On March 14, 2020, the Spanish government, in response to the COVID-19 pandemic, established strict measures to restrict freedom of movement.1 The strategy implemented by the authorities could be utilised as a natural experiment to assess the impact on the wellbeing of pregnant women of measures such as home confinement, the widespread use of masks and other forms of social distancing. Recent studies suggest that the incidence of preterm birth has decreased during the strictest months of the lockdown.2 Even communication channels that are not purely scientific have reported the subjective perception of neonatologists in different parts of the world that there has been a decrease in preterm births.3 Since data for Spain had not yet been published, we decided to review what had happened in the region of Valencia, Spain, and see if our findings corroborated reports in other geographical areas.
By reviewing newborn metabolic screening records, we collected data on the preterm births that took place in the Valencian Community during the state of alert between March 14 and June 21, 2020 and compared them with the births of the 5 previous years in the same time period. We classified preterm births based on the duration of gestation into the following groups: mild/late preterm (32-36 weeks), moderate preterm (28–31 weeks) and extremely preterm (24–27 weeks). To perform the comparison, we used the z-test for proportions with continuity correction and calculated odds ratios with their 95% confidence intervals using the software R, version 4.0.2. To analyse differences in preterm birth trends in the years under study, we used joinpoint linear regression (Joinpoint Regression Program, version 4.9.0.0, March 2021; Statistical Methodology and Applications Branch, Surveillance Research Program, National Cancer Institute; accessed July 5, 2021). The study was approved by the Bioethics Research Committee and adhered to the STROBE guidelines for the reporting of observational studies epidemiology.
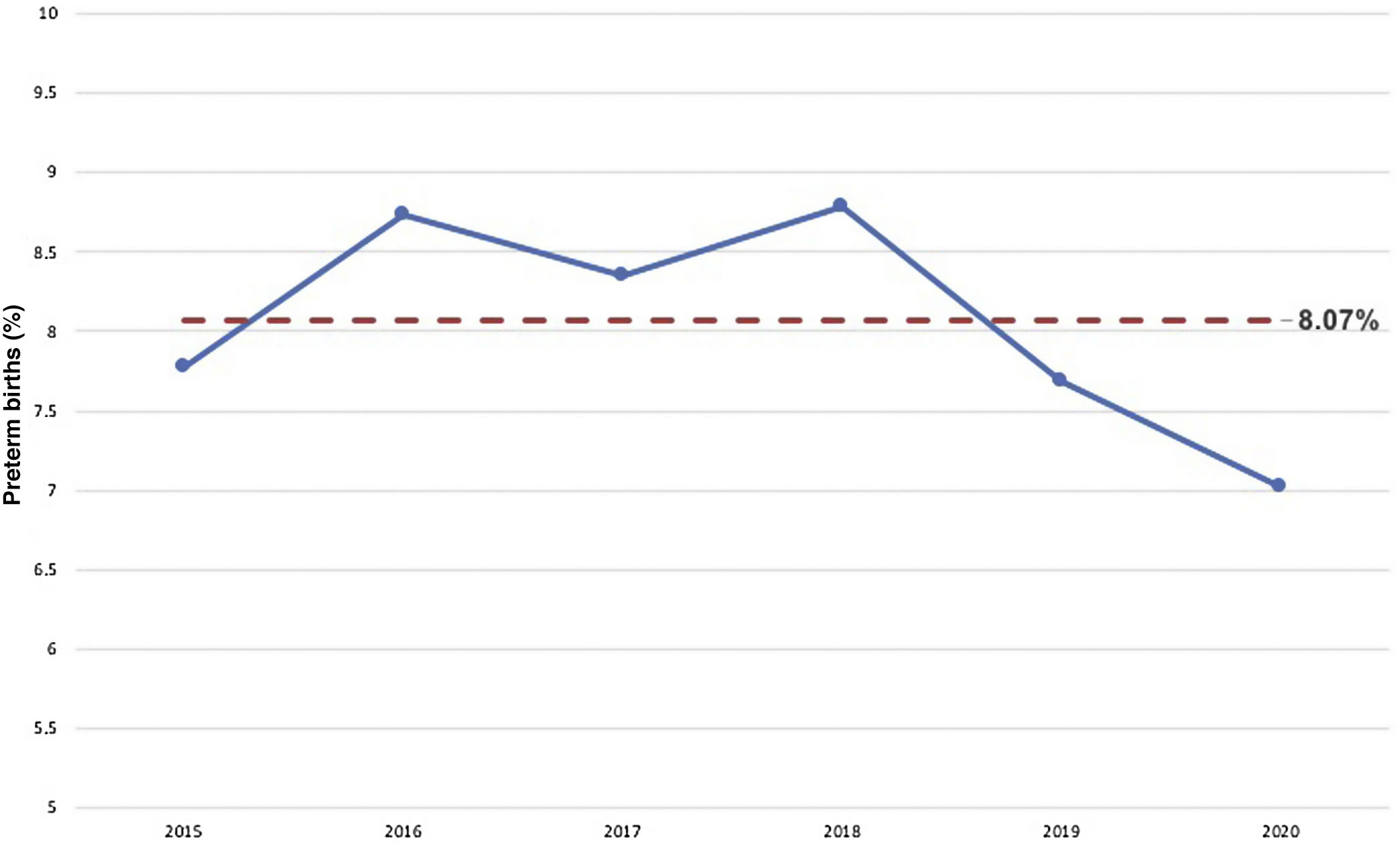
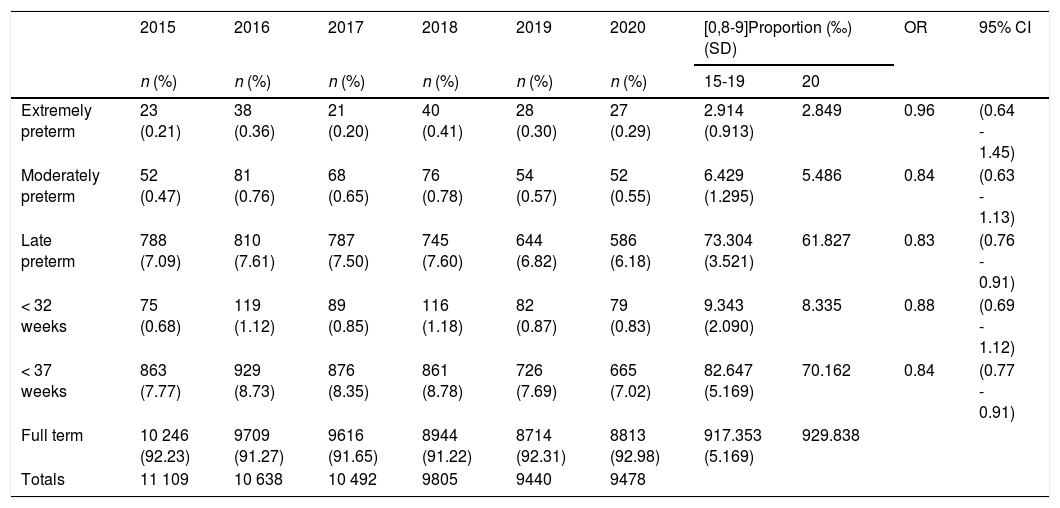
We counted 60 962 births, of which 4920 were preterm (8.07%). The proportion of preterm births during the state of alert of 2020 was significantly lower compared to the proportions observed in the same period of the 5 previous years (OR, 0.84; 95% CI, 0.77–0.91; P < 0.001) (Fig. 1). We also found a significant decrease in the proportion of mild/late preterm births (OR, 0.83; 95% CI, 0.76–0.91; P < 0.001). We did not find significant differences in the proportions of moderate and extremely preterm births (Table 1). The joinpoint analysis evinced a decreasing trend in the percentage of preterm births between 2015 and 2020, although it was not statistically significant and the differences were relatively small. However, there was a significant change in trend when we fit the model with a single joint point, shifting from an increasing trend in the 2015–2018 period with an annual percent change of 3% to a decreasing trend in the 2018–2020 period with an annual percent change of –10.9%, a relevant finding the cause of which would be worth investigating.
Distribution of births in the period under study (March 14–June 21, 2015–2020).
| 2015 | 2016 | 2017 | 2018 | 2019 | 2020 | [0,8-9]Proportion (‰) (SD) | OR | 95% CI | ||
|---|---|---|---|---|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | 15-19 | 20 | |||
| Extremely preterm | 23 (0.21) | 38 (0.36) | 21 (0.20) | 40 (0.41) | 28 (0.30) | 27 (0.29) | 2.914 (0.913) | 2.849 | 0.96 | (0.64 - 1.45) |
| Moderately preterm | 52 (0.47) | 81 (0.76) | 68 (0.65) | 76 (0.78) | 54 (0.57) | 52 (0.55) | 6.429 (1.295) | 5.486 | 0.84 | (0.63 - 1.13) |
| Late preterm | 788 (7.09) | 810 (7.61) | 787 (7.50) | 745 (7.60) | 644 (6.82) | 586 (6.18) | 73.304 (3.521) | 61.827 | 0.83 | (0.76 - 0.91) |
| < 32 weeks | 75 (0.68) | 119 (1.12) | 89 (0.85) | 116 (1.18) | 82 (0.87) | 79 (0.83) | 9.343 (2.090) | 8.335 | 0.88 | (0.69 - 1.12) |
| < 37 weeks | 863 (7.77) | 929 (8.73) | 876 (8.35) | 861 (8.78) | 726 (7.69) | 665 (7.02) | 82.647 (5.169) | 70.162 | 0.84 | (0.77 - 0.91) |
| Full term | 10 246 (92.23) | 9709 (91.27) | 9616 (91.65) | 8944 (91.22) | 8714 (92.31) | 8813 (92.98) | 917.353 (5.169) | 929.838 | ||
| Totals | 11 109 | 10 638 | 10 492 | 9805 | 9440 | 9478 | ||||
CI, confidence interval; OR, odds ratio; SD, standard deviation.
Preventive measures against COVID-19, such as social distancing, school and nursery closures or hand hygiene may have decreased contact with pathogens and had an impact on asymptomatic maternal infection, a known trigger of preterm birth.4 However, other factors are also involved in preterm birth: population characteristics, reproductive health policy, infertility treatment or the indications for termination of pregnancy. In 2019, the Euro-Peristat project5 released the European perinatal health report 2015 with data on preterm births for 31 European countries that evinced the importance of population characteristics. In countries with a comparable level of development, the frequency of preterm birth varied significantly, ranging from 5% to 12% of the total births. The data illustrate the marked variation that exists between European countries in relevant risk factors such as twin gestation, maternal age, pregestational body mass index, smoking during pregnancy and the proportion of immigrants in the population. For instance, the proportion of mothers aged 35 years or older ranged from 14% and 37.3% and the prevalence of smoking from 3.6% to 18.3%. We ought to highlight that when it came to these factors used as examples, the highest frequencies corresponded to Spain and the Valencian Community, respectively. The main limitation of our study is the retrospective collection of the data, which could not be avoided in the event of an unexpected situation like the SARS-CoV-2 pandemic. The results should be generalised with caution, as the analysis was limited to regional data and did not take into account the delivery of prenatal care during the lockdown or the type of delivery/termination of pregnancy. A recent study by Carrasco et al detected an increase in the proportion of caesarean deliveries and of preterm births (36.2% and 20.6%, respectively) in a cohort of pregnant women infected by SARS-CoV-2 during the first wave of the pandemic in Spain.6 Another aspect that may need to be considered is the impact of the differences in the cumulative incidence of SARS-CoV-2 infection between autonomous communities in the same period. In conclusion, our observations in our region suggest that there is an association between environmental factors and the frequency of preterm birth. This is the first study published on the subject in Spain, although there are still gaps in the evidence—pending confirmation of the findings in other autonomous communities and in Spain overall, or data on the actual impact of population characteristics—that could be addressed in future research.
Please cite this article as: Molina-Merino A, Martínez-Rodríguez L, Cubells-García E, Hortelano-Platero V, Estañ-Capell J. Efecto del confinamiento sobre los nacimientos pretérmino en la Comunidad Valenciana. An Pediatr (Barc). 2021;95:379–381.