We are writing in relation to the article published by Piñeiro Pérez et al., titled “Reluctance of parents to immunize their children with nirsevimab”,1 which we read with considerable interest, as it is the first article to address the reasons for choosing not to immunize children with this novel monoclonal antibody in a country like Spain, where it is administered free of charge.
Our Working Group on the Impact of Universal Prophylaxis for Respiratory Syncytial Virus (RSV) in Spain has evaluated the enormous decrease achieved by the administration of nirsevimab in the number of episodes of acute bronchiolitis managed in pediatric emergency departments (PEDs) in the 2023–2024 and 2024–2025 seasons.2,3
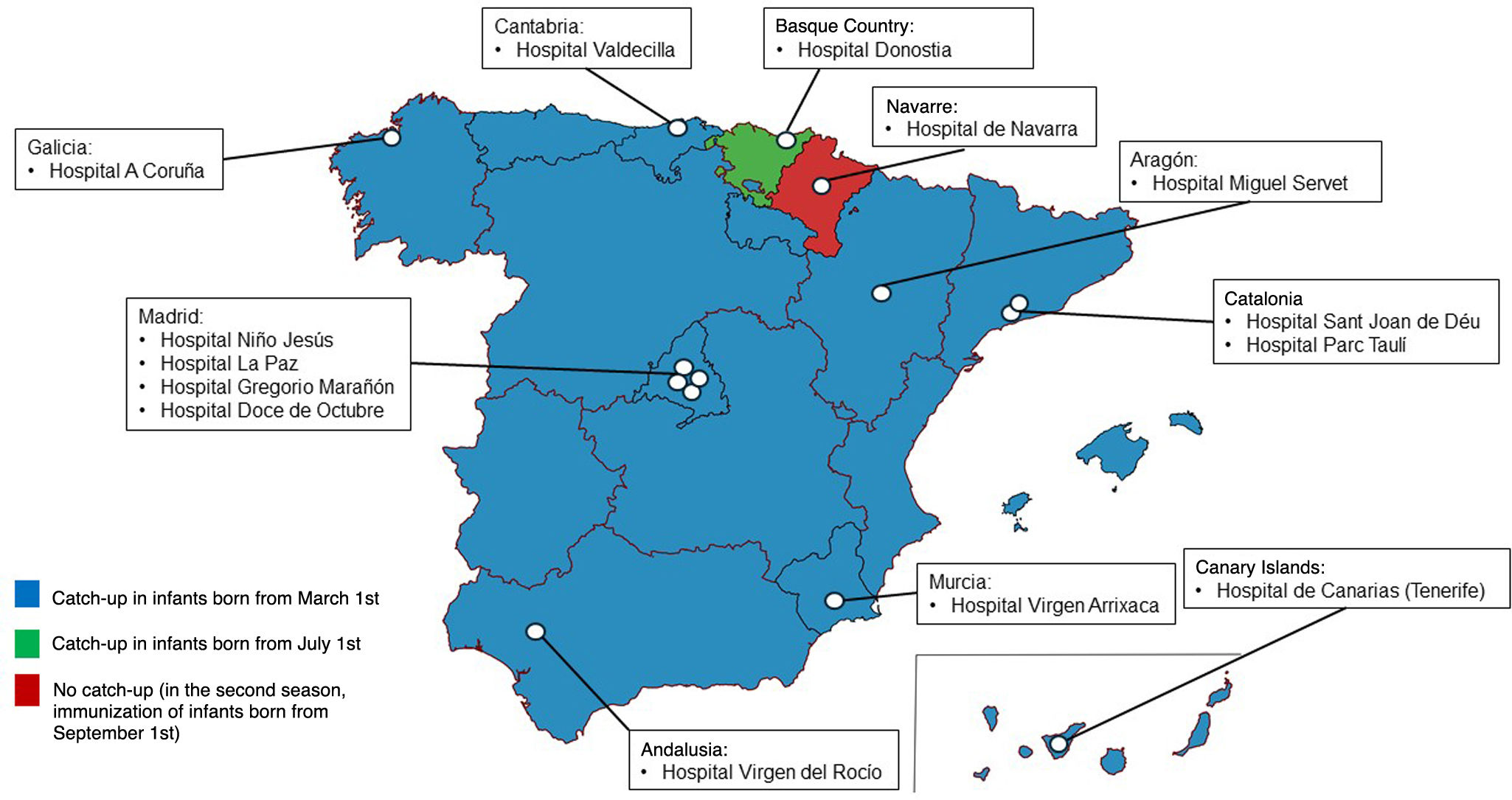
We established a register in which we documented the reason for not having immunized infants that were admitted with acute bronchiolitis and had not been immunized as indicated by the recommendations issued by the Ministry of Health of Spain.4 Our findings cover 14 PEDs in nine autonomous communities (ACs) in Spain, including two hospitals in ACs that have implemented more restrictive strategies for capturing infants outside the RSV season or catch-up immunization (Fig. 1).
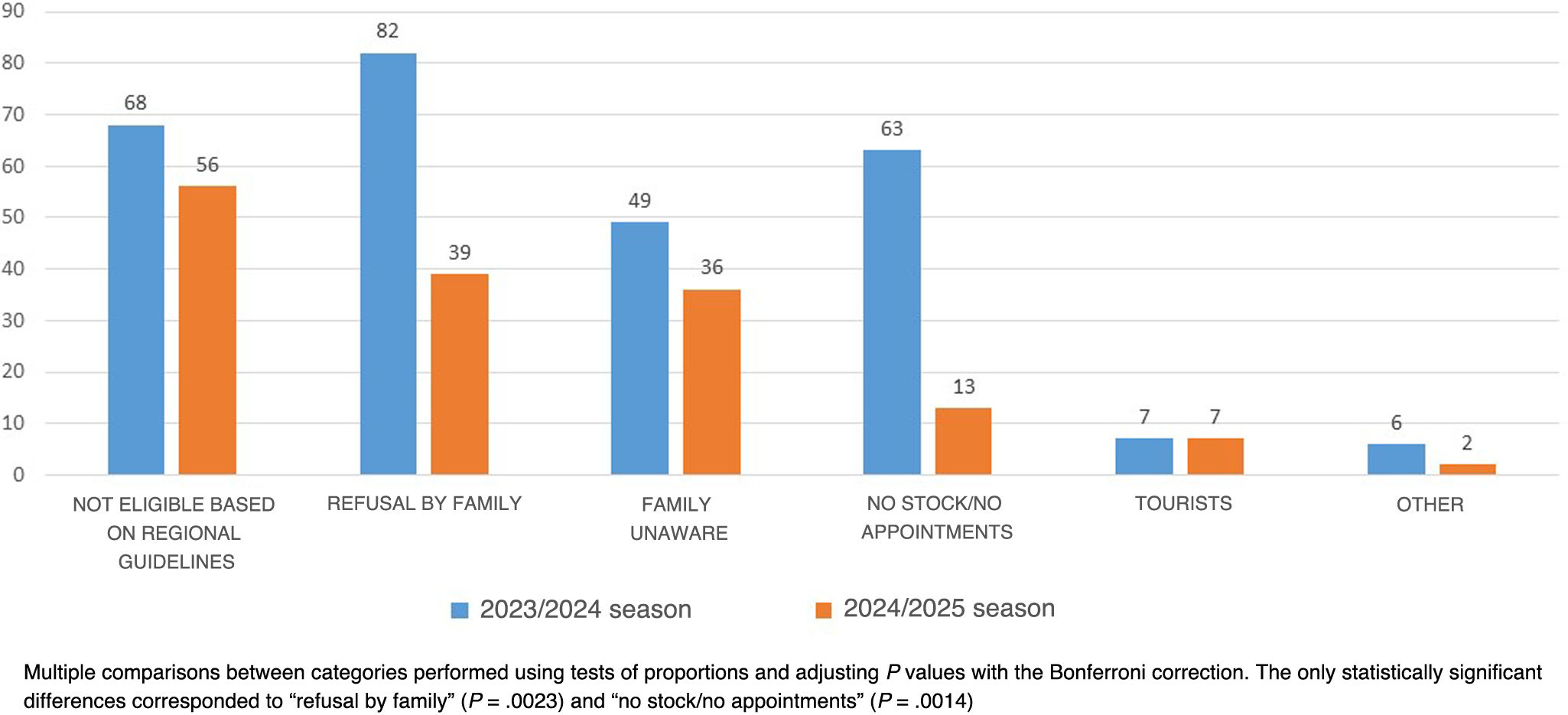
During the 2023–2024 season, participating hospitals admitted 340 unimmunized infants with acute bronchiolitis, and the reason for not having immunized them was recorded in 275 cases (80.9%). In the 2024–2025 season, they admitted 185 infants, with the reason for not immunizing documented in 153 (82.7%) (Fig. 2).
In the 2024–2025 season, nonadherence to the recommendations of the Ministry of Health by regional health care administrations at the AC level became the most frequent cause of not immunizing. Conversely, family refusal decreased significantly, probably due to the excellent effectiveness and safety profile of nirsevimab in the preceding season. These findings, which were disseminated extensively among health care professionals and by the mass-media, may have partly overcome the reluctance reported by Piñeiro Pérez et al.1 A lack of awareness of the immunization campaign among families continued to be the third leading cause and highlighted the differences in immunization coverage between infants born during the RSV season, in whom providing information and immunization was easier, compared to infants in the catch-up group, which may not be reached by the campaign.4 Last of all, it seemed that the logistic problems involving nirsevimab shortages and appointment unavailability, which were to be expected to a degree in the first season, had been solved for the most part by the second season.2
In spite of the limitations intrinsic to its retrospective design, our study contributes additional information on the reasons for not immunizing infants in Spain and the temporal trends in these reasons observed in the second season of nirsevimab administration.
Our findings prompt reflection on the strategies implemented in the Basque Country and Navarre, which did not adhere to the recommendations of the Ministry of Health. In addition, we believe that educational campaigns should be implemented to not only address the reasons for family refusal, but also to underscore the importance of immunizing all eligible patients in adherence with current recommendations.
FundingThe authors declare not having received any form of funding to write this letter to the editor.
Dr David Andina has received fees from Sanofi for being featured as an instructor in educational. The authors declare that they have no competing financial interests or personal relationships that could have influenced the work presented in this article.