The objective of this study is to analyse long-term outcomes and kidney function in children requiring continuous renal replacement therapy (CRRT) after an acute kidney injury episode.
Patients and methodsA retrospective observational study was performed using a prospective database of 128 patients admitted to the paediatric intensive care unit between years 2006 and 2012 who required CRRT. The subsequent outcomes were assessed in those surviving at hospital discharge.
ResultsOf the 128 children who required CRRT in the paediatric intensive care unit, 71 survived at hospital discharge (54.4%), of whom 66 (92.9%) were followed up. Three patients had chronic renal failure prior to admission to the PICU. Of the 63 remaining patients, 6 had prolonged or relapses of renal function disturbances, but only one patient with atypical hemolytic uraemic syndrome developed end-stage renal failure. The rest had normal kidney function at the last check-up.
ConclusionsMost of surviving children that required CRRT have a positive outcome, presenting low mortality rates and recovery of kidney function in the medium term.
El objetivo de este estudio fue analizar la evolución a largo plazo y la función renal de los niños que han requerido técnicas de depuración extrarrenal continua (TDEC) tras un daño renal agudo.
Pacientes y métodosSe realizó un estudio observacional retrospectivo sobre una base de datos prospectiva en 128 pacientes que requirieron TDEC durante su ingreso en la Unidad de Cuidados Intensivos Pediátrica (UCIP) durante los años 2006 a 2012. Se analizó la evolución de los pacientes que sobrevivieron al alta de la UCIP.
ResultadosSetenta y uno de los 128 niños tratados con TDEC, un 54,4%, sobrevivió al alta y se realizó el seguimiento en 66 de ellos (92,9%). Tres pacientes presentaban insuficiencia renal crónica previa al ingreso en UCIP. De los 63 pacientes restantes, 6 presentaron alteración de la función renal prolongada o recaídas, pero solo un paciente con un síndrome hemolítico-urémico atípico quedó en insuficiencia renal terminal, presentando el resto una función renal normal en la última revisión.
ConclusionesLa mayoría de los niños que precisan TDEC y que sobreviven al episodio agudo presentan una buena evolución posterior con baja mortalidad y recuperación de la función renal a medio plazo.
Acute renal failure (ARF) or acute kidney injury (AKI), which is currently the most used term, is a frequent complication in children who are in critical condition. Its incidence varies between 4.5% and 82%, according to the definition and characteristics of the studied population.1
AKI is associated with high rates of hospital mortality.2 Mortality rates differ according to studies,3–9 depending on the nature of the underlying disease and the severity of renal failure; it is higher in children under the age of two years.10
The aetiology of AKI differs between adults and children.11 The most common causes for AKI in children are tubular necrosis due to heart surgery, shock and/or sepsis, haemolytic uraemic syndrome and, less frequently, acute glomerulonephritis, urinary tract obstruction, toxins (including drugs) and renal parenchymal disease or renal parenchymal disease caused by complications of systemic disorders.12
In adults in critical condition 9.2% of patients with AKI who need renal replacement therapy (RRT) develop chronic renal failure (CRF) or develop it as the disease progresses.13 However, study results in adults cannot be extrapolated to children because, among other reasons, adults have more comorbidities.11
The severity of renal failure, the need for RRT and the number of episodes of AKI are associated with a poorer evolution.14
In addition, it has been observed that minor though severe changes in renal function can cause short-term and long-term complications, such as CRF.15
There are very few studies that have analysed the long-term evolution of AKI in children, and some of them have only analysed the prognosis of children with primary renal disease.16
The aim of this study is to analyse the long-term prognosis and renal function of children who have required RRT.
Patients and methodsA retrospective observational study was performed by reviewing the clinical records of patients included in a prospective database of children who required RRT during their admission to a paediatric intensive care unit (PICU) between 2006 and 2012. The study was approved by the local Ethics Committee.
All the patients between the age of one month and 18 years who were diagnosed with paediatric AKI according to KDIGO criteria17 and who were treated with continuous renal replacement therapy (CRRT) and survived after being discharged from the PICU were selected. The demographic data, the clinical severity scores from the Paediatric Risk of Mortality 2 index,18 the Paediatric Index of Mortality 219 and the Paediatric Logistic Organ Dysfunction,20 the characteristics of the CRRT during admission to the PICU, and progress after being discharged from the PICU were analysed. At each clinical examination, the following parameters were recorded: haemogram (haemoglobin, leukocytes, platelets), biochemistry (urea, creatinine, albumin, sodium, potassium, chloride, calcium, phosphate, magnesium) cystatin, glomerular filtration rate based on cystatin levels (estimated glomerular filtration rate)21, vitamin D, parathormone, arterial blood gas (pH, bicarbonate, base excess), lactic acid, renal ultrasound scan, number of admissions and their characteristics (cause, need and type of renal replacement therapy) and treatment during evolution (bicarbonate, calcium and protein restriction), and mortality (cause and date).
A descriptive statistical analysis was carried out using SPSS 21.0. Qualitative variables are presented as percentages and quantitative variables as medians and interquartile range (IQR) (25th and 75th percentiles), since the population did not have a normal distribution.
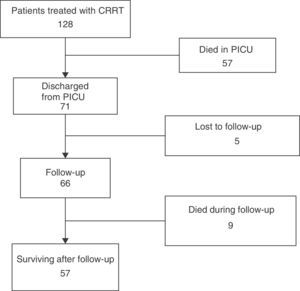
ResultsOne hundred and twenty-eight patients were treated with CRRT between 2006 and 2012. Fifty-seven patients (44.5%) died in the PICU.
Fig. 1 summarises the patients’ evolution. Out of the 71 patients who survived and were discharged from the hospital, nine died subsequently, six (66.7%) due to heart problems, two (22.2%) due to multiple organ failure and one (11.1%) due to brain death, and 57 are currently still alive (Fig. 1). None of the nine patients died due to renal alterations.
The demographic and RRT data from the 71 patients discharged from the PICU are shown in Table 1. Forty-nine (69%) were male. The most frequent diagnosis was congenital cardiopathy in 50 patients (70.4%) (39 patients after heart surgery and seven after a heart transplant), followed by septic shock in seven patients (9.8%). The other 14 patients (19.7%) were admitted for other reasons (four after abdominal surgery, one after respiratory tract surgery, one due to haemolytic uraemic syndrome, two due to tumour lysis syndrome, three due to congenital metabolic diseases, one due to peritonitis associated with a catheter for peritoneal dialysis, one due to massive thrombosis of mitral prosthesis and one due to glomerulonephritis [in a patient with Hodgkin lymphoma]).
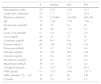
General data from the 71 patients.
| Median | P25 | P75 | |
|---|---|---|---|
| Age (months) | 51.1 | 6.0 | 99.0 |
| Weight (kg) | 15.0 | 6.0 | 25.0 |
| PRISM 2 (mortality risk) | 14.0 | 11.0 | 20.0 |
| PIM 2% (mortality risk) | 12.4 | 5.5 | 25.8 |
| PELOD % (mortality risk) | 16.2 | 1.3 | 24.8 |
| Lactic (mEq/l) | 1.7 | 1.0 | 3.0 |
| Total duration of technique (h) | 158 | 85.0 | 293 |
P25: 25th percentile; P75: 75th percentile.
The average stay at the PICU was 27 days (IQR: 16.5–47.5) and the average duration of mechanical ventilation was 14 days (IQR 7.5–27.5). Twenty patients (28.1%) needed extracorporeal membrane oxygenation.
Analytical data before and after CRRT are shown in Table 2. Only two patients (2.8%) needed dialysis techniques at the time of discharge from the PICU (one had haemolytic uraemic syndrome and another a previous CRF).
Biochemical data before and after CRRT.
| Initial value | Final value | |||||
|---|---|---|---|---|---|---|
| Median | P25 | P75 | Median | P25 | P75 | |
| Creatinine (mg/dl) | 1.2 | 0.6 | 1.7 | 0.5 | 0.3 | 0.8 |
| Urea (mg/dl) | 72.0 | 25.5 | 104.2 | 35.0 | 26.0 | 52.0 |
| Uric (mg/ml) | 8.0 | 6.4 | 9.9 | 1.8 | 1.0 | 2.1 |
| Potassium (mEq/l) | 4.0 | 3.4 | 4.8 | 3.8 | 3.4 | 4.1 |
| Platelets | 156,500 | 84,750 | 238,000 | 119,500 | 75,500 | 189,500 |
Fig. 1 summarises patients’ evolution. Sixty-six patients (92.5%) were monitored after being discharged from the hospital, with an average follow-up period of 40.4 months (IQR 18.4–64.8 months).
In three patients, kidney function alterations lasted over one month and three other children had relapses or new AKI episodes: their characteristics and evolution are shown in Table 3. One of them, an infant with ARF who was later diagnosed with atypical haemolytic uraemic syndrome, suffered from end-stage renal failure and was dialysis-dependant for more than three months, which required renal transplantation.
Characteristics of patients with prolonged alteration of renal function and/or relapse.
| Patient | Age (months) | Gender | Diagnosis | Progress |
|---|---|---|---|---|
| 1 | 3 | Female | Atypical haemolytic-uraemic syndrome | ESKD. Renal transplantation |
| 2 | 6 | Male | Congenital cardiopathy | New AKI that required CRRT following surgery. Complete recovery of renal function. Died after one year due to cardiac arrest caused by brain death. |
| 3 | 180 | Male | Glomerulonephritis. Hodgkin lymphoma | New moderate AKI due to meningococcal sepsis, no CRRT required. Full recovery |
| 4 | 12 | Female | Meningococcal sepsis | Moderate 3-month RF that does not require RRT. Full recovery |
| 5 | 84 | Male | Congenital cardiopathy | Readmission due to PTE that required CRRT. Full recovery |
| 6 | 99 | Male | Congenital cardiopathy | Prolonged 7-month RF that required CRRT. Full recovery after heart transplant |
AKI: acute kidney injury; RF: renal failure: ESKD: end-stage kidney disease; CRRT: continuous renal replacement therapy, PTE: pulmonary thromboembolism.
Three patients had CRF before admission to the PICU. The first had nail-patella syndrome with focal segmental glomeruloesclerosis. Subsequently, he underwent renal transplantation and needed CRRT again after surgery, with favourable progress. The second patient was readmitted for a heart retransplant. His progress was favourable and did not need CRRT. The third patient, diagnosed with lupus erythematosus and associated nephropathy, was admitted due to pneumococcal sepsis and needed CRRT. He progressed well and is currently asymptomatic, with immunosuppressant treatment. At the end of the study, none of the three patients’ renal function had worsened compared with their previous state.
The rest of the patients had normal renal function at the time of the last follow-up visit.
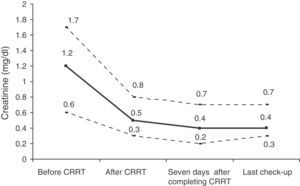
The blood test results from the last check-up are shown in Table 4. In 15 patients, urea levels were over 40, but only three patients had creatinine levels over 1mg/dl (one of the patients with previous CRF who had 1.5mg/dl creatinine, an 18-year-old male with 1.1mg/dl creatinine, which was normal for his age, and a 23-year-old male with a heart transplant undergoing immunosuppressant treatment with tacrolimus who had 1.5mg/dl creatinine). Fig. 2 shown the changes in creatinine. There were no significant changes in creatinine after discharge from the PICU (p=0.892). None of the patients had hyperpotassaemia and only four patients had mild metabolic acidosis. The rest of the analytical parameters were normal. In 52 (78.7%) patients who underwent follow-up a renal ultrasound scan was performed, which was normal in 35 (67.3%). Ten (19.2%) had cortical hyperechogenicity, two (3.8%) had an associated uropathy and five (9.6%) other non-relevant findings.
Haemogram, arterial blood gas and biochemistry at last check-up.
| N | Median | P25 | P75 | |
|---|---|---|---|---|
| Haemoglobin (g/dl) | 65 | 13.2 | 11.6 | 14.3 |
| Leukocytes (cells/mcl) | 65 | 7.7 | 5.3 | 10.9 |
| Platelets (cells/mcl) | 65 | 211,000 | 149,500 | 262,500 |
| pH | 15 | 7.30 | 7.30 | 7.40 |
| Bicarbonate (mmol/l) | 15 | 25 | 21 | 28 |
| BE | 13 | 0.6 | −2.2 | 2.7 |
| Lactic acid (mmol/l) | 6 | 1.9 | 1.3 | 2.9 |
| Urea (mg/dl) | 64 | 33 | 27 | 39 |
| Creatinine (mg/dl) | 64 | 0.4 | 0.4 | 0.7 |
| Sodium (mEq/l) | 64 | 138 | 136 | 141 |
| Potassium (mEq/l) | 71 | 4.2 | 3.6 | 4.6 |
| Chloride (mEq/l) | 50 | 102 | 99.7 | 104 |
| Calcium (mg/dl) | 51 | 9.4 | 9.0 | 9.8 |
| Phosphorus (mg/ml) | 48 | 4.3 | 3.6 | 4,8 |
| Magnesium (mEq/l) | 48 | 1.9 | 1.7 | 2.2 |
| Vitamin D (ng/ml) | 12 | 32.3 | 17.0 | 38.2 |
| PTH (pg/ml) | 6 | 71.5 | 34.0 | 111.7 |
| GFR (ml/min/1.73m2) | 25 | 85 | 66 | 126 |
| Cystatin | 25 | 1.0 | 0.7 | 1.2 |
BE: base excess; GFR: estimated glomerular filtration rate; PTH: parathormone.
During follow-up visits, 59 (89.4%) patients needed to be admitted to hospital. Out of the total of readmissions, 180 (43.5%) were due to heart conditions and 41 (9.9%) due to renal conditions (most of the readmissions were for patients who had end-stage renal failure and needed renal transplantation).
DiscussionIn adults, AKI is associated with a higher risk of CRF, and a high number of patients who need RRT after an AKI episode evolves into CRF.9,13,14,22–28 In a study performed by Lowell in 703 patients with AKI and RRT, 65 (9.2%) developed CRF.13
There are several elements that seem to be associated with the development of CRF after an AKI episode: older age, comorbidities,2,28 clinical duration and acuteness,14,26,27 number of AKI episodes,14 partial recovery of renal function after the acute episode,26 renal disease aetiology23 and the existence of previous CRF.25,27
There are very few studies that have analysed the long-term evolution of children with ARF; some have analysed patients with AKI and, others, like ours, only those who had required RRT. Our work is one of the studies that analyses the long-term evolution of a higher number of paediatric patients (71 children) who needed CRRT for a long period (seven years).
Askenazi et al. studied 174 children who survived an ARF episode for 3–5 years. Sixteen developed CRF after the acute episode, and only 29 of the remaining 126 could be followed-up. Six of these had hyperfiltration and two microalbuminuria, and were the only ones who needed RRT in the acute episode.11
Mammen et al. prospectively monitored for three years the renal function of 126 children who had had AKI, although only 22 had needed RRT. All the patients survived the AKI episode and recovered their previous renal function, except for one who progressed to dialysis dependency. During follow-up, 10% developed CRF and 38% had a slight decrease in renal function. Another 3.2% developed hypertension and 8.2% hyperfiltration, which are long-term risk factors for CRF. In this study, the need for acute dialysis was significantly associated with the development of CRF.1
Spizzirri et al. analysed the evolution of 118 children with haemolytic uraemic syndrome who were monitored for at least 10 years. Of these, 3.4% developed end-stage renal failure and 37% a slight decrease in clearance, hypertension or urine protein.16
In our study, most of the children who needed CRRT regained long-term renal function. Only six patients presented prolonged alterations or relapses, and just one of them, with atypical haemolytic-uraemic syndrome, developed end-stage renal failure. Our results contrast with those of other paediatric studies, which found that a higher number of children with AKI subsequently evolved into CRF.11 This could be because most of our patients had AKI of non-renal origin, caused by cardiogenic shock after heart surgery or by septic shock. When these patients develop multiple organ failure, mortality rates are high, but if they survive, they regain their renal function completely. Children with AKI of renal origin, meanwhile, have lower mortality rates, but the long-term evolution of renal function is worse. This is also the case for adults.23
The percentage of readmissions in our study is very high (89.4%). However, it must be taken into consideration that both the initial AKI episode and the readmissions were caused by the underlying pathology of the patient, mostly congenital cardiopathies, and not by the renal problem. Only nine of our patients died after being discharged from the hospital and none of the deaths were caused by renal alterations.
Our study has some limitations. The main one is that it is a retrospective analysis that has prevented us from obtaining all renal function parameters, since there was no programmed follow-up of the patients. Therefore, it has not been possible to detect minor alterations in renal functions, such as urine protein, microalbuminuria or hyperfiltration, which can predict the risk of developing long-term CRF.1,11 On the other hand, there was no record of diuresis prior to initiating CRRT in our database, nor of the percentage of patients who met AKI criteria due to diuresis alterations and/or creatinine levels. Thus, it is possible that some of the patients who were included in the study had been treated only for diuretic-resistant hypervolemy. Consequently, our study only shows the evolution of patients who needed treatment with CRRT and it is not possible to analyse the association between the evolution of the long-term renal function with diuresis or the severity of the renal alteration before treatment.
Lastly, this is a unicentric study, with a high percentage of children who developed AKI due to cardiogenic shock after heart surgery, and it is possible that it does not represent the general population.
For these reasons, it is necessary to perform multicentric prospective studies that analyse the evolution of children who have had AKI with a specific renal function follow-up protocol.1,11,29
ConclusionsMost of the children who need CRRT and survived the acute episode regained renal function in the medium term, and are now making good progress.
Conflict of interestsThe authors declare that there are no conflicts of interest.
Please cite this article as: Almarza S, Bialobrzeska K, Casellas MM, Santiago MJ, López-Herce J, Toledo B, et al. Evolución a largo plazo de los niños tratados con técnicas de depuración extrarrenal continua. An Pediatr (Barc). 2015;83:404–409.