Shigella is a gram-negative non-capsulated non-motile bacillus of the Enterobacteriaceae family. It causes bacillary dysentery and it is transmitted by the faecal-oral route. It has a low infective dose that facilitates its dissemination.1 The genus comprises 4 species: Shigella dysenteriae, Shigella flexneri, Shigella boydii y Shigella sonnei. The latter accounts for up to 80% de of infections in Europe and North America and is considered an emergent pathogen.1 Most paediatric infections are asymptomatic or manifest with mild symptoms. However, it can also cause bacteraemia, encephalopathy, intestinal perforation and peritonitis.1 Antibiotherapy is recommended to control outbreaks, in patients who attend a child care centre or live in residential facilities and to reduce the duration of diarrhoea in cases of complicated dysentery.2 In high-income countries, these infections are associated with sexual transmission in men who have sex with men (MSM).1 In 2022, the European Centre for Disease Prevention and Contro (ECDC) warned of an increase in extensively-drug resistant S sonnei infections in several European countries, chiefly in MSM.3 In Spain, previous studies had reported the emergence of infections by multidrug-resistant (MDR) S sonnei associated with transmission among MSM.4
We present two cases of infection by MDR S sonnei in children who were, to our knowledge, the first paediatric cases with an MDR profile reported in Spain.Case 1 Girl aged 4 years who presented with a typical febrile seizure, fever of 39.4 °C, vomiting and abundant watery diarrhoea. A blood panel was ordered that revealed elevation of markers of infection (C-reactive protein [CRP], 168 mg/L; procalcitonin [PCT], 7.53 ng/mL), prompting initiation of treatment with cefotaxime at a dose of 200 mg/kg/day, which the patient received for 3 days. The blood culture was negative. Shigella sonnei was isolated from the stool culture, and the isolate was found to be resistant to ampicillin, cefotaxime, amoxicillin, trimethoprim-sulfamethoxazole, azithromycin and levofloxacin, and sensitive to amoxicillin-clavulanic acid, piperacillin-tazobactam, tigecycline and carbapenems. Since the patient exhibited clinical improvement, she was discharged after 4 days, and completed one week of treatment with oral amoxicillin-clavulanic acid. Girl aged 4 years managed in the same primary care centre as the previous case. She presented with fever of up to 39.5 °C of 24 h’ duration and watery and abandoned diarrhoea with onset one week prior. There was an outbreak of gastroenteritis in her school. After ensuring that the patient was clinically stable, she was discharged home, and a stool culture ordered. Shigella sonnei was isolated from culture, with the same antimicrobial susceptibility profile as the previous case. In this case, the patient had a favourable outcome with resolution of symptoms at the time of follow-up at the primary care centre, Once the results of the stool culture were available, and she did not receive any antibiotic treatment.
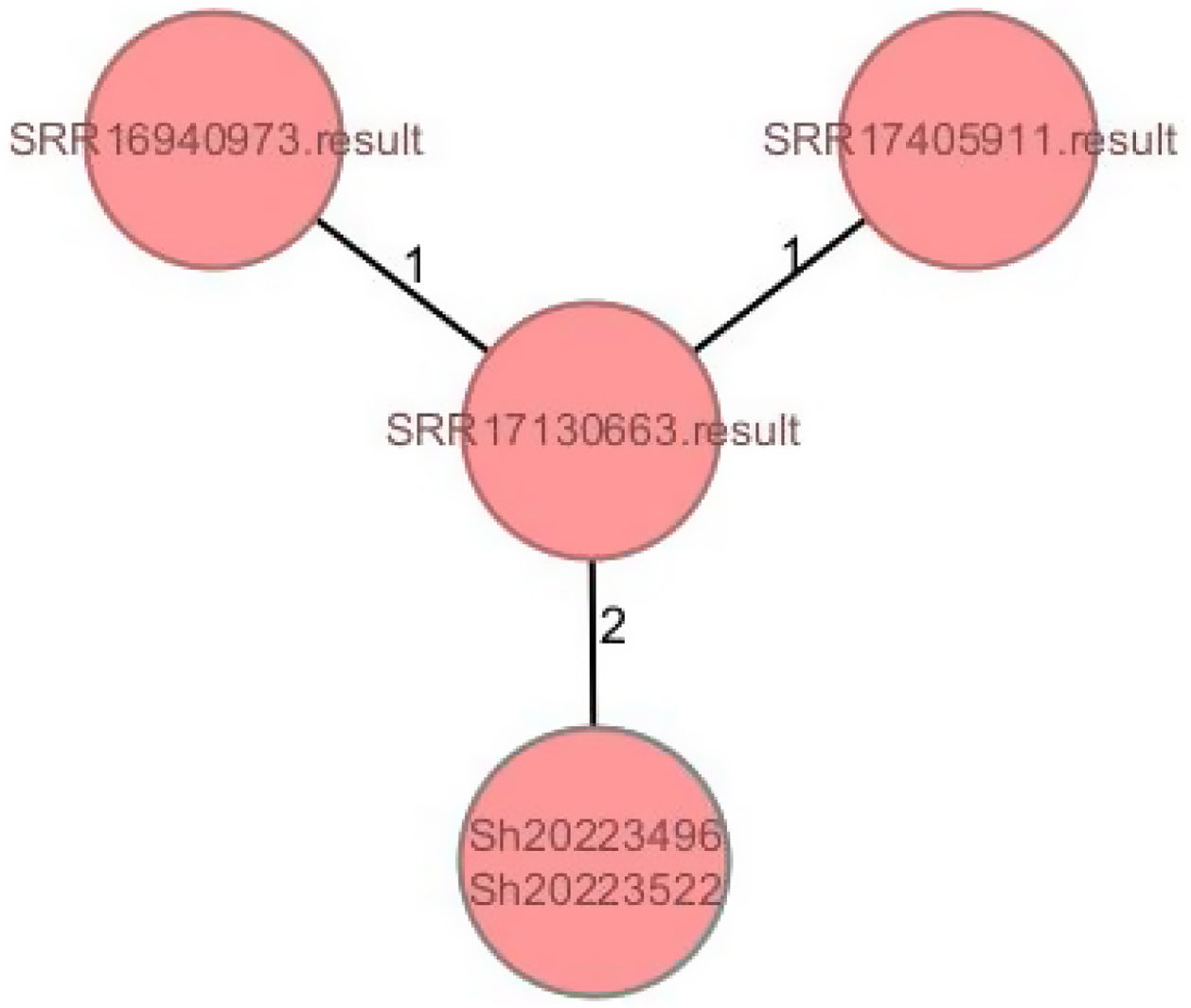
Both isolates of MDR S sonnei were sequenced and analysed by means of cgMLST (core/whole genome multilocus sequence typing). The comparison of the 2 isolates with the reference genomes available through the ECDC showed that these cases could be included in the same genetic cluster with a maximum difference of 3 alleles, and the presence of the same IncFII plasmid carrying the blaCTX-M-27 gene, which evinced the geographical spread of this strain (Fig. 1).
Whole genome analysis of the two clinical isolates of Shigella sonnei. Comparison with three reference genomes: SRR16940973, SRR17405911 andSRR1713130663, and genomic analysis of antimicrobial resistance genotype. Genotyping was performed by high-throughput whole-genome sequencing with pair-end reads using the commercial kit NexteraTM DNA Flex Library Preparation Kit and the NextSeq sequencing system (Illumina Inc, San Diego, CA, USA). The DNA was extracted with the Maxwell RSC automated platform (Promega, Madison, Wisconsin, USA). The obtained sequences were assembled with the software tools SPAdesversion 3.15.4 and PROKKA version 1.12. Clustering was carried out with the software Ridom SeqSphere + version 6.0.2 using the scheme defined for Escherichia coli (2528 loci) and establishing a threshold of 10 alleles for the detection of clusters.
The number of episodes of enteritis caused by MDR pathogens is increasing in Spain.4 A retrospective and descriptive study carried out our hospital of all the cases of shigellosis reported between January 2016 and April 20224 only identified two other paediatric cases with isolation of Shigella species, both in male patients with diarrhoea containing blood and mucus in 2019, and both involving strains that were not MDR. The first case corresponded to a boy from Angola aged 5 years, and the Shigella strain was only found to be resistant to ampicillin and trimethoprim-sulfamethoxazole and was sensitive to cefotaxime and ciprofloxacin, as well as all other tested antibiotics. The second, a boy aged 8 years with infection by a multisensitive Shigella species that was only resistant to ampicillin. However, the 2 more recent cases that we present in this article, detected in November 2022, exhibited a MDR profile.
Due to the increasing prevalence of resistance to trimethoprim-sulfamethoxazole, ampicillin, sulphonamides and tetracyclines, the World Health Organization (WHO) recommends fluoroquinolones as first-line treatment for patients of any age with shigellosis.5 The increase of MDR in Shigella spp, mainly to third-generation cephalosporins, azithromycin and fluoroquinolones, as observed in the cases presented here, is a concern in developed countries.5
The ECDC underscores the importance of early detection and the prevention of the sexual transmission of Shigella. However, given the nature of this infection and the magnitude of the problem in Europe, we need to improve our knowledge of the epidemiology of Shigella infections in children. Many outbreaks of shigellosis take place in nurseries and schools.6 Young children are most vulnerable to the potential complications of Shigella infections.2 Empirical treatments for acute enteritis by enteroinvasive strains could not be effective, which poses a particularly serious risk to immunocompromised patients. All of this poses a threat to public health, so measures need to be developed for the early detection of infection and the prevention of transmission that contemplate the paediatric population.