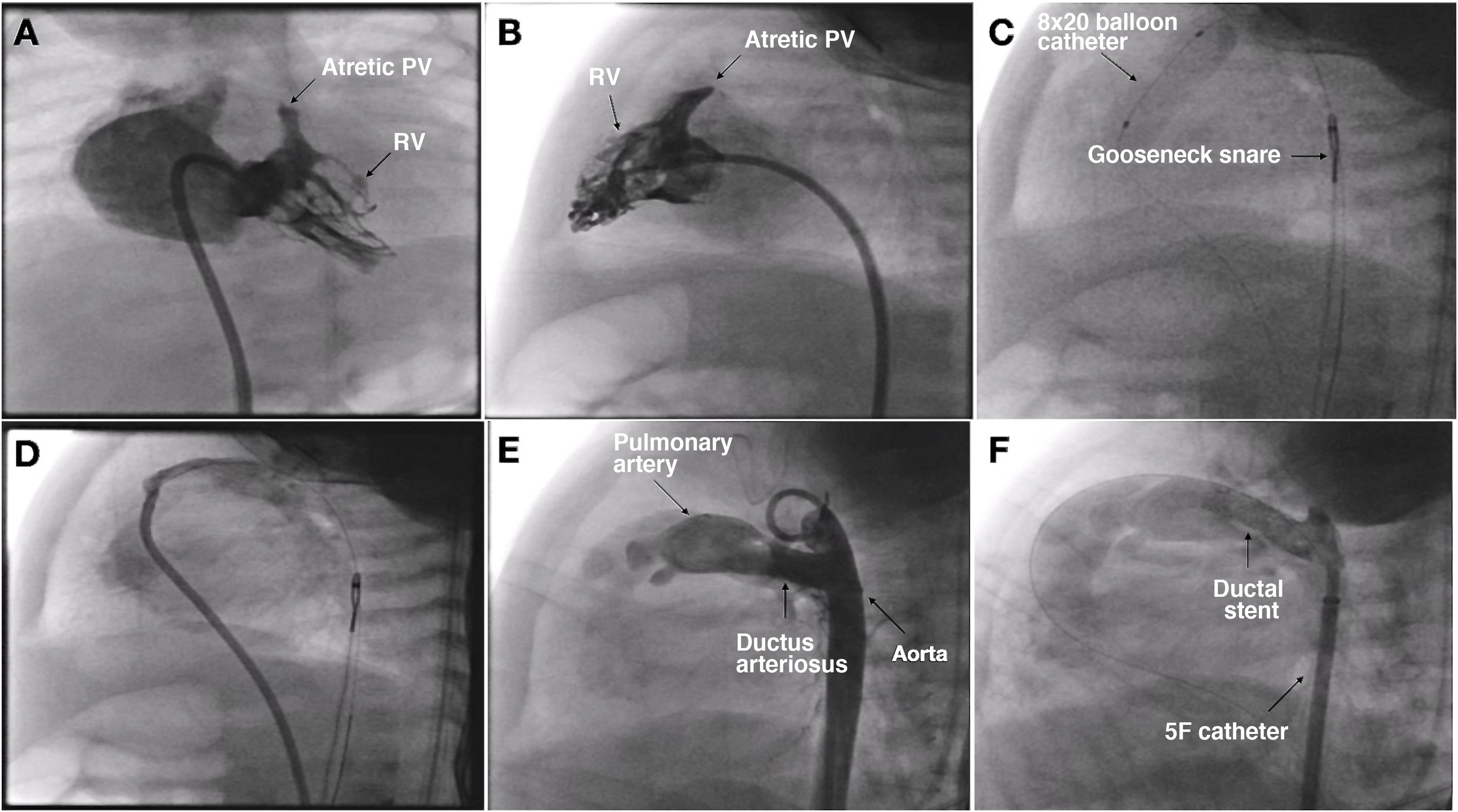
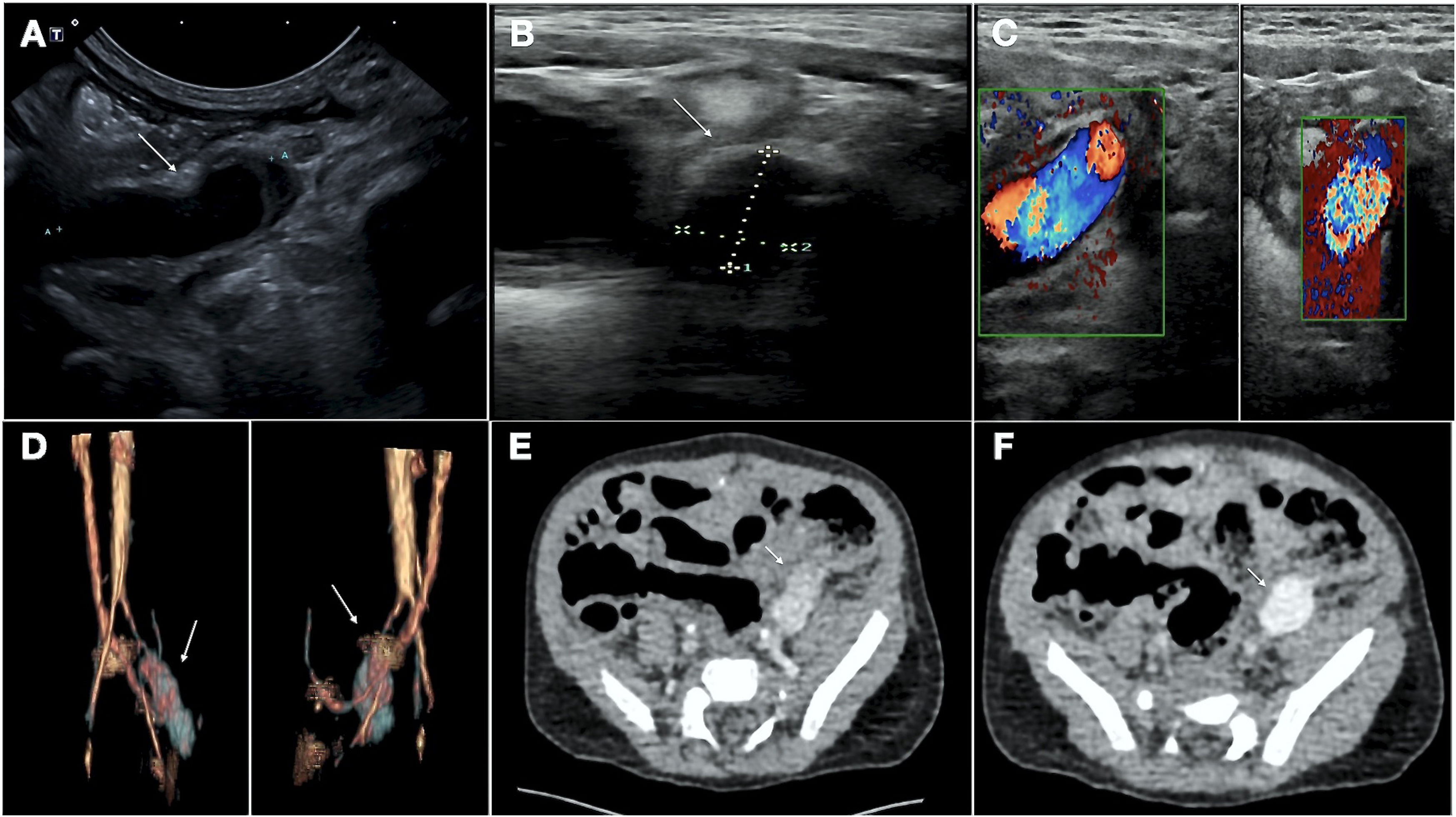
We present the case of a boy aged 15 months with a prenatal diagnosis of pulmonary atresia with intact ventricular septum who underwent pulmonary valve perforation and balloon valvuloplasty with an 8 mm balloon at 9 days post birth (Fig. 1A–D; Appendix B, videos 1–3). At 30 days, due to persistent desaturation, the decision was made to perform percutaneous ductal stenting, since this was less invasive compared to other techniques used to increase pulmonary flow. The procedure, guided by ultrasound, consisted in the delivery, via the left femoral artery and using a 5 F introducer, of a drug-eluting stent (Onyx Frontier, Medtronic, USA) measuring 4.5 × 12 mm to the ductus arteriosus (Fig. 1E and F; Appendix B, videos 4 and 5). Five days after the procedure, the patient experienced vomiting, and the abdominal ultrasound scan used for initial assessment revealed a mass in the left groin, with subsequent Doppler and angio-CT scans allowing visualization of a pseudoaneurysm at the level of the left common iliac artery (Fig. 2A–F).
(A) and (B) Right ventriculogram, anteroposterior and lateral views showing pulmonary valve atresia (7.5 mm ring). C) Pulmonary valvuloplasty performed with a TYSHAK MINI® (NuMED) 8 × 20 mm balloon catheter advanced on a 0.0014 coronary guidewire, which traversed the ductus arteriosus to the aorta supported by a gooseneck snare. (D) Angiographic confirmation of preserved pulmonary flow after valvuloplasty. (E) Lateral aortogram showing patent ductus arteriosus and filling of right chambers. (F) Aortogram following stent placement.
PV, pulmonary valve; RV, right ventricle.
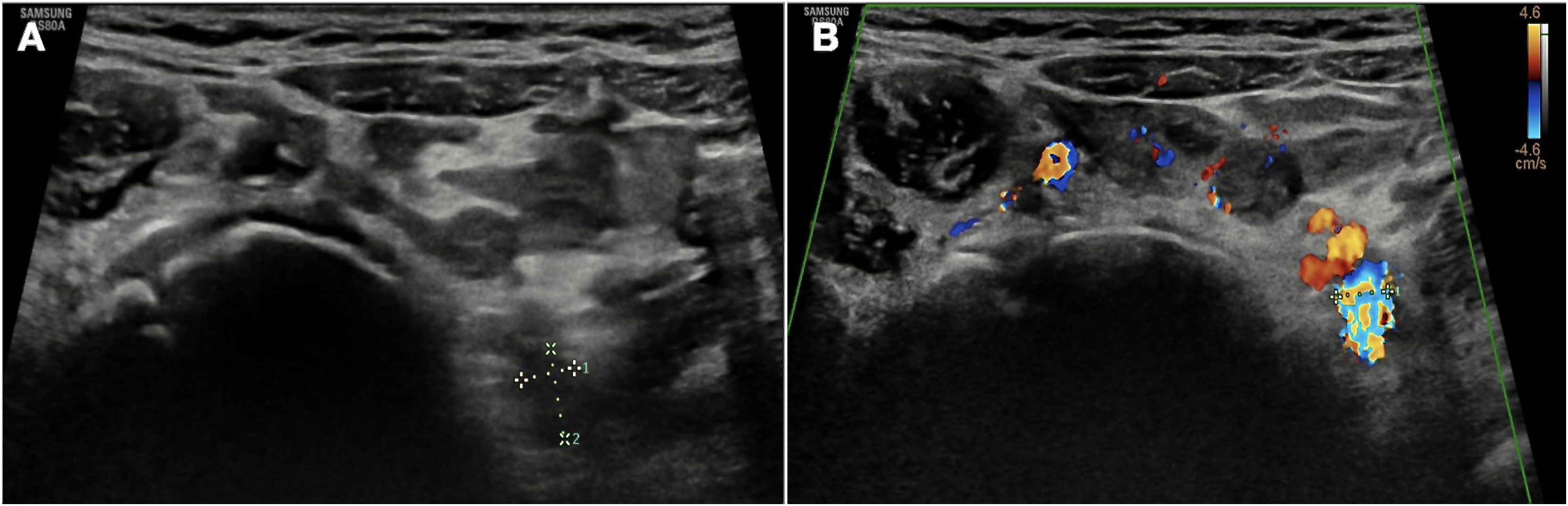
Due to the risks involved in surgical intervention and the scarcity of the evidence on endovascular treatment in newborns, currently limited to isolated case reports,1,2 the patient was managed conservatively with close clinical and radiological monitoring. Fifteen months later, the patient remains asymptomatic and has started to stand and walk without any problems associated with the pseudoaneurysm, which has exhibited progressive reduction in follow-up imaging (Fig. 3A and B). We present this case to demonstrate the feasibility of the conservative management of vascular complications in pediatric patients, an approach that requires very close clinical and radiological monitoring in experienced centers.
The following are Supplementary data to this article: