Several authors question the performance of systematic renal ultrasound after first urinary tract infection (UTI) in young children, given the high sensitivity of prenatal ultrasounds to detect major malformations and the low prevalence of clinical relevant findings. The aims of this study are to evaluate the yield of renal ultrasound performed after the first UTI in patients aged less than 2 years and to analyse potential risk factors (RF) of altered renal ultrasound.
Patients and methodsRetrospective study, including patients aged less than 2 years diagnosed with UTI in the Emergency Department between July 2013 and December 2014. Patients with an underlying nephro-urological pathology, previous UTIs and those without prenatal or post-infection renal ultrasound were excluded. Altered renal ultrasound was defined as the presence of dilated urinary tract or structural abnormalities. Potential RF analysed were: male, age less than 3 months, presence of fever and microorganism other than Escherichia coli. Univariate and multivariate logistic regression were performed.
ResultsA total of 306 patients were included. Altered renal ultrasound was found in 35 cases (11.4%; 95% CI 8.3–15.5): 24 (68.6%) urinary tract dilation, and 11 (31%) structural abnormalities. Among the cases with altered ultrasound, 68.6% were male, 51.4% were younger than 3 months, 74.3% were febrile, and 31.4% were caused by microorganisms other than E. coli, compared to 45% (P=.009), 31.7% (P=.021), 78.2% (P=.597) and 10% (P=.001) of cases with normal ultrasound. In the multivariate analysis, age less than 3 months (OR 2.1; 95% CI 1.0–4.3, P=.05) and microorganism other than E. coli (OR 3.8; 95% CI 1.7–8.7, P=.002) remained as RF.
ConclusionsThe yield of renal ultrasound after the first UTI is low. Its indication should be individualised according to the presence of RF: age less than 3 months and microorganism other than E. coli.
Diversos autores cuestionan la realización sistemática de una ecografía renal en los lactantes con una primera infección del tracto urinario (ITU), dada la alta sensibilidad de las ecografías prenatales para la detección de malformaciones mayores y la baja prevalencia de hallazgos clínicamente significativos. Los objetivos de este trabajo son valorar el rendimiento diagnóstico de la ecografía renal realizada después de la primera ITU en pacientes menores de 2 años y analizar posibles factores de riesgo (FR) de presentar una ecografía renal alterada.
Pacientes y métodosEstudio retrospectivo. Se incluyen los pacientes menores de 2 años diagnosticados de ITU en Urgencias entre julio de 2013 y diciembre de 2014. Se excluyen aquellos con enfermedad nefrourológica, ITU previas y sin ecografía renal prenatal o postinfección. Se considera ecografía renal alterada la presencia de dilatación de las vías urinarias y/o anomalías estructurales. Los posibles FR evaluados son: sexo masculino, edad inferior a 3 meses, fiebre y microorganismo distinto a Escherichia coli. Se realiza estudio univariante y por regresión logística multivariante.
ResultadosSe incluyen 306 pacientes. Presentan ecografía renal alterada 35 (11,4%; IC 95% 8,3-15,5): 24 (68,6%) dilatación de las vías urinarias y 11 (31%) alteraciones estructurales. De las ecografías alteradas, el 68,6% corresponden a varones, el 51,4% a una edad inferior a 3 meses, el 74,3% a ITU febriles y el 31,4% por microorganismo distinto a E. coli, respecto al 45% (p=0,009), el 31,7% (p=0,021), el 78,2% (p=0,597) y el 10% (p=0,001) de las ecografías normales. En el análisis multivariante se mantienen como FR la edad inferior a 3 meses (OR 2,1; IC 95% 1,0-4,3; p=0,05) y un microorganismo distinto a E. coli (OR 3,8; IC 95% 1,7-8,7; p=0,002).
ConclusionesEl rendimiento de la ecografía renal después de la primera ITU es bajo. Se debería individualizar su indicación según la presencia de FR: edad inferior a 3 meses y microorganismo distinto a E. coli.
Urinary tract infections (UTIs) are among the most frequent bacterial diseases in febrile infants.1–5 In incontinent patients, they are usually detected in emergency departments (EDs) due to the need to collect a sterile urine sample for diagnosis. In addition to the diagnosis and the initial course of antibiotherapy, management should include informing the family on the indications for subsequent imaging tests.
Although there are discrepancies between current guidelines and between clinical protocols at different sites regarding the indications for the various imaging tests that can be performed after a first UTI,6 renal ultrasound is included in most due to its broad availability and lack of harmful effects. However, since the introduction of routine prenatal ultrasound examinations, several publications have argued that the most frequent urinary tract malformations are detected before birth.7 With the aim of omitting performance of renal ultrasound after an initial episode of UTI in patients with a normal prenatal ultrasound, Miron et al.8 conducted a prospective study in 250 children aged less than 5 years and assessed the correlation between prenatal and postnatal ultrasound findings, finding a concordance of 96% (95% confidence interval [CI], 93–99). Nevertheless, the role of prenatal ultrasound is still being debated, and the ultrasound after the first UTI is included in many guidelines. Thus, the clinical practice guideline for the management of UTI of the American Academy of Pediatrics9 recommends performance of a renal ultrasound in any febrile child aged less than 2 years with a first episode of UTI. In Spain, both the UTI protocol of the Asociación Española de Pediatría (Spanish Association of Pediatrics)10 and the clinical practice guideline for the management of UTI in the paediatric population developed by the Ministry of Health11 recommend its performance after an initial febrile episode of UTI, with the latter adding the following criteria: incontinent patient without a normal prenatal or postnatal ultrasound, signs of urinary tract dysfunction, abdominal or vesical mass, elevated serum creatinine levels or UTI caused by an organism other than Escherichia coli.
The objectives of our study were to assess the diagnostic yield of renal ultrasound after an initial UTI in patients aged less than 2 years and to analyse potential risk factors for abnormal ultrasound findings.
Materials and methodsStudy designWe conducted a retrospective observational and analytical study in a tertiary women's and children's hospital with 275 paediatric beds that is the referral hospital of a catchment area with a population of 1800000 inhabitants and manages an average of 105000 emergency visits a year.
Study sampleWe reviewed the health records of patients aged less than 2 years managed in the ED between July 2013 and December 2014 discharged from the department with a diagnosis of UTI (code 599.0 of the diagnostic classification of the Sociedad Española de Urgencias de Pediatría [Spanish Society of Paediatric Emergency Medicine]).12 Out of all these cases, we included those with microbiological confirmation of UTI (colony count ≥10000 UFC of a single microorganism in a catheterized urine specimen). We excluded patients with underlying urinary system diseases, with a previous history of UTI or who did not undergo a prenatal or post-UTI ultrasound examination.
Variables under studyWe collected data for the following variables in a form designed for the purpose: age, sex, presence of fever (temperature ≥38°C detected at home or in the ED), microorganism isolated in urine culture, findings of renal ultrasound and indication for other imaging tests in patients with abnormal ultrasound findings. For cases with a normal initial ultrasound, we also analysed the occurrence of new episodes of UTI in the year following diagnosis. To do so, we reviewed the electronic health records of the hospital and the patient's records in the regionwide health record database of the public health system of Catalonia.
We analysed the following variables as potential risk factors for an abnormal ultrasound: male sex, age (less or more than 3 months), presence of fever and causative microorganism other than E. coli.
During the period under study, all patients aged less than 2 years that received a diagnosis of first episode of UTI in the ED routinely underwent a renal ultrasound examination, whether they were admitted to hospital or managed at the outpatient level, and were referred to the outpatient nephrology department. Based on the findings of the ultrasound examination, the nephrologist determined the need for further testing, follow-up and/or treatment. In our hospital, all ultrasound scans are interpreted by paediatric radiologists.
In this study, we defined abnormal renal ultrasound as an ultrasound examination that found evidence of dilatation and/or structural anomalies in the urinary tract, and pathological renal ultrasound as an abnormal ultrasound whose findings led to a change in the management of the patient, either by initiation of antibiotic prophylaxis or referral to surgical assessment.
Statistical analysisWe stored and processed the extracted data in a Microsoft Access database. We tabulated the quantitative and categorical data, and subsequently analysed it with the statistical software SPSS version 20.0. We have described quantitative variables using the mean or median and categorial variables using percentages. We performed tests to analyse the distribution of data (Kolmogorov-Smirnov) and to compare quantitative data (Student t test, Mann–Whitney U test) and qualitative data (chi square test, contingency tables, Fisher exact test). We calculated 95% CIs for proportions using the Wilson score method. Statistical significance was defined as a p-value of less than 0.05. We performed a multivariate logistic regression analysis. The potential predictor variables included in the full model were those corresponding to p-values of less than 0.3 in the univariate analysis. We used the final logistic regression model to recalculate the odds ratios and their 95% CIs.
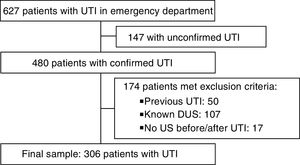
ResultsA total of 627 episodes of UTI were diagnosed during the period under study, with microbiological confirmation in 480 cases. After excluding 174 patients for meeting exclusion criteria, the final sample comprised 306 cases (Fig. 1). Table 1 describes the clinical and epidemiological characteristics of the sample.
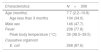
Clinical and epidemiological characteristics of children with a diagnosis of urinary tract infection.
| Characteristics | N=306 |
|---|---|
| Age (months) | 7.7 (2.2–10.8) |
| Age less than 3 months | 104 (34.0) |
| Male sex | 146 (47.7) |
| Fever | 238 (77.8) |
| Peak body temperature (°C) | 39 (38.5–39.5) |
| Causative organism | |
| E. coli | 268 (87.6) |
Categorical variables expressed as absolute and relative frequencies, quantitative variables as median and interquartile range.
The renal ultrasound was abnormal in 35 patients (11.4%; 95% CI, 8.3–15.5): detection of urinary tract dilatation of varying degree in 24 (68.6%) and structural anomalies in 11 (31.4%). The nephrology department decided to expand the evaluation with a voiding cystourethrogram (VCUG) in 26 patients (74.6%), which led to diagnosis of vesicoureteral reflux (VUR) in 7 (26.9%). In 6 cases (2.0%; 95% CI, 0.9–4.2), the renal ultrasound was considered pathological, as it led to prescription of antibiotic prophylaxis. These cases included 4 children with high-grade VUR (iv–v) and 2 with structural anomalies (megaureter). These last 2 patients were also referred for assessment to the Department of Surgery.
In the univariate analysis (Table 2), male sex, age less than 3 months and a causative pathogen other than E. coli were predictors of abnormal ultrasound findings. In the multivariate regression analysis, the variables that remained significant were age less than 3 months, with an OR of 2.1 (1–4.3; P=.05) and a causative pathogen other than E. coli, with an OR of 3.8 (1.7–8.7; P=.002). The 6 patients with a pathological renal ultrasound presented one or both of these risk factors.
Risk factors for abnormal ultrasound findings in children aged less than 2 years with a first episode of urinary tract infection.
| Risk factor | Renal ultrasound | P | |
|---|---|---|---|
| Normal (n=271) | Abnormal (n=35) | ||
| Male sex | 122 (45.0) | 24 (68.6) | 0.009 |
| Age < 3 months | 86 (31.7) | 18 (51.4) | 0.021 |
| Fever | 212 (78.2) | 26 (74.3) | 0.597 |
| Pathogen other than E. coli | 27 (10.0) | 11 (31.4) | 0.001 |
Categorical variables expressed as absolute and relative frequencies.
Of the 271 patients with a normal renal ultrasound, 26 (9.6%) had a new episode of UTI in the first year of follow-up. A new renal ultrasound was performed in 7 of them, and was abnormal in 1 case (mild ectasia). Fifteen of these patients were evaluated with a VCUG, which detected a low-grade VUR in 3.
DiscussionOur study confirmed the low yield of renal ultrasound following a first UTI, as the test was only relevant in patients with risk factors. Several recent studies have found similar results concerning the efficacy of renal ultrasound in patients with UTI as a tool for screening for urinary system anomalies, with a low sensitivity, specificity and predictive value compared to other diagnostic techniques (VCUG, dimercaptosuccinic acid [DMSA] renal scan).13,14 In 2014, Zamir et al. published a study in 255 patients with a first UTI; the renal ultrasound was abnormal in 33, and the management was not changed as a result of the findings in any of the patients.15 The results of a study by Nelson et al. were similar, and the authors concluded that renal ultrasound is a poor tool for diagnosis of urinary system anomalies after analysing a sample of 2259 patients and finding a prevalence of clinically significant anomalies of 2%.16 These results agree with those of our study, where the renal ultrasound after a first UTI only led to changes in management in 6 patients (2% of cases), all of them aged less than 3 months and/or with a UTI caused by a pathogen other than E. coli. The latter finding is consistent with the findings of a previous study conducted in the same hospital17 and with the indications of the clinical practice guideline of the Spanish National Health System of 2011,11 which specifically recommends performance of a renal ultrasound in patients with UTI caused by a microorganism other than E. coli on account of the existing evidence on the high prevalence of urinary system abnormalities in these patients. On the other hand, the higher frequency of abnormal findings in the follow-up ultrasound in younger children, which is statistically significant in infants aged less than 3 months, could be partly explained to the higher prevalence of VUR in younger children, which decreases gradually with age (with a rate of spontaneous resolution of 10% to 15% per year of growth).18
Multiple studies have demonstrated that patients with diseases of the urinary system are at higher risk of urinary tract infection; previous calculations19 have estimated the positive predictive value of recurrent UTI for predicting high-grade VUR at 55%, whereas children with a single episode of UTI are at lower risk of associated malformations. Based on this evidence, the latest update of the National Institute for Health and Care Excellence (NICE) guideline on the management of UTIs in patients aged less than 16 years20 recommends against routine performance of ultrasound after a first uncomplicated UTI in children aged more than 6 months, reserving this diagnostic tool for cases of recurrent UTI, atypical UTI or patients aged less than 6 months. The low frequency of recurrence of UTI within a year of diagnosis in patients with a normal ultrasound after a first episode of UTI found in our study supports this recommendation, and suggests that it may be more useful to perform a VCUG after a second episode of UTI rather than a second ultrasound in patients without any of the 2 risk factors mentioned above.
The main limitations of our study are those intrinsic to its retrospective design. On the other hand, while the regionwide electronic health records allowed us to track the outpatient management of the patients, we had to exclude 17 patients due to the absence of records for a prenatal or post-UTI ultrasound; it is possible that these patients were managed in private facilities and that there were radiologic findings unknown to us in these cases. However, this subset of patients is very small, and therefore we consider that it did not have a relevant impact on the results. For the same reason, it is also possible that some of the patients with normal ultrasounds had subsequent episodes of UTI during the follow-up that we were unable to detect.
To conclude, the overall yield of renal ultrasound after a first episode of UTI in children aged less than 2 years is low, as its findings have little impact on the subsequent management in most cases, which suggests that the decision to perform a renal ultrasound should be made on a case-to-case basis based on the presence of risk factors: age less than 3 months or causative microorganism other than E. coli.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Faura Morros A, Cuaresma González A, Hernández-Bou S, Trenchs Sainz de la Maza V, Camacho Diaz JA, Luaces Cubells C. Rentabilidad diagnóstica de la ecografía renal tras la primera infección de orina en los lactantes. An Pediatr (Barc). 2019;90:232–236.
☆☆ Previous presentations: This study was presented as an oral communication at the XXI Annual Meeting of the Sociedad Española de Urgencias Pediátricas (2016; Valencia, Spain) and the XXII Annual Meeting of the Societat Catalana de Pediatría (2016; Tortosa, Spain).