2007–2010 (515) | 2011–2014 (398) | P | |
|---|---|---|---|---|---|
| Maternal age | 33 (29–36) | 32 (28–35) | 33 (29–36) | 34 (31–37) | <.001 |
| Previous live birth | 460 (32.4%) | 151 (27.0%) | 174 (34.1%) | 135 (34.8%) | .020 |
| Caucasian | 1108 (75.2%) | 425 (75.8%) | 389 (75.5%) | 294 (73.9%) | .523 |
| Educational attainment | .593 | ||||
| No education | 13 (.9%) | 7 (2.2%) | 4 (.8%) | 2 (.5%) | |
| Primary school | 309 (21.0%) | 134 (41.9%) | 91 (17.7%) | 84 (21.1%) | |
| Secondary, vocational | 598 (40.6%) | 241 (43.0%) | 218 (42.3%) | 139 (34.9%) | |
| University | 554 (37.6%) | 179 (31.9%) | 202 (39.2%) | 173 (43.5%) | |
| Parental occupation | .078 | ||||
| Employed by third party | 1178 (79.9%) | 445 (81.2%) | 408 (79.5) | 325 (82.5%) | |
| Self-employed | 214 (14.5%) | 89 (16.2%) | 77 (15.0%) | 48 (12.2%) | |
| Unemployed | 64 (4.3%) | 15 (2.7%) | 28 (5.5%) | 21 (5.3%) | |
| Family environment | <.001 | ||||
| Well-adjusted | 1413 (95.9%) | 516 (92.0%) | 504 (97.9%) | 393 (98.7%) | |
| Anxious, concerned | 61 (4.1%) | 45 (8.0%) | 11 (2.1%) | 5 (1.3%) | |
| Housing conditions | <.001 | ||||
| Good | 1412 (95.8%) | 521 (92.9%) | 506 (98.3%) | 385 (97.0%) | |
| Fair | 50 (3.4%) | 29 (5.2%) | 9 (1.7%) | 12 (3.0%) | |
| Poor | 11 (.7%) | 11 (2.0%) | 0 | 0 | |
Median (interquartile range). Absolute frequency (%).
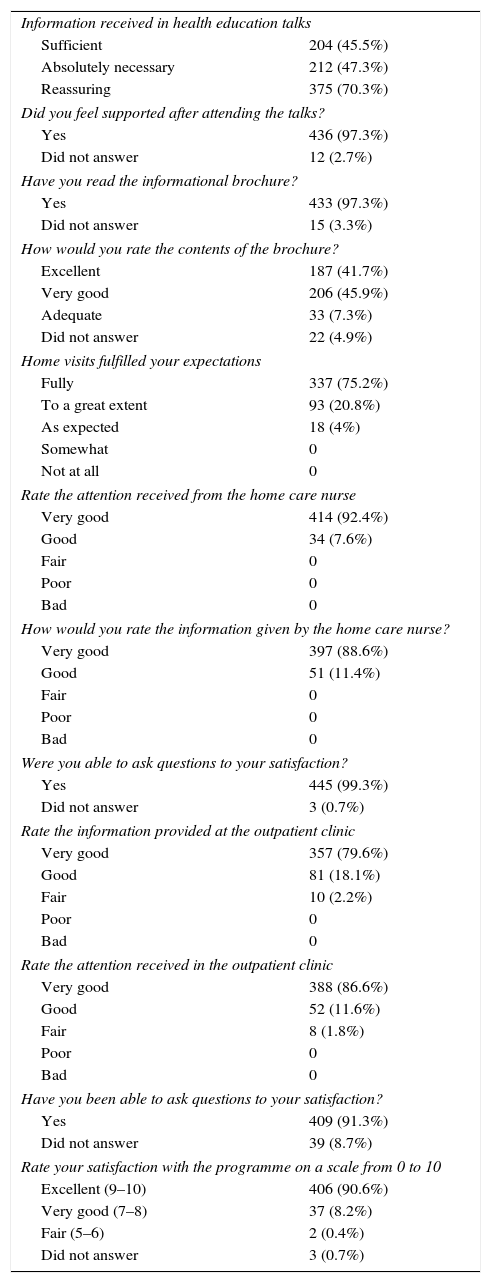
Table 4 presents the results of the survey completed by 448 families (83.6% of those invited to participate). When parents were asked in an open-ended question how they felt when they were invited to participate in the HC programme, most replied that they were scared at first but eventually developed trust. When asked whether the information provided in the educational talks was sufficient, necessary and/or reassuring, 73.3% noted that they were reassuring, while 45% deemed them sufficient and 47% believed they were absolutely necessary. We ought to note that 98.8% of respondents rated the programme at seven or more on a scale of ten.
Results of the satisfaction survey given to parents of infants in home care (n=448 families).
| Information received in health education talks | |
| Sufficient | 204 (45.5%) |
| Absolutely necessary | 212 (47.3%) |
| Reassuring | 375 (70.3%) |
| Did you feel supported after attending the talks? | |
| Yes | 436 (97.3%) |
| Did not answer | 12 (2.7%) |
| Have you read the informational brochure? | |
| Yes | 433 (97.3%) |
| Did not answer | 15 (3.3%) |
| How would you rate the contents of the brochure? | |
| Excellent | 187 (41.7%) |
| Very good | 206 (45.9%) |
| Adequate | 33 (7.3%) |
| Did not answer | 22 (4.9%) |
| Home visits fulfilled your expectations | |
| Fully | 337 (75.2%) |
| To a great extent | 93 (20.8%) |
| As expected | 18 (4%) |
| Somewhat | 0 |
| Not at all | 0 |
| Rate the attention received from the home care nurse | |
| Very good | 414 (92.4%) |
| Good | 34 (7.6%) |
| Fair | 0 |
| Poor | 0 |
| Bad | 0 |
| How would you rate the information given by the home care nurse? | |
| Very good | 397 (88.6%) |
| Good | 51 (11.4%) |
| Fair | 0 |
| Poor | 0 |
| Bad | 0 |
| Were you able to ask questions to your satisfaction? | |
| Yes | 445 (99.3%) |
| Did not answer | 3 (0.7%) |
| Rate the information provided at the outpatient clinic | |
| Very good | 357 (79.6%) |
| Good | 81 (18.1%) |
| Fair | 10 (2.2%) |
| Poor | 0 |
| Bad | 0 |
| Rate the attention received in the outpatient clinic | |
| Very good | 388 (86.6%) |
| Good | 52 (11.6%) |
| Fair | 8 (1.8%) |
| Poor | 0 |
| Bad | 0 |
| Have you been able to ask questions to your satisfaction? | |
| Yes | 409 (91.3%) |
| Did not answer | 39 (8.7%) |
| Rate your satisfaction with the programme on a scale from 0 to 10 | |
| Excellent (9–10) | 406 (90.6%) |
| Very good (7–8) | 37 (8.2%) |
| Fair (5–6) | 2 (0.4%) |
| Did not answer | 3 (0.7%) |
From a cost-benefit perspective, the care of a preterm NB in the intermediate care nursery prior to discharge costs 70 euro to staff (nurses and doctors) compared to 11 euro for HC (nurse and taxi fares) per child per day, with savings of approximately 59 euro a day per child in HC.
DiscussionThis study presents the outcomes of the HC programme of our neonatology department for a 13-year period. Salient findings include a progressive decrease in weight at the time of hospital discharge accompanied by an increase in exclusive BF and increased duration of HC, with a steady decrease in the frequency of readmissions and a high level of family satisfaction.
In 1998, Raddish and Merritt wrote that “discharge preparation, and readiness of parents or other caregivers […] represent the art of medicine.”20 Family-centred developmental care has gained prominence in recent years,2 and once they overcome the acute morbidity of the early neonatal period, many preterm NBs undergo a period of intermediate care whose main purpose is monitoring neurodevelopment and weight gain. Combining these two concepts, and having learned of positive experiences in other Spanish neonatal units in Spain,10,11,21 the department of neonatology of our hospital launched the HC programme with the aim of putting infants as early as possible in the full-time care of parents in an environment free of nosocomial infections and restoring balance to the family, in the belief that the mental, emotional and physical health of parents influences the growth, development, health and quality of life of the child.22 Furthermore, in the early days following discharge, HC allows the detection of psychosocial problems in the family such as stress and anxiety,23 which pose a barrier to good care,24 and providing the family with the necessary support to address those problems.
The trends in the social characteristics of families and HC in the twelve-year period show an increase in maternal age, as expected, and also a greater number of previous live births. Housing conditions are better and families seem to be less anxious and worried, despite there being no changes in the predominant ethnicity, educational attainment or occupation of parents. At initiation of HC, infants weigh less and there is a higher rate of exclusive BF, which may account for the smaller comparative weight gain in the first week of HC and the increased duration of the latter, albeit with a decrease in the time spent travelling, and in spite of a decrease in weight at the time of final discharge. However, the overall rates of readmission to hospital and discontinuation of HC have been decreasing, which is indicative of the delivery of quality care. The increased weight gain in the first week post discharge compared to the week preceding discharge from hospital confirms the previous findings of our group.13,16
In these twelve years, programmes have been implemented to improve family-centred developmental care, health education for parents, and NB safety. The health education of parents is one of the pillars of successful HC. In a study conducted in Singapore, Cheo Lian et al.25 demonstrated that the implementation of a health education programme for parents in which nurses were involved as educators, advisors, facilitators and discharge coordinators succeeded in reducing the average length of stay by 23.3 days (from 58.2 days to 34.9 days), with a rate of readmission of 0%. They concluded that communication is the key to the success of the programme.25 Other published studies have shown reductions in the length of stay ranging from four26 to seventeen days,27 and in our study, the reduction was similar to the one found in a previous study conducted in our hospital, of 10.1 days,13 during which had NBs not been in HC, they would have remained hospitalised in a level I nursery with the associated cost of human resources. Home care has been especially recommended for late preterm infants,28 although there are also authors that recommend its universal implementation,29 whereby all infants would receive home visits from a nurse or midwife following early discharge from hospital.
The main limitation of this study is the potential selection bias of having the care nurse and nurse in charge of HC be responsible for deciding which families were admitted to the programme. On the other hand, families have been selected by the same two nurses, the co-authors of this study, during the 12 years, so the admission criteria have probably remained the same.
One of the changes worth highlighting is the considerable increase in breastfeeding rates at discharge, exclusive as well as mixed. Between 2011 and 2014, 91.3% of the infants were being breastfed, a percentage that was slightly superior to that reported by Alexandre et al. (90.3%) in a study conducted on a population of infants born preterm at 30–34 weeks’ gestation.30 Home care helps establish and maintain BF. Preterm birth is a special circumstance in which breastfeeding can be experienced as a way to complete a pregnancy that is often perceived as incomplete and to help the mother grow into her role. Oftentimes, preterm birth is preceded by a difficult pregnancy, and the separation of mother and NB, the need to extract milk and stimulate lactation with a pump, non-nutritive sucking, easy fatigue in the NB, difficulties experienced in the transition from tube-feeding to feeding by suckling, anxiety and fatigue in the mother and others are factors that hinder the establishment of BF. Home care allows mothers to be in charge of feeding their babies 24hours a day.
The user satisfaction survey, filled out by 83.6% of the families invited to participate, assessed their opinion on the entire process of care delivery, and is an important source of information that allows the identification of areas and opportunities for improvement at the different levels of care. Furthermore, HC can save the public health system approximately 60 euro per child per day.
In short, the outcomes of home care for preterm and low-birth-weight NBs have been improving over time, and the programme probably saves between 10 and 11 days of hospitalisation without compromising the quality of care or the satisfaction of families.
Conflict of interestsThe authors have no conflict of interests to declare
Please cite this article as: Figueras Aloy J, Esqué Ruiz MT, Arroyo Gili L, Bella Rodriguez J, Álvarez Miró R, Carbonell Estrany X. Evolución de la atención a domicilio para niños prematuros y de bajo peso de nacimiento desde 2002 hasta 2014. An Pediatr (Barc). 2016;85:134–141.