Hepatopulmonary fusion (HPF) is a rare and highly fatal congenital malformation found in right-sided congenital diaphragmatic defects. It is characterized by the fibrovascular fusion of the liver and lung that is commonly detected during the surgical repair of the defect.1 It affects approximately three out of 1000 patients with congenital diaphragmatic hernia.2
The cornerstone of treatment is surgical repair, and the operative approach depends on the degree of fusion and vascular compromise.3 The prognosis is poor, and most patients die during the perioperative period from complications such as respiratory failure, bleeding, heart failure, vena cava thrombosis and pulmonary hypertension.1,4
Fever than 50 cases have been reported worldwide through year 2020.5 Due to the low incidence of this disease and the selected operative approach, we considered the publication of this case relevant.
We present the case of a male patient born at 37 weeks of gestation with a diagnosis of right-sided diaphragmatic hernia. At 48 h post birth, surgical repair was attempted via thoracotomy, with visualization of a severely hypoplastic right lung that was completely fused to the Glisson capsule over the dome of the right lobe of the liver, particularly segments V, VII and VIII. The separation of the fused tissue proved impossible and was complicated by bleeding, which was controlled with 4−0 polypropylene sutures.
Given the critical and unstable condition of the patient, the small posterolateral remnant of the diaphragm was fixed to the ribcage as a palliative measure until a second intervention could be performed under better conditions. The reintervention, seven days later, evinced the presence of an extensive diaphragmatic defect with protrusion of the liver and a severely hypoplastic lung that were densely adherent, with enmeshment of liver and lung parenchyma and blood vessels and no identifiable separation plane. The pulmonary artery was very thin, the inferior vena cava could not be found, and the hepatic veins drained directly to the right atrium, as observed later in the CT angiogram (Fig. 1).
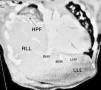
The chosen approach was closure of the defect around the liver, without attempting to separate the fused tissues. The remnant of the diaphragm was stitched to the capsule with horizontal mattress sutures (4−0 polypropylene) and reinforced with polytetrafluoroethylene patches (GORE-TEX®), forming an effective seal to prevent herniation of the bowel loops. After the surgery, the dome of the liver was at the level of the IV intercostal space, as in diaphragmatic eventration (Fig. 2).
During the postoperative period, the patient required high-frequency ventilation, from which he was gradually weaned off, and had severe pulmonary hypertension managed with sildenafil, without use of nitric oxide.
He was discharged home with minimal supplemental oxygen requirements, and weaned off it gradually, while pulmonary hypertension remained mild to moderate at 8 months of follow-up. His respiratory mechanics continue to be good, even though the liver remains at the level of the fourth intercostal space.
Hepatopulmonary fusion is also associated with bronchobiliary fistula and anomalous right-sided pulmonary venous drainage to the retrohepatic inferior vena cava, as occurs in scimitar syndrome.6 In more than 50% of cases, it is associated with cardiac, vascular, chromosomal or pulmonary anomalies.6
The goal of treatment is to reduce the herniated abdominal contents, separate the fused lung and liver and achieve closure of the defect, although several reports highlight the considerable difficulty of achieving it.6
Some of the possible surgical repair options are complete separation, partial separation, repair of the defect around the fused organs without their separation, implantation of prosthetic material or partial liver and lung resection.2,4,5 In most cases, complete separation is impossible due to the complexity of the fusion, and partial separation, with or without use of mesh, or plication of the hernia sac around the fused organs may be a safer approach.1,6
If the fusion of liver and lung is primarily fibrovascular, that is, involving connective tissues and blood vessels, complete separation may be feasible. When it involves the parenchyma of both organs, separation without causing fatal hemorrhage is practically impossible.6
In short, this is an extremely rare anomaly with a very poor prognosis even with surgical management. Complete separation of the liver and lung is possible in certain cases, but it is not always feasible or advisable. Closure of the defect around the unseparated fusion may be a valid option in the case of unfavorable anatomy or in very critically ill patients.