Point-of-care lung ultrasound (LUS) is a recognised tool for the diagnosis and follow-up of disease in the NICU.1
We present the case of a male newborn with bronchiolitis caused by RSV admitted at 15 days post birth due to septic shock. The LUS scan evinced extensive consolidation with alveolar collapse in the left lower lobe (LLL) (Fig. 1; Appendix A: supplemental material 1), compatible with pneumonia,2 with changes in echogenicity of the pulmonary parenchyma.3 The patient required mechanical ventilation, haemodynamic support and antibiotherapy. At day 3 of admission, there was evidence of left pneumothorax (chest drainage), with changes in the sonographic appearance: hyperechoic linear artefacts contained in the area of consolidation of the LLL, suggestive of pneumatocele (Fig. 2, Appendix A: supplemental material 2). These images were consistent with the findings of the chest radiograph, and the CT scan confirmed the diagnosis of necrotising pneumonia with pneumatocele (Fig. 3). Panton–Valentine leukocidin–producing Staphylococcus aureus was isolated repeatedly from blood culture (with negative results of tracheal aspirate culture).
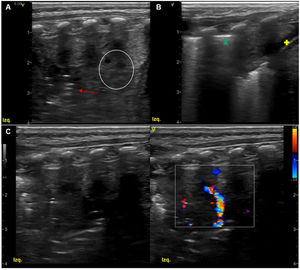
Ultrasound scan at admission. 11 L linear array probe. Longitudinal plane in left posterior hemithorax. (A–C) Large area of consolidation spanning 6 intercostal spaces (EIC) at the base and 3 cm deep, with hepatization and dynamic air bronchogram (red arrow), with Doppler signal and minimal pleural effusion (yellow + sign). Notice the hyperechoic artefact usually generated by the change in acoustic impedance between the subcutaneous tissue and the lung tissue, pleural line (green × sign). (A) Hypoechoic lesions in the consolidated parenchyma with hepatization (white circle), an early sonographic feature associated to parenchymal necrosis.
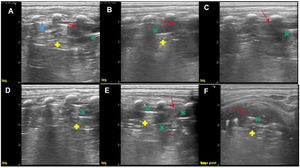
Lung ultrasound at 10 days of admission. 11 L linear array probe. (A–E) Longitudinal plane in left posterior hemithorax (LLL): area of consolidation (red arrows) containing static hyperechoic linear artefacts (green × sign and yellow + sign). This artefact is generated by the change in impedance between the consolidated lung parenchyma and the pneumatocele. (A) This must be differentiated from the features generated by residual pneumothorax (blue star): Pleural line, absence of lung sliding and presence of A-lines. (E) The pneumatocele is surrounded by consolidated parenchyma with hepatization (green × signs). (F) Transversal plan in left posterior lung base: hepatization of parenchyma corresponding to area of consolidation (red arrow) containing hyperechoic artefacts (green × sign) followed by smaller hyperechoic linear artefacts (yellow + sign).
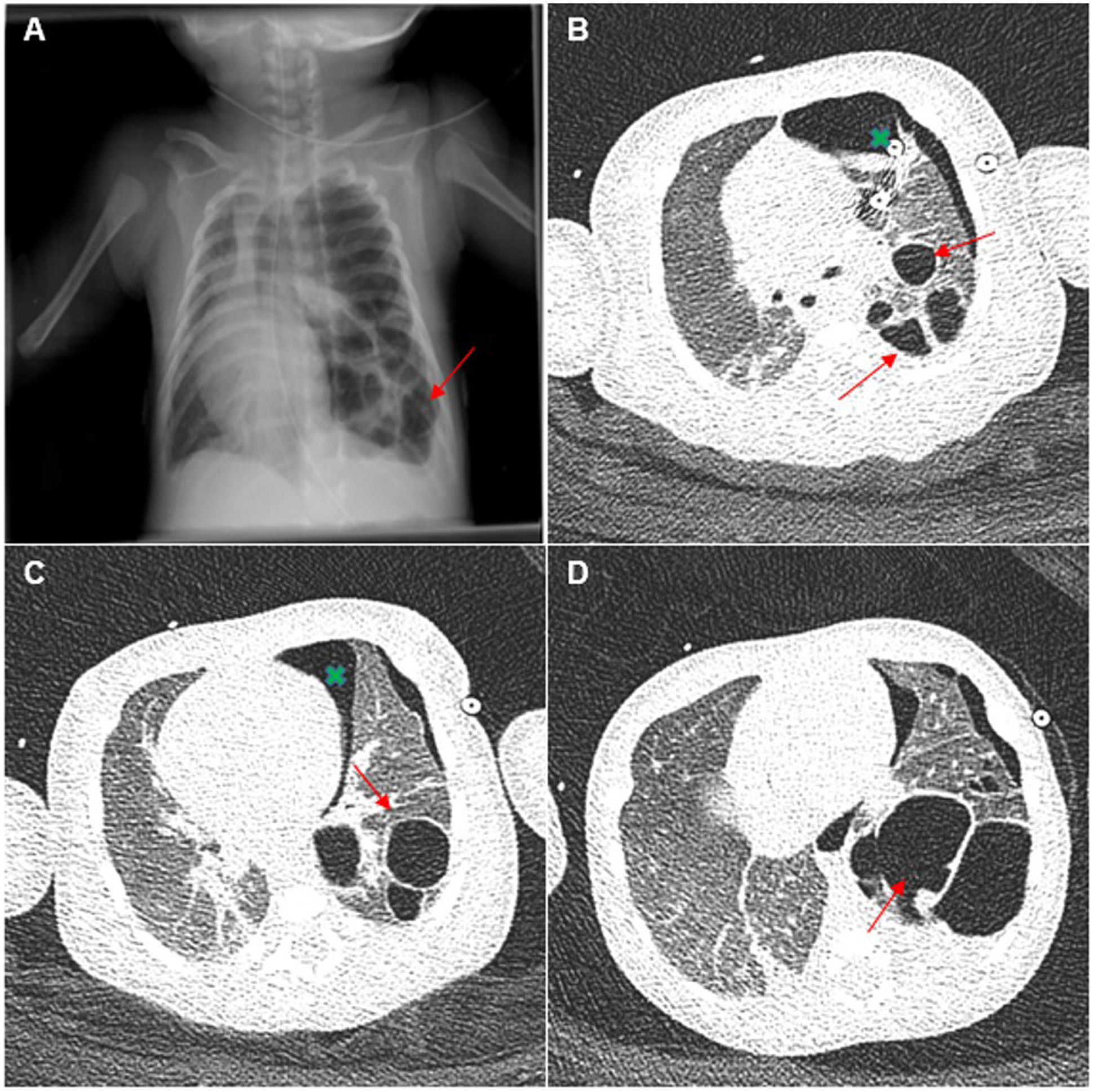
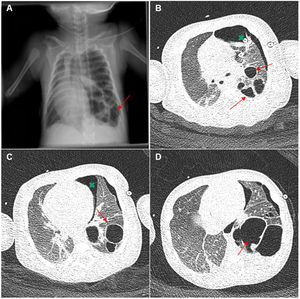
(A) Chest radiograph (anteroposterior decubitus ): multiple gas-filled cavitary lesions in LLL in the same location as the sonographic lesions compatible with pneumatocele (red arrows). (B–D) Chest CT scan with contrast. Lung window: multiple cystic lesions involving nearly the entire left lower lobe of diameters of up to 5 cm compatible with postinfectious cavitation (red arrows). Intact left upper lobe. Left pneumothorax with drainage tube (green × signs).
The correlation between the findings of LUS and CT has been documented in the paediatric and neonatal populations.2,3 To our knowledge, this is the first reported case of pneumatocele diagnosed by ultrasound, highlighting the identification of hyperechoic linear features in the consolidation area as a sign supporting a strong suspicion of pneumatocele in necrotising pneumonia