Posterior reversible encephalopathy syndrome (PRES) is a clinical and radiological diagnosis with a variable neurologic presentation that may include vomiting, headache, changes in consciousness and seizures. The most sensitive test for diagnosis is cranial magnetic resonance imaging (MRI). It yields a typical appearance with bilateral focal lesions, in most cases involving the parietal and occipital lobes.1 Typically, patients exhibit clinical and radiological resolution in response to early treatment.2 We present the cases of 2 paediatric patients that presented with PRES as onset of acute post-infectious glomerulonephritis.
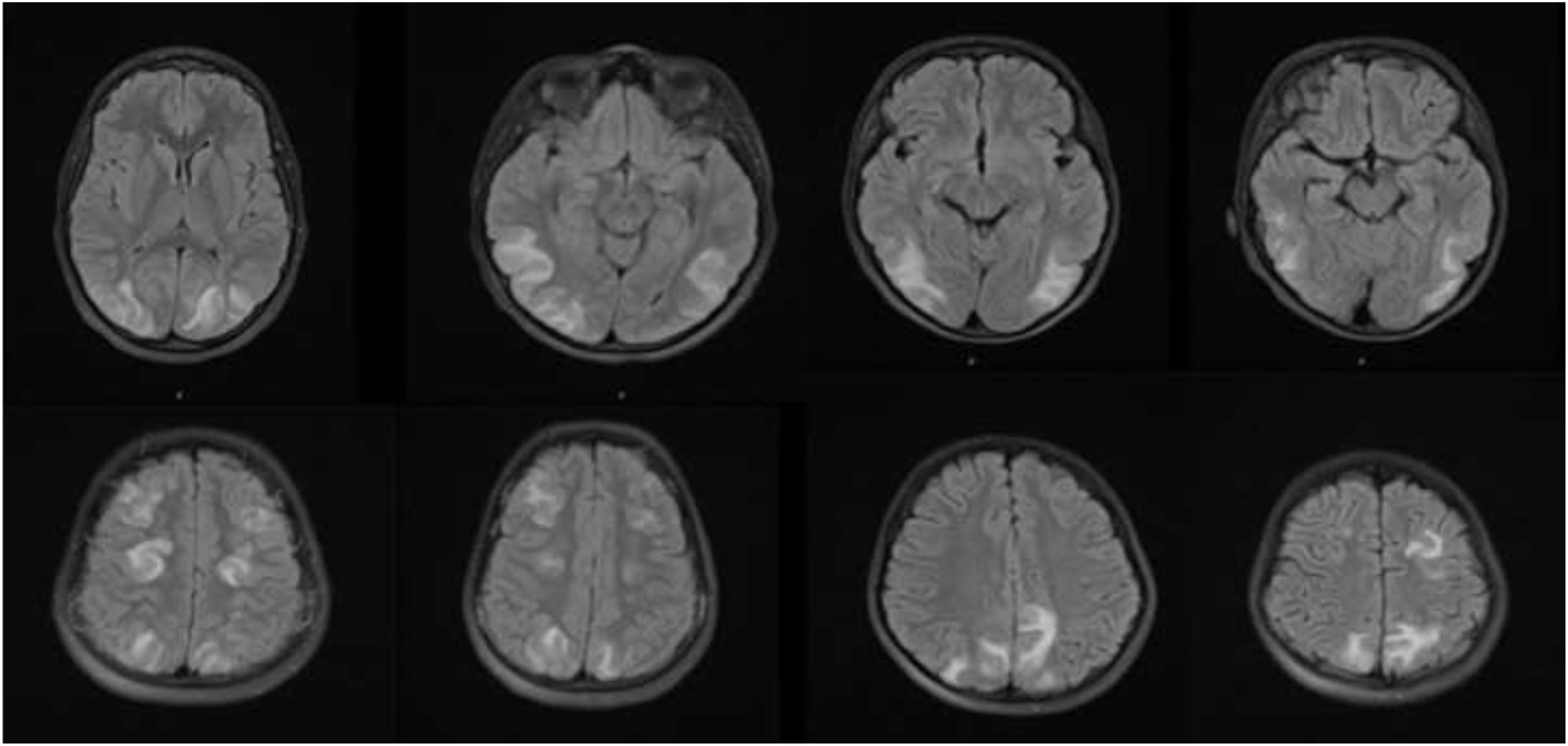
The first patient was a boy aged 11 years who presented with somnolence and generalised tonic-clonic seizures. In the preceding 48 h, he had experienced headache and blurry vision. The most relevant finding of the history-taking was a wound in the right leg that became infected and required oral antibiotherapy the month before. Once the patient was stabilized and the seizures controlled with administration of midazolam, the patient was admitted to the paediatric intensive care unit (PICU). The blood pressure (BP) was 160/100 mm Hg (95th percentile for age, sex and height, 118/78 mm Hg), leading to diagnosis of hypertensive urgency. The findings of blood tests were compatible with stage 1 acute kidney injury (Table 1) and there was macroscopic haematuria. The evaluation was completed with a cranial MRI, with findings compatible with posterior leukoencephalopathy syndrome (Fig. 1) and the salient findings of the workup for assessment of acute glomerulonephritis were a low level of complement factor 3 (C3) and a high anti-streptolysin O (ASO) antibody titre (Table 1). The initial treatment consisted of nicardipine and furosemide, followed by oral amlodipine for a month. At present, the patient has normal renal function, without proteinuria, haematuria or high blood pressure, and with normalization of C3 levels and the neurological examination.
Main laboratory test results of the patients at diagnosis and at 8 weeks of follow-up.
| Patient 1 | Patient 2 | |||
|---|---|---|---|---|
| Diagnosis | 8 weeks | Diagnosis | 8 weeks | |
| Creatinine (mg/dL) | 1 | 0.58 | 0.93 | 0.63 |
| GFR (mL/min/1,73 m2 | 63 | >90 | 62 | >90 |
| Urea (mg/dL) | 56 | 25 | 43 | 19 |
| Sodium (mEq/L) | 135 | 138 | 139 | 137 |
| Potassium (mEq/l) | 4.2 | 4.5 | 1.4 | 3.8 |
| Phosphorus (mg/dL) | 5.3 | 5.3 | 3.9 | 4.1 |
| C3 (mg/dL) | (NR, 80-90)812036108C4 (mg/dL)(NR, 10-408 | 120 | 36 | 108 |
| (NR, 80−90) | ||||
| C4 (mg/dL) | 15 | 28 | 19 | 24.7 |
| (NR, 10−40) | ||||
| ASO (IU/mL) | 395 | 53 | 598 | 195 |
| (NR, 0−160) | ||||
| Urine sediment | Uncountable RBCs/field | No pathological features | 500 RBC/μL | 17 RBC/μL |
| 300 WBC/μL | ||||
| ACR (mg/g) | 1542 | 7.5 | 405.3 | 8.7 |
| (NR < 30) | ||||
ACR, urine albumin to creatinine ratio; ASO, anti-streptolysin O antibodies; C3, complement factor 3; C4, complement factor 4; GFR, glomerular filtration rate estimated with the Schwartz equation (2009); NR, normal range; RBC, red blood cell; WBC, white blood cell.
Magnetic resonance images obtained in the 2 presented cases.
Long TR sequence (T2-weighted and FLAIR) images from patient 1 (A) and patient 2 (B) showing symmetrical areas of cortico-subcortical hyperintensity in the temporo-occipital and frontoparietal regions of both cerebral hemispheres, compatible with posterior reversible encephalopathy syndrome.
The second patient was a boy aged 9 years admitted to the PICU due to hypertensive urgency presenting with generalised tonic-clonic seizures associated with headache and macroscopic haematuria with onset 24 h prior. Ten days before, the patient had received treatment with amoxicillin-clavulanic acid for cervical suppurative lymphadenopathy. At the time of admission, his BP was 170/110 mm Hg (95th percentile for age, sex and height, 120/76 mm Hg). The findings of a head CT scan were normal. Blood test findings were compatible with stage 1 acute kidney injury, with low levels of C3 and elevation of ASO (Table 1). The findings of the cranial MRI were compatible with PRES (Fig. 1B). The patient had a favourable outcome, with neurologic recovery and adequate control of BP after receiving treatment with intravenous labetalol followed by oral amlodipine. At present the patient has normal kidney function with normalization of serum C3 levels and normal BP without pharmacological treatment, although with persistence of microscopic haematuria, a common feature in the follow-up these patients.
We have presented 2 cases of PRES associated with post-infectious glomerulonephritis that were not related to streptococcal pharyngitis, as is typical. The first case occurred following a cutaneous infection and the second following cervical lymphadenopathy, both with elevation of ASO without isolation of the pathogen. The aetiology of PRES is heterogeneous,3 although in children it usually develops in the context of hypertensive seizures secondary to renal disease, chemotherapy or pharmacological immunosuppression, blood disorders or systemic lupus erythematosus. Recently it has been described in association with infection by SARS-CoV-2.4 Early diagnosis is difficult due to the coexistence of nonspecific symptoms, although macroscopic haematuria, which was present in our patients, can suggest a renal aetiology. In our patients, acute encephalitis was initially suspected until the detection of high blood pressure. Since this is an infrequent disease, it is important to maintain a high level of clinical suspicion in the presence of nonspecific neurologic symptoms emerging after an infection of likely streptococcal aetiology. We also ought to highlight the importance of measuring the arterial blood pressure in paediatric patients and be knowledgeable of the reference ranges provided in paediatric guidelines. The treatment is based on controlling the trigger, which in the cases of PRES associated with post-infectious acute glomerulonephritis presented here corresponded to managing the high blood pressure and acute kidney injury. Gewirtz et al5 recently provided evidence that poor control of high blood pressure increases morbidity in these patients due to exacerbation of cerebral oedema, so treatment must be provided, usually in the intensive care unit, with continuous infusion of antihypertensive drugs to gradually reduce BP with the aim of preventing cerebral ischaemia. In paediatrics, the drugs used most widely for management of hypertensive urgency are labetalol and nicardipine, while sodium nitroprusside is falling into disuse because it is considered to carry high risks.6 While PRES is characterised by its reversibility and favourable prognosis in up to 75%–90% of cases, it is a severe disease with a mortality ranging from 3% to 6% and that causes neurologic sequelae in 10%–20% of affected patients.5 For all the above reasons, we underscore the importance of being aware of this disease to maintain a high suspicion in the event of compatible symptoms that would allow early initiation of appropriate treatment, without which it can cause irreversible brain damage.
Please cite this article as: Castellano-Martinez A, Roldán-Cano V, Morales-Arandojo P, Rodriguez-González M. Síndrome de encefalopatía posterior reversible como comienzo de glomerulonefritis postinfecciosa. An Pediatr (Barc). 2022;96:452–454.