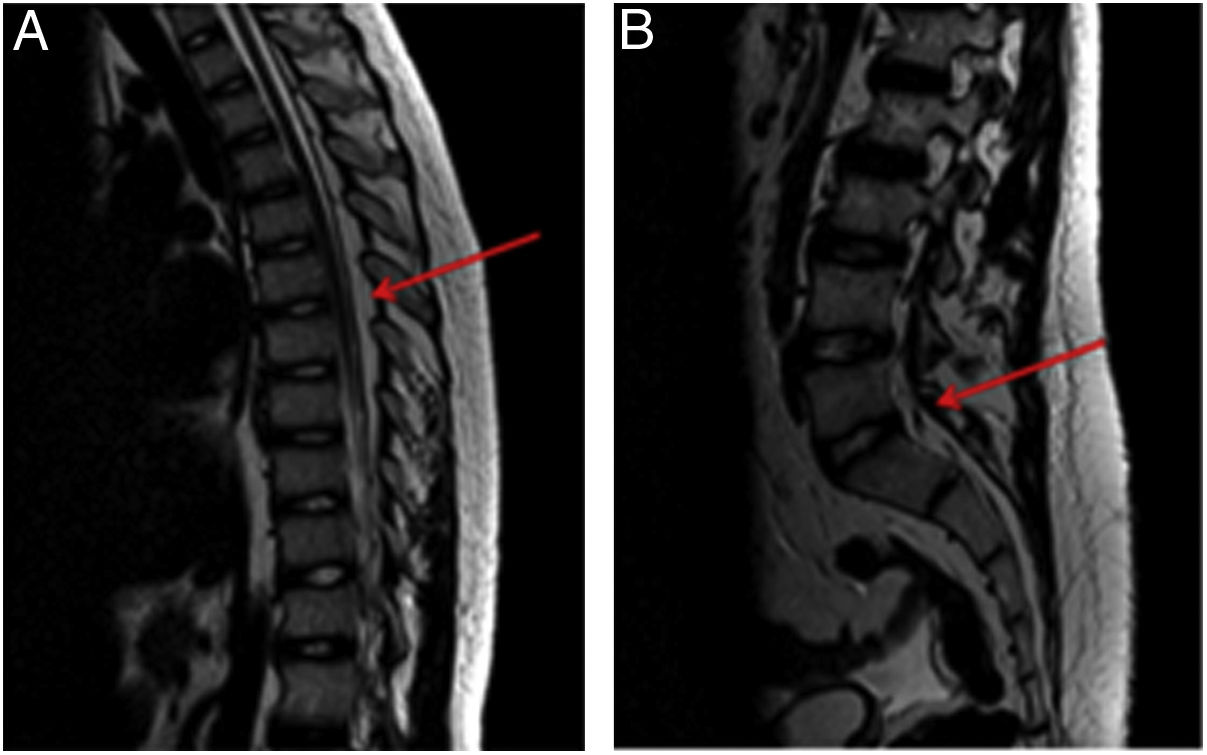
A male patient aged 15 years who had received a diagnosis of Evans syndrome required prolonged treatment with prednisone (2mg/kg/day for 4 weeks, followed by a dose of 1mg/kg day that could not be reduced due to recurrence). At 3 months of treatment, he started experiencing intense, activity-limiting lumbar pain unresponsive to analgesia, progressive, radiating from the lower extremities and decreased proximal strength (4/5). The patient was admitted for evaluation and pain management. A magnetic resonance imaging (MRI) scan of the spine evinced extensive spinal epidural lipomatosis (Fig. 1) secondary to the treatment.
Magnetic resonance of the spine evincing an increase in epidural fat (spinal epidural lipomatosis) resulting in stenosis of the spinal canal at the dorsal (1A) and lumbar (1B) levels. The mass effect was most severe in the L4-S1 segment (1B) and possibly compounded by congenital lumbar canal stenosis.
Conservative treatment with analgesia and rehabilitation was initiated at the same time as mycophenolate mofetil for treatment of Evans syndrome with the aim of tapering off the steroid, which was withdrawn completely 3 months after the diagnosis of lipomatosis without any complications. The patient had a favourable outcome.
Spinal epidural lipomatosis is characterised by an overgrowth of fatty tissue in the epidural sac in the spinal canal that can cause progressive compression of the spinal cord. Steroid therapy has been described as its most common cause1,2, and while spinal epidural lipomatosis is a rare adverse event, it should be suspected in patients presenting with compatible symptoms compatibles (lumbar pain, pain and loss of strength in lower extremities). Magnetic resonance is the gold standard of diagnosis3 and the first-line treatment is conservative—with some patients requiring surgical decompression2—with withdrawal of the steroid whenever possible.
FundingThis research did not receive any external funding.
Conflicts of interestThe authors have no conflicts of interest to declare.