Behçet's disease (BD) is a disease of unknown aetiology that is rare in the paediatric population. Its typical features are recurrent oral and genital ulcers associated with other systemic ocular, cutaneous, neurologic, vascular and articular manifestations. In exceptional cases, the onset occurs with central nervous system manifestations. We describe the case of a female patient aged 10 years with brainstem meningoencephalitis as the initial presentation of BD that responded well to immunosuppressive therapy.
The patient, born to consanguineous Maghrebi parents, sought care for fever of four days’ duration, oral ulcers, headache and sleepiness. The parents reported that in the past 18 months she had experienced recurrent, but not periodical, four-day episodes of fever (maximum temperature, 39.5°C) and oral ulcers that had not been investigated. The physical examination revealed fever, three ulcers in the oral mucosa, lethargy, nuchal rigidity and upbeat nystagmus with no other apparent neurological abnormalities. The following diagnostic tests were performed: complete blood count and blood chemistry panel (normal [N]); erythrocyte sedimentation rate (18mm/h; N<20); C-reactive protein (89mg/L; N<15), eye fundus examination (N), lumbar puncture (predominantly mononuclear pleocytosis with 950 white blood cells/mL; N<10), cerebrospinal fluid protein (mildly elevated at 68mg/mL; N, 15–40) and glucose (N).
Meningoencephalitis was suspected and empirical treatment with intravenous acyclovir initiated while awaiting the results of PCR tests for herpes simplex virus 1 and 2, which turned out negative. The patient was tested for infectious agents (Mantoux test, antibody testing for HIV, Borrelia, Listeria and syphilis) and cancer (chest radiograph, blood differential test and LDH), and no abnormalities were found. Faecal calprotectin was measured to rule out intestinal inflammatory disease, and was found to be normal.
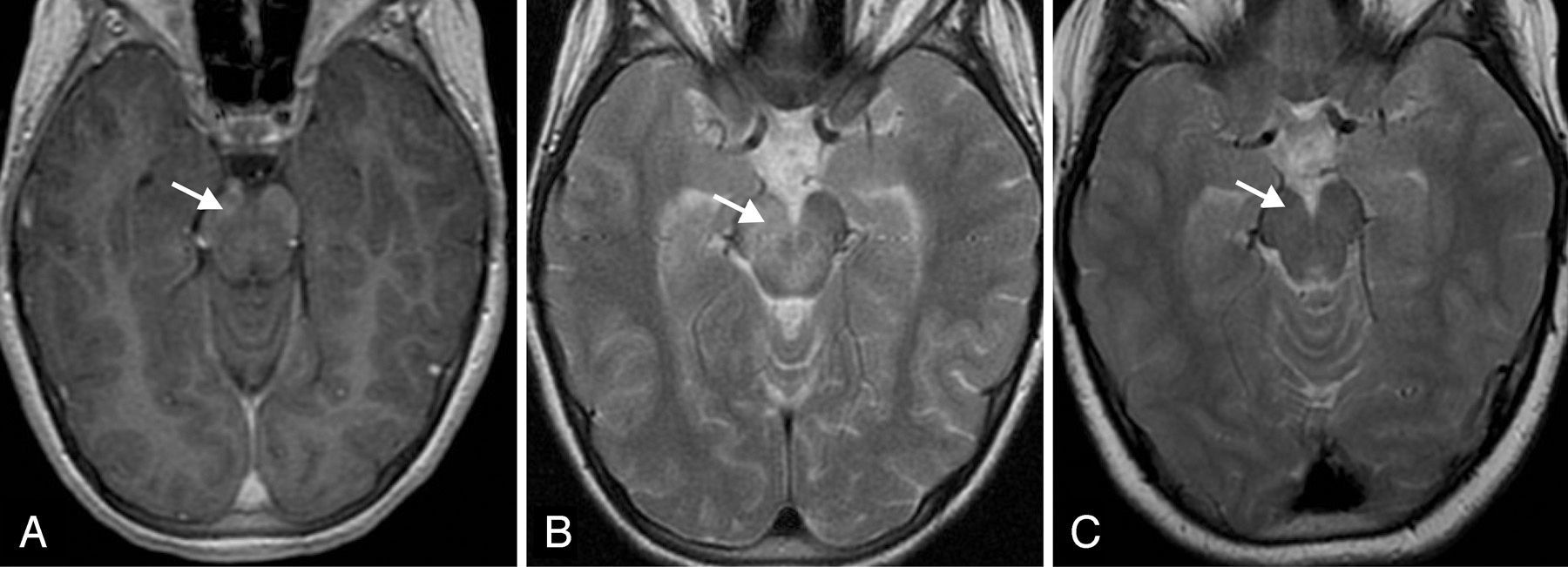
During hospitalisation, she experienced palsy of the VI cranial nerves with ongoing fluctuations in the level of consciousness, leading to performance of a head CT scan with contrast that showed no abnormalities. Forty-eight hours later, the patient underwent a cranial MRI scan that showed a hyperintense T2 signal at the level of the brainstem, centred at the midbrain and extending towards the cerebral peduncles and the pons, with leptomeningeal enhancement and an uptaking punctiform focus at the level of the right cerebellar peduncle (Fig. 1A and B). Given the presence of a brain lesion probably caused by inflammation, the patient was screened for autoimmune diseases, and the antinuclear antibodies, complement and antineutrophil cytoplasmic antibodies tests were all negative. The patient underwent genetic testing for hereditary autoinflammatory diseases (familial Mediterranean fever, periodic fever syndrome due to mevalonate kinase deficiency, TRAPS, BLAU syndrome/early-onset sarcoidosis) that found no mutation associated with her disease. The test for HLA-B51 was negative.
Behçet's disease was suspected based on the clinical presentation and imaging findings, leading to initiation of empirical immunosuppressive therapy with corticosteroids (first with intravenous methylprednisolone bolus injection at 30mg/kg/day for 3 days, and then by the oral route at 2mg/kg/day), colchicine (0.5mg every 12h by the oral route) and azathioprine (1.5mg/kg/day by the oral route).
The patient responded well to the treatment, with a gradual improvement of symptoms that allowed the progressive tapering and eventual discontinuation of corticosteroids. The followup MRI at six months after initiation of treatment did not show any pathological changes (Fig. 1C). At present, the patient continues treatment with azathioprine and colchicine, with good results.
Behçet's disease is diagnosed based on clinical manifestations, and there are no validated classification criteria for the paediatric population. Koné-Paut et al. created an international registry of paediatric patients with BD with the purpose of defining the characteristics of paediatric patients with the disease and subsequently developing classification criteria adapted to this population.1 In 26% of cases of BD, the onset occurs before age 16 years.2 Neurological involvement has been described in 5% to 30% of BD cases in children, most frequently with central nervous system involvement in the form of thrombosis.3–5
Parenchymal involvement is typically found at the level of the brainstem, appearing as a single inflammatory oedematous lesion that is hyperintense on T2 and iso- to hypointense on T1, associated with meningitis.6
To date, no randomised clinical trials have been conducted for the treatment of BD.7 The goals of treatment are symptom control and preventing damage to the affected organ, usually by administration of corticosteroids or immunosuppressants such as azathioprine, ciclosporin or anti-TNF alpha.7 Advances in the knowledge of the pathophysiology of BD will help define a more specific therapeutic approach.
Neurological involvement is an exceptional initial presentation in childhood BD. The characteristic neuroimaging findings and the accompanying characteristic symptoms guide the clinical diagnosis.
Please cite this article as: Rodà D, Martínez-Monseny A, Rebollo M, Iglesias E. Meningoencefalitis de tronco como presentación de Behçet. An Pediatr (Barc). 2016;84:117–118.