The first hours of life of a sick or premature newborn are crucial for its prognosis and therefore delivery should take place in a center prepared for that degree of complexity. When this condition is not met, the newborn must be transferred in an optimal and safe way to the center that can offer the necessary care. The training, staffing, organization and coordination of the neonatal transport team are essential to guarantee a safe transfer. Being aware of the interest and the advances that are currently taking place in this area of pediatrics, the Standards Commission and the Neonatal Transport Commission of the Spanish Society of Neonatology have prepared this document. In it, both the provision of human and material resources necessary as well as the bases of clinical stabilization in transport to carry out the neonatal transfer in a safe way and proportionate to the needs of the critical newborn have been exhaustively reviewed and detailed.
Las primeras horas de vida de un recién nacido enfermo o prematuro son cruciales para su pronóstico y por lo tanto el parto debería acontecer en un centro preparado para ese grado de complejidad. Cuando no se cumple esta condición, el recién nacido debe ser trasladado de un modo óptimo y seguro al centro que pueda ofrecerle los cuidados necesarios. La formación, dotación, organización y coordinación del equipo de transporte neonatal son indispensables para garantizar un traslado en condiciones. Siendo conscientes del interés y los avances que en la actualidad se están produciendo en esta área de la pediatría, la Comisión de Estándares y la Comisión de Transporte Neonatal de la Sociedad Española de Neonatología han elaborado el presente documento. En él, se ha revisado y detallado de forma exhaustiva tanto la dotación de recursos humanos y materiales necesarios como las bases de la estabilización clínica en transporte para llevar a cabo el traslado neonatal de forma segura y proporcionada a las necesidades del recién nacido crítico.
The delivery and the first hours of life of newborn (NB) infants that are vulnerable on account of prematurity or illness largely determine their long-term outcomes. This is why these infants should be born in facilities that are ready to care for them and, if this is not the case, be transported to such facilities safely and efficiently.1,2 Neonatal transport (TN) requires meticulous organization involving the coordination of different resources, patient stabilization in the sending hospital (SH) and subsequent transport and admission to the receiving hospital (RH) where the NB infant can receive the required care. It is essential that the comprehensive and specialised care required by these patients is offered both before and during transport.1 The specific training of the NT team and their experience in neonatal care must guarantee adequate care with the maximum safety for the patient, achieving a decrease in perinatal morbidity and mortality, optimising the use of neonatal intensive care unit (NICU) resources and increasing the satisfaction of parents, families and health care professionals.1,2 An established and specific NT system is an essential resource in the development of the neonatal care system.
The aim of this document is to define the standards required in human and material resources to organise and manage the transport of critical NBs optimally and safely.
Organization of a neonatal transport systemFor NT to meet the efficacy, efficiency and care quality objectives, it is essential that the transport system be organised taking into account the particular needs of each autonomous community in terms of the number of transports of critical NBs and the complexity of neonatal units based on the levels of care offered.3 The support of policymakers and the availability of resources are the elements that have the greatest impact in NT planning.1
Coordination and communicationCoordination and communication are essential for the proper functioning of the NT system.1 Within the public health system, emergency care coordinating teams play a key role, managing the demands of SH and the transport to the RH through the following responsibilities4:
- 1
Coordinating health care services based on the emergency triage.
- 2
Having up-to-date information on the capacity and available services for each facility.
- 3
Obtain and transfer patient medical records.
- 4
Establish protocols for the classification of the critical NB.
- 5
Establish NT pathways based on this classification.
- 6
Guaranteeing availability of beds at the RH.
- 7
Allocating, managing and optimising human and material resources.
- 8
Facilitate communication between the parties involved in NT to reduce transport times.
The main indication for NT involves the impossibility of managing the disorder manifesting in certain infants at the SH based on complexity and diagnostic and therapeutic needs, for instance, the need of surgical intervention, high-frequency oscillatory ventilation or extracorporeal membrane oxygenation (ECMO). Thus, there are different types of NT based on the details of the transport.
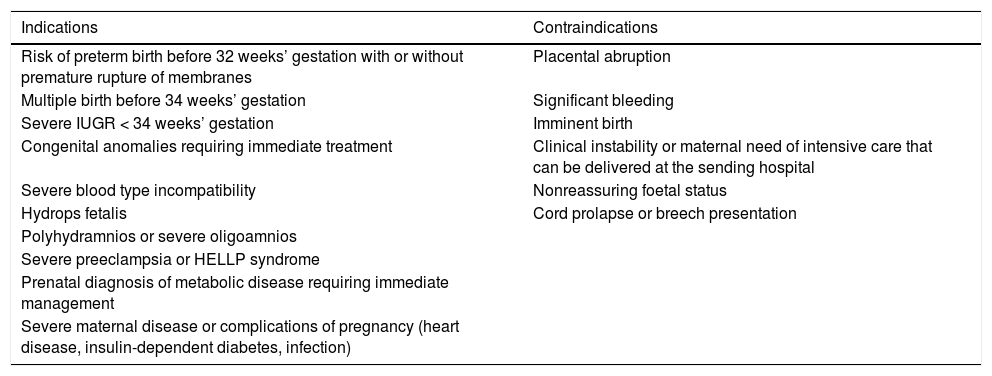
Intrauterine transport: transport of a pregnant woman from one labour and delivery unit to another one of higher complexity that can offer the mother or neonate the care they require or due to maternal and/or foetal compromise. Prenatal diagnosis and correct planning of the birth in the right facility allows perinatal transport under the best possible conditions. Intrauterine transport is the gold standard for mothers and infants whenever possible and has been proven to reduce perinatal morbidity and mortality compared to postnatal transport.5
Some of the aspects that need to be considered in deciding the timing of transport are the risk of imminent birth, the obstetric history, potential complications during transport, correct planning of delivery in a facility with the appropriate level of care for the circumstances, the distance between the hospitals and the availability of beds in the RH6 (Table 1). There are tools available to facilitate decision-making, such as the Malinas score,7 which assesses the stage of labour and cervical dilation to estimate the risk of imminent birth, or the foetal fibronectin test, which combined with the cervical length allows estimating the risk of preterm birth within 7 days.8 While the different tools can be useful, there is no prevailing preference for any of them. At presence, one of the key interventions available is the education of pregnant women on how to identify the early signs and symptoms of preterm birth.2,8
Main indications and contraindications of intrauterine transport to a tertiary care hospital.
| Indications | Contraindications |
|---|---|
| Risk of preterm birth before 32 weeks’ gestation with or without premature rupture of membranes | Placental abruption |
| Multiple birth before 34 weeks’ gestation | Significant bleeding |
| Severe IUGR < 34 weeks’ gestation | Imminent birth |
| Congenital anomalies requiring immediate treatment | Clinical instability or maternal need of intensive care that can be delivered at the sending hospital |
| Severe blood type incompatibility | Nonreassuring foetal status |
| Hydrops fetalis | Cord prolapse or breech presentation |
| Polyhydramnios or severe oligoamnios | |
| Severe preeclampsia or HELLP syndrome | |
| Prenatal diagnosis of metabolic disease requiring immediate management | |
| Severe maternal disease or complications of pregnancy (heart disease, insulin-dependent diabetes, infection) |
HELLP, haemolysis, elevated liver enzymes, low platelet count; IUGR, intrauterine growth restriction.
Adapted from Moreno et al.6
Neonatal transport: optimal NT depends on the correct classification of neonatal units by level of care and the regional organization of health care systems. Thus, the sending or receiving role of each hospital is clearly defined based on their capacity and services. Many newborn infants are transported from one hospital to another during the “golden hours” that are key in neonatal morbidity and mortality and therefore require particularly rigorous care. The outcomes of extremely preterm NBs are poorer in those transported in the first 48 h post birth compared to those delivered in tertiary care hospitals, so it is recommended that efforts be made to ensure delivery of these infants in a setting offering tertiary neonatal care, considering prenatal over postnatal transport a priority as long as it is safe.5
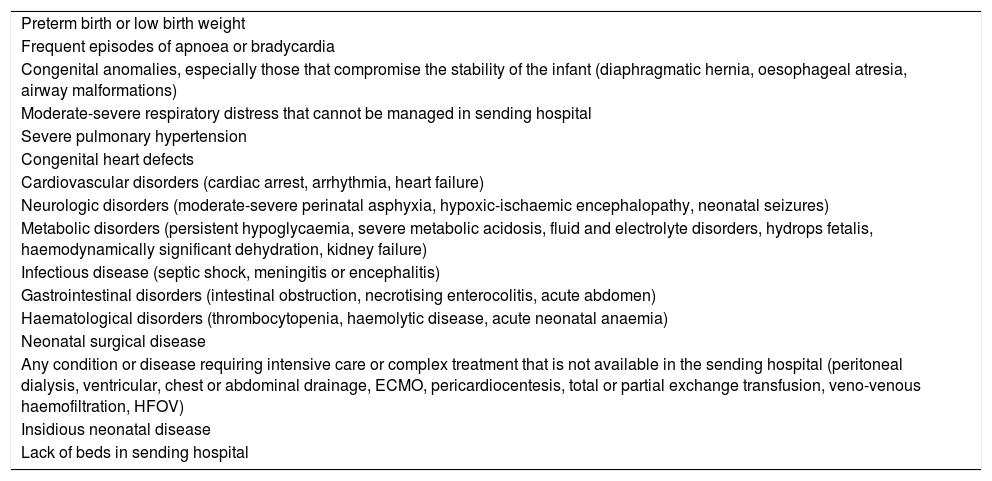
It is of vital importance that NT be organised, planned and executed by appropriately trained staff equipped with the necessary resources. Current technology and knowledge allow for an increasing number of urgent interventions, such as nitric oxide, hypothermia or even ECMO, to be implemented during transport. Table 2 summarises the main indications for neonatal transfer.6
Main indications for neonatal transfer.
| Preterm birth or low birth weight |
| Frequent episodes of apnoea or bradycardia |
| Congenital anomalies, especially those that compromise the stability of the infant (diaphragmatic hernia, oesophageal atresia, airway malformations) |
| Moderate-severe respiratory distress that cannot be managed in sending hospital |
| Severe pulmonary hypertension |
| Congenital heart defects |
| Cardiovascular disorders (cardiac arrest, arrhythmia, heart failure) |
| Neurologic disorders (moderate-severe perinatal asphyxia, hypoxic-ischaemic encephalopathy, neonatal seizures) |
| Metabolic disorders (persistent hypoglycaemia, severe metabolic acidosis, fluid and electrolyte disorders, hydrops fetalis, haemodynamically significant dehydration, kidney failure) |
| Infectious disease (septic shock, meningitis or encephalitis) |
| Gastrointestinal disorders (intestinal obstruction, necrotising enterocolitis, acute abdomen) |
| Haematological disorders (thrombocytopenia, haemolytic disease, acute neonatal anaemia) |
| Neonatal surgical disease |
| Any condition or disease requiring intensive care or complex treatment that is not available in the sending hospital (peritoneal dialysis, ventricular, chest or abdominal drainage, ECMO, pericardiocentesis, total or partial exchange transfusion, veno-venous haemofiltration, HFOV) |
| Insidious neonatal disease |
| Lack of beds in sending hospital |
ECMO, extracorporeal membrane oxygenation; HFOV, high frequency oscillatory ventilation.
Adapted from Moreno et al.6
Return transport: from the facility where intensive care was delivered to the SH or the hospital closest to the family home once the condition that motivated the transfer to or delivery in the RH. It allows optimising the availability of beds in different care settings, regrouping families so they can be closer to the hospitalised children, promoting the interpersonal relationship between professionals and reducing health care costs.
Family and transportThe transport of a highly vulnerable patient, such as a critical NB, is a negative and stressful experience for families that may interfere with bonding and hinder participation of parents in infant caregiving activities. To minimise these negative repercussions, providers must inform parents about every aspect related to the transport of their child and, in adherence with European guidelines, at least one of the parents should be allowed to accompany the infant during transport.2 It is also important to ensure accurate identification of the patient before proceeding with the transfer. Sending hospitals should have a protocol developed in cooperation with the department of obstetrics to facilitate the transfer of mothers that could not be transported with their infants.
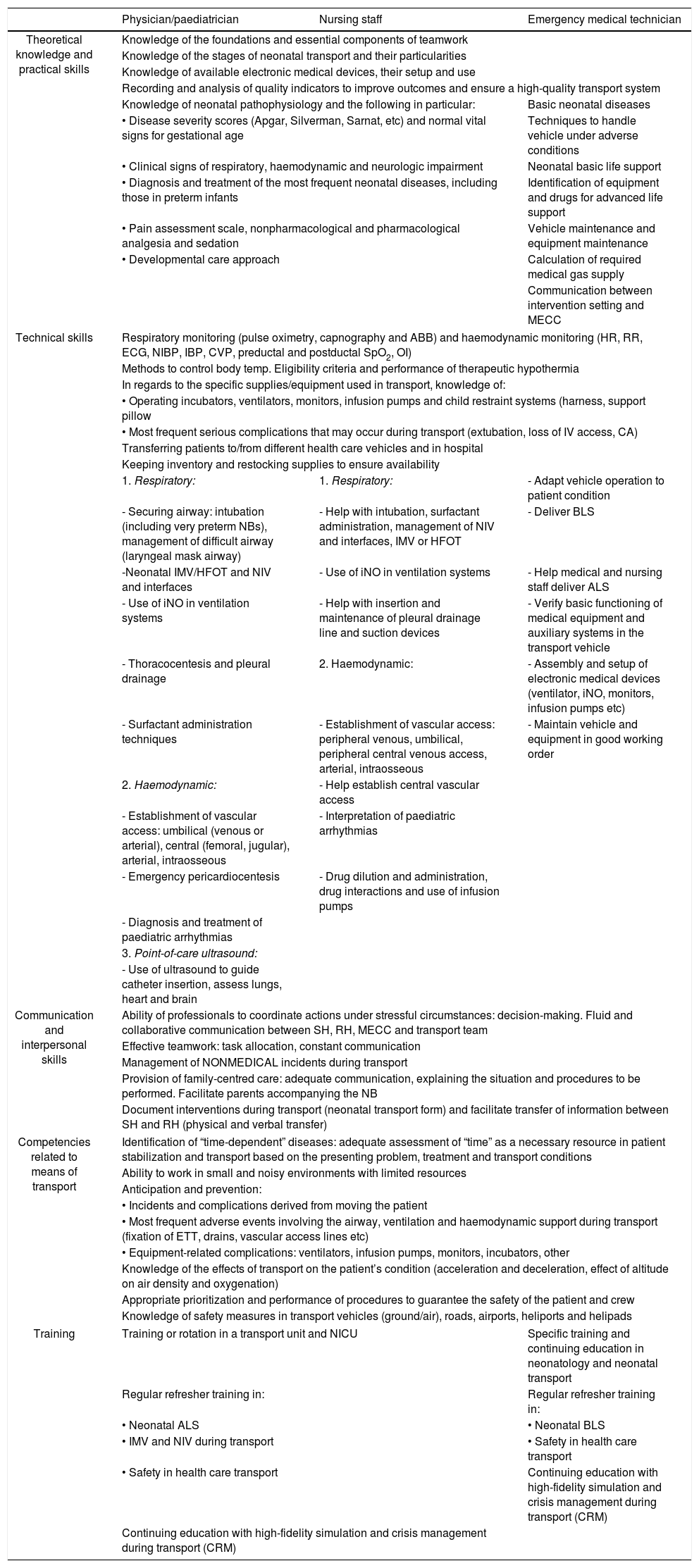
Human resources and skills of the neonatal transport teamIdeally, the NT team will include a paediatrician specialised in neonatology, paediatric nursing staff and an emergency medical technician (EMT-driver or pilot). The entire team must be knowledgeable of the most frequent neonatal problems, be trained in transport and basic and advanced life support (neonatal and paediatric) and support teamwork and leadership. The competence of transport team members in these areas will contribute to the optimal outcome of transport (Table 3). The required competencies include:
- 1
Theoretical knowledge and clinical skills6,9–13
- 2
Technical skills6,9–12
- 3
Communication and social skills6,9
- 4
Skills related to the means of transport14
- 5
Continuing education.9,10,12,15
Human resources and competencies in neonatal transport.
| Physician/paediatrician | Nursing staff | Emergency medical technician | |
|---|---|---|---|
| Theoretical knowledge and practical skills | Knowledge of the foundations and essential components of teamwork | ||
| Knowledge of the stages of neonatal transport and their particularities | |||
| Knowledge of available electronic medical devices, their setup and use | |||
| Recording and analysis of quality indicators to improve outcomes and ensure a high-quality transport system | |||
| Knowledge of neonatal pathophysiology and the following in particular: | Basic neonatal diseases | ||
| • Disease severity scores (Apgar, Silverman, Sarnat, etc) and normal vital signs for gestational age | Techniques to handle vehicle under adverse conditions | ||
| • Clinical signs of respiratory, haemodynamic and neurologic impairment | Neonatal basic life support | ||
| • Diagnosis and treatment of the most frequent neonatal diseases, including those in preterm infants | Identification of equipment and drugs for advanced life support | ||
| • Pain assessment scale, nonpharmacological and pharmacological analgesia and sedation | Vehicle maintenance and equipment maintenance | ||
| • Developmental care approach | Calculation of required medical gas supply | ||
| Communication between intervention setting and MECC | |||
| Technical skills | Respiratory monitoring (pulse oximetry, capnography and ABB) and haemodynamic monitoring (HR, RR, ECG, NIBP, IBP, CVP, preductal and postductal SpO2, OI) | ||
| Methods to control body temp. Eligibility criteria and performance of therapeutic hypothermia | |||
| In regards to the specific supplies/equipment used in transport, knowledge of: | |||
| • Operating incubators, ventilators, monitors, infusion pumps and child restraint systems (harness, support pillow | |||
| • Most frequent serious complications that may occur during transport (extubation, loss of IV access, CA) | |||
| Transferring patients to/from different health care vehicles and in hospital | |||
| Keeping inventory and restocking supplies to ensure availability | |||
| 1. Respiratory: | 1. Respiratory: | - Adapt vehicle operation to patient condition | |
| - Securing airway: intubation (including very preterm NBs), management of difficult airway (laryngeal mask airway) | - Help with intubation, surfactant administration, management of NIV and interfaces, IMV or HFOT | - Deliver BLS | |
| -Neonatal IMV/HFOT and NIV and interfaces | - Use of iNO in ventilation systems | - Help medical and nursing staff deliver ALS | |
| - Use of iNO in ventilation systems | - Help with insertion and maintenance of pleural drainage line and suction devices | - Verify basic functioning of medical equipment and auxiliary systems in the transport vehicle | |
| - Thoracocentesis and pleural drainage | 2. Haemodynamic: | - Assembly and setup of electronic medical devices (ventilator, iNO, monitors, infusion pumps etc) | |
| - Surfactant administration techniques | - Establishment of vascular access: peripheral venous, umbilical, peripheral central venous access, arterial, intraosseous | - Maintain vehicle and equipment in good working order | |
| 2. Haemodynamic: | - Help establish central vascular access | ||
| - Establishment of vascular access: umbilical (venous or arterial), central (femoral, jugular), arterial, intraosseous | - Interpretation of paediatric arrhythmias | ||
| - Emergency pericardiocentesis | - Drug dilution and administration, drug interactions and use of infusion pumps | ||
| - Diagnosis and treatment of paediatric arrhythmias | |||
| 3. Point-of-care ultrasound: | |||
| - Use of ultrasound to guide catheter insertion, assess lungs, heart and brain | |||
| Communication and interpersonal skills | Ability of professionals to coordinate actions under stressful circumstances: decision-making. Fluid and collaborative communication between SH, RH, MECC and transport team | ||
| Effective teamwork: task allocation, constant communication | |||
| Management of NONMEDICAL incidents during transport | |||
| Provision of family-centred care: adequate communication, explaining the situation and procedures to be performed. Facilitate parents accompanying the NB | |||
| Document interventions during transport (neonatal transport form) and facilitate transfer of information between SH and RH (physical and verbal transfer) | |||
| Competencies related to means of transport | Identification of “time-dependent” diseases: adequate assessment of “time” as a necessary resource in patient stabilization and transport based on the presenting problem, treatment and transport conditions | ||
| Ability to work in small and noisy environments with limited resources | |||
| Anticipation and prevention: | |||
| • Incidents and complications derived from moving the patient | |||
| • Most frequent adverse events involving the airway, ventilation and haemodynamic support during transport (fixation of ETT, drains, vascular access lines etc) | |||
| • Equipment-related complications: ventilators, infusion pumps, monitors, incubators, other | |||
| Knowledge of the effects of transport on the patient’s condition (acceleration and deceleration, effect of altitude on air density and oxygenation) | |||
| Appropriate prioritization and performance of procedures to guarantee the safety of the patient and crew | |||
| Knowledge of safety measures in transport vehicles (ground/air), roads, airports, heliports and helipads | |||
| Training | Training or rotation in a transport unit and NICU | Specific training and continuing education in neonatology and neonatal transport | |
| Regular refresher training in: | Regular refresher training in: | ||
| • Neonatal ALS | • Neonatal BLS | ||
| • IMV and NIV during transport | • Safety in health care transport | ||
| • Safety in health care transport | Continuing education with high-fidelity simulation and crisis management during transport (CRM) | ||
| Continuing education with high-fidelity simulation and crisis management during transport (CRM) | |||
ABB, acid-base balance; ALS, advanced life support; BLS, basic life support; CA, cardiac arrest; CPR, cardiopulmonary resuscitation; CRM, crew resource management; CVP, central venous pressure; EMT, emergency medical technician; ETT, endotracheal tube; HFOV, high frequency oscillatory ventilation; HR, heart rate; IBP, invasive blood pressure; IMV, invasive mechanical ventilation; iNO, inhaled nitric oxide; MECC, Medical Emergency Coordination Centre; NB, newborn; NIBP, noninvasive blood pressure; NICU, neonatal intensive care unit; NIV, noninvasive ventilation; OI, oxygenation index; RH, receiving hospital; RR, respiratory rate; SH, sending hospital; SpO2, oxygen saturation; Temp, temperature.
Expertise in transport is acquired naturally if the staff is actively and regularly involved in specialised transport teams and in neonatal and paediatric intensive and emergency care units. The connection to these units is essential to maintain the necessary clinical and technical skills to carry out NT. During transport, health care decisions ultimately rest with the physician. The tasks are allocated to different members of the staff, but there are some tasks that any of the team members should be able to perform in a critical juncture.
Emergency medical technicianThe duties of EMT extend beyond the mere operation of the vehicle and include a series of tasks that are part of the team’s work. The EMT plays an important role in ensuring the safety of the patient and all other riders (transport team and family members) and the maintenance of the transport unit and its equipment. It has to adapt the handling of the vehicle to the characteristics of the patient so it has the least possible impact on the clinical condition of the infant. The participation of EMTs in health care and educational activities allows contemplating a future in which specialization would be accredited, and we advocate for the establishment of the role of paediatric EMT.
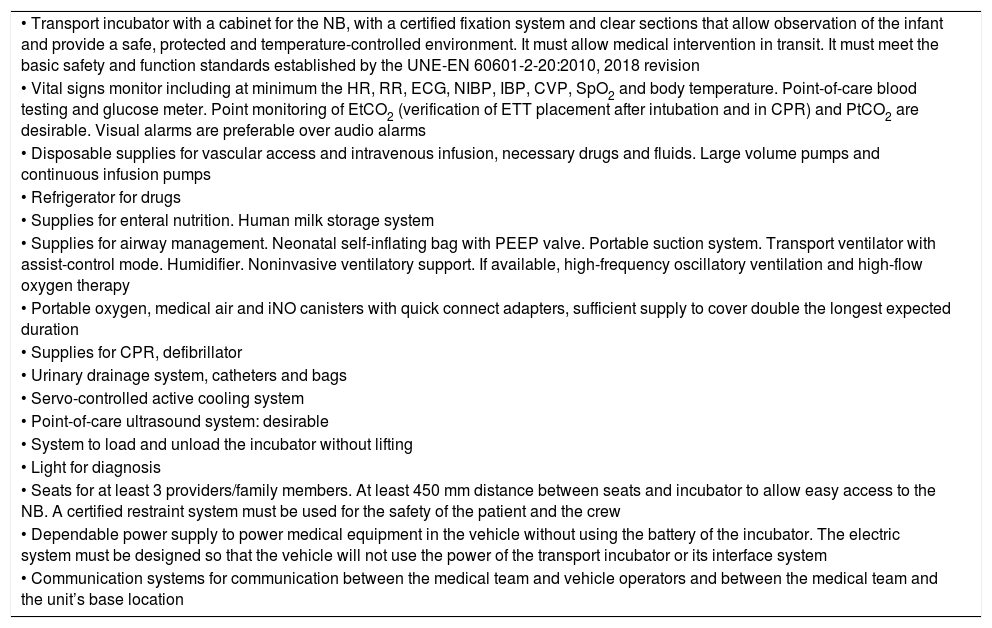
Material resources for neonatal transportWhether transport is urgent or scheduled, the vehicle and equipment must fulfil the requirements of a mobile intensive care unit for the effective transfer of newborn infants of varying maturity and requiring different levels of care and interventions. Interchangeability and interoperability in different settings and scenarios using different transport vehicles must be ensured. Table 4 summarises the material resources that are recommended for NT.2,16,17
- a
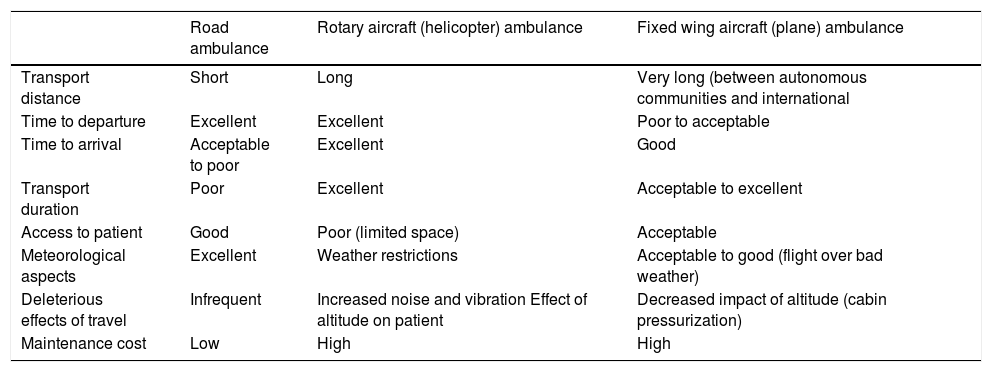
Transport vehicles:Table 5 compares the different types of transport vehicles.
- 1
Ground transport: availability of a vehicle exclusively dedicated to NT is recommended, along with specific maintenance and cleaning protocols.
- 2
Air transport: an air ambulance is an aircraft designed, equipped and dedicated to the transport of patients that may require medical care in transit, such as ambulance service airplanes or helicopters. The vehicle triage should be based on the urgency of the condition (considering time-dependent outcomes) and the transport distance and duration. When the isochrone map (showing the time required to travel from a certain point to a certain hospital) shows a time greater than 1 h or the distance exceeds 150 km, use of a helicopter is recommended, and in case of longer travel, use of an airplane, taking into account the available resources and the experience of the transport team.18 Air transport involves greater specialisation of the staff and is subject to limitations based on geography, weather conditions and night travel that are not standardised across Spain.4 Health care devices and products must function safely under local temperature and humidity conditions, the vibration and shock caused by movement of the air ambulance, air pressure variations and electromagnetic interference as established in the UNE EN 13718-1:2014 and EN 13718-2:2015 standards.19,20
Table 5.Comparison of the advantages and disadvantages of the different vehicles used in neonatal transport.
Road ambulance Rotary aircraft (helicopter) ambulance Fixed wing aircraft (plane) ambulance Transport distance Short Long Very long (between autonomous communities and international Time to departure Excellent Excellent Poor to acceptable Time to arrival Acceptable to poor Excellent Good Transport duration Poor Excellent Acceptable to excellent Access to patient Good Poor (limited space) Acceptable Meteorological aspects Excellent Weather restrictions Acceptable to good (flight over bad weather) Deleterious effects of travel Infrequent Increased noise and vibration Effect of altitude on patient Decreased impact of altitude (cabin pressurization) Maintenance cost Low High High - 1
- b
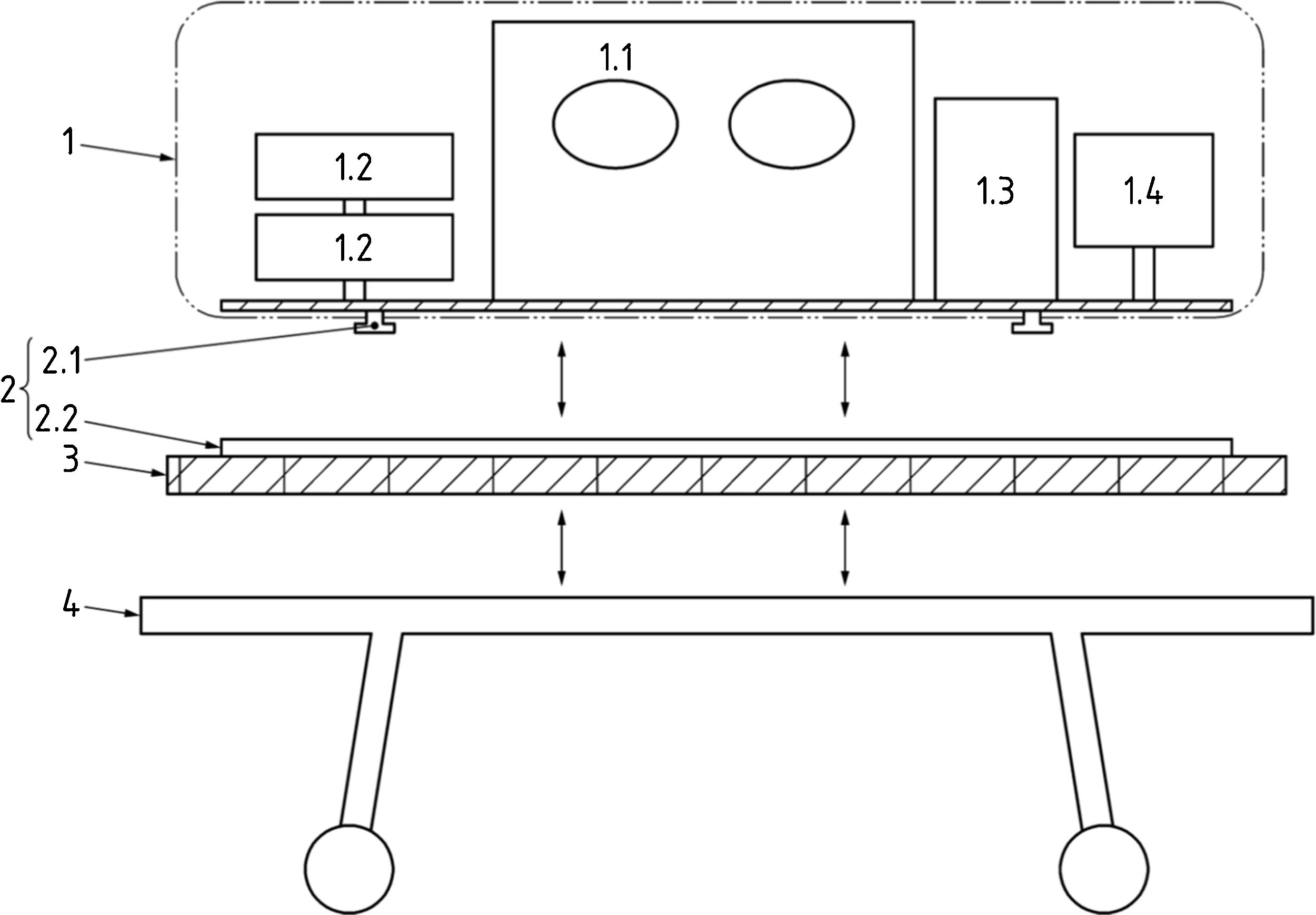
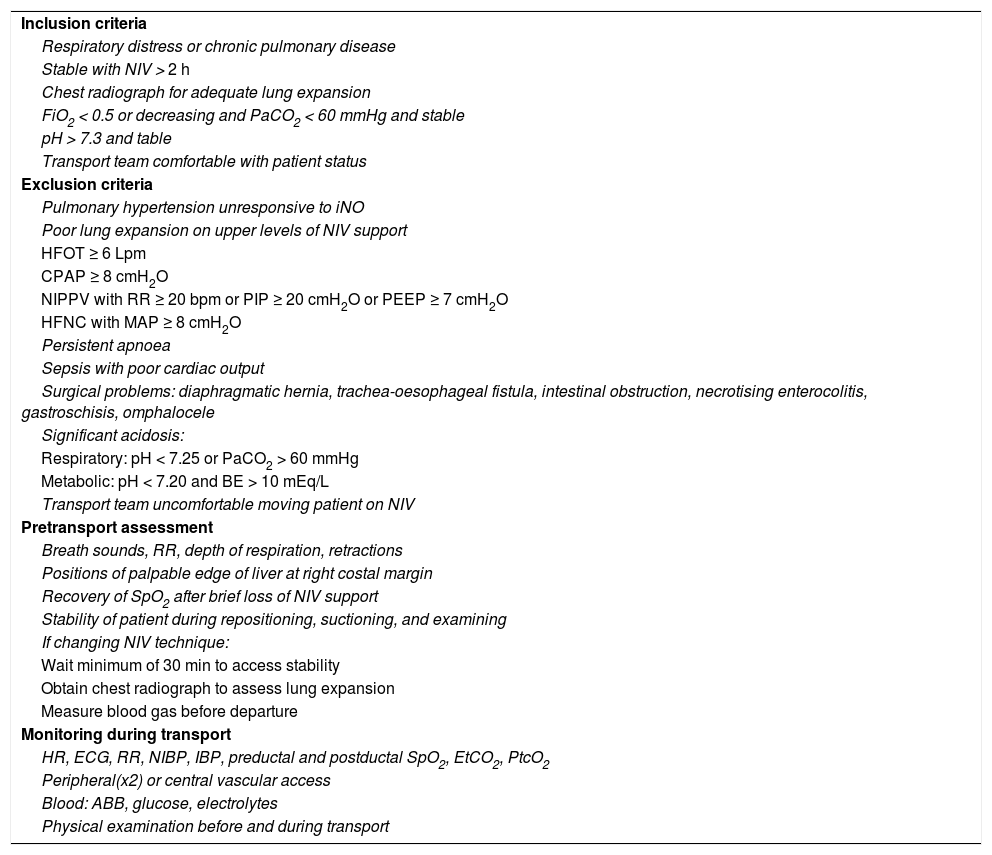
Transport incubator system (TIS) (Fig. 1)
Figure 1.Transport incubator system fixed to the frame of the vehicle (UNE-EN 13976-1). Components of the transport incubator system (TIS): 1.1: incubator; 1.2: syringe pump; 1.3: ventilator; 1.4: monitor. Fixation system: 2.1: track studs; 2.2: track rails; 3: Interface to be used if track rails cannot be fixed directly to the stretcher system. If the interface is to be attached to undercarriage, original fixation points on the undercarriage should be used; 4: Stretcher system (stretcher/undercarriage/stretcher support, etc).
Equipment and supplies for neonatal transport.
| • Transport incubator with a cabinet for the NB, with a certified fixation system and clear sections that allow observation of the infant and provide a safe, protected and temperature-controlled environment. It must allow medical intervention in transit. It must meet the basic safety and function standards established by the UNE-EN 60601-2-20:2010, 2018 revision |
| • Vital signs monitor including at minimum the HR, RR, ECG, NIBP, IBP, CVP, SpO2 and body temperature. Point-of-care blood testing and glucose meter. Point monitoring of EtCO2 (verification of ETT placement after intubation and in CPR) and PtCO2 are desirable. Visual alarms are preferable over audio alarms |
| • Disposable supplies for vascular access and intravenous infusion, necessary drugs and fluids. Large volume pumps and continuous infusion pumps |
| • Refrigerator for drugs |
| • Supplies for enteral nutrition. Human milk storage system |
| • Supplies for airway management. Neonatal self-inflating bag with PEEP valve. Portable suction system. Transport ventilator with assist-control mode. Humidifier. Noninvasive ventilatory support. If available, high-frequency oscillatory ventilation and high-flow oxygen therapy |
| • Portable oxygen, medical air and iNO canisters with quick connect adapters, sufficient supply to cover double the longest expected duration |
| • Supplies for CPR, defibrillator |
| • Urinary drainage system, catheters and bags |
| • Servo-controlled active cooling system |
| • Point-of-care ultrasound system: desirable |
| • System to load and unload the incubator without lifting |
| • Light for diagnosis |
| • Seats for at least 3 providers/family members. At least 450 mm distance between seats and incubator to allow easy access to the NB. A certified restraint system must be used for the safety of the patient and the crew |
| • Dependable power supply to power medical equipment in the vehicle without using the battery of the incubator. The electric system must be designed so that the vehicle will not use the power of the transport incubator or its interface system |
| • Communication systems for communication between the medical team and vehicle operators and between the medical team and the unit’s base location |
CPR, cardiopulmonary resuscitation; ECG, electrocardiogram; EtCO2, capnography; ETT, endotracheal tube; HR, heart rate; IBP, invasive blood pressure; iNO, inhaled nitric oxide; NB, newborn; NIBP, noninvasive blood pressure; RR, respiratory rate; PEEP, positive end-expiratory pressure; PtCO2, transcutaneous carbon dioxide pressure; SpO2, oxygen saturation; temp, temperature.
Source: Jourdain et al,2 Lee et al,16 British Columbia Transfer Record.17
The TIS is comprised of a portable incubator combined with the rest of the equipment. It is important to control its weight and bulk to ensure the safety of vehicle occupants.21 The total mass of the system should not exceed 140 kg and should not affect the stability or manoeuvrability of the ambulance.
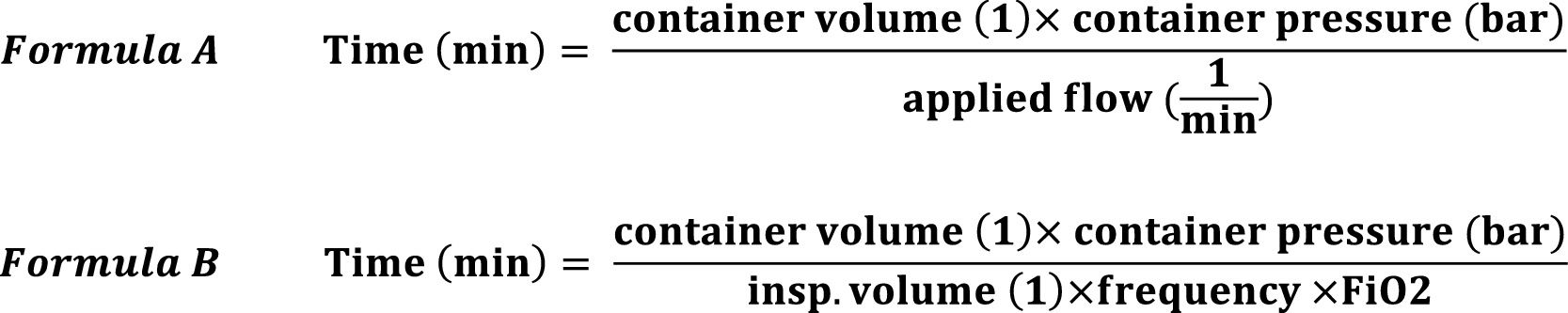
To ensure the power supply, the total usage of the TIS should not exceed 1200 W connected to a 230 V alternating current source, 720 W connected to a 24 V direct current (DC) source or 360 W connected to a 12 V DC source. The incubator must have a rechargeable battery serving as a portable power supply capable of maintaining the temperature for at least 90 min. The TIS must be equipped with oxygen and medical gas, and it is essential to calculate the necessary supply of gases for transport, especially when covering long distances (Fig. 2). All the components must be safely secured so they cannot move during transit, in adherence with the EN 1789:2007 + A2:2014 standards for ground ambulances and the EN 13718-1:2014 and EN 13718-2:2015 standards for air ambulances.
Calculation of the medical gas supply needed in transport. Formula A (time in minutes of medical gas autonomy delivering a constant flow with a flowmeter). Formula B (time in minutes autonomy in patient connected to mechanical ventilation).
FiO2, inspired fraction of oxygen; IRV, inspiratory reserve volume.
The requirements for TISs in regards to suspension/shock absorption, temperature conditions, vibration, mechanical integrity, electromagnetic compatibility, mass, electricity, fixation of component parts and interface conditions during incubator transport are established in the UNE-EN 13976-1:201822 and EN 13976-2:2018 standards.23 No system is completely effective in attenuating mechanical vibration, and gel mattresses in incubators are only partially effective in reducing its transmission.24 Caution must be exerted to avoid obstructing air inlets and vent holes with blankets, which can cause an increase in temperature above safe levels. The noise level inside the incubator should not exceed 60 dB during regular use or 80 dB when an alarm is sounding. Use ear defenders is recommended in every transport, although these devices only reduce noise by a maximum of 7 dB. New systems for NT must be develop that reduce noise exposure.25 Exposure to the highest intensity of light occurs during vehicle loading and unloading. This exposure should be minimised or prevented using eye covers, light-reducing cot covers or tinting of the transport cot to reduce the illuminance without compromising the ability to observe the neonate during transport.26
Pretransport stabilizationTransport causes noise, vibration, acceleration and deceleration forces and temperature fluctuations in addition to detracting from the quality of care due to limited space and restricted mobility. The transport team must stabilise the infant before transport to be able to face a risk situation that will be compounded by the effects of transport under the best possible conditions.25
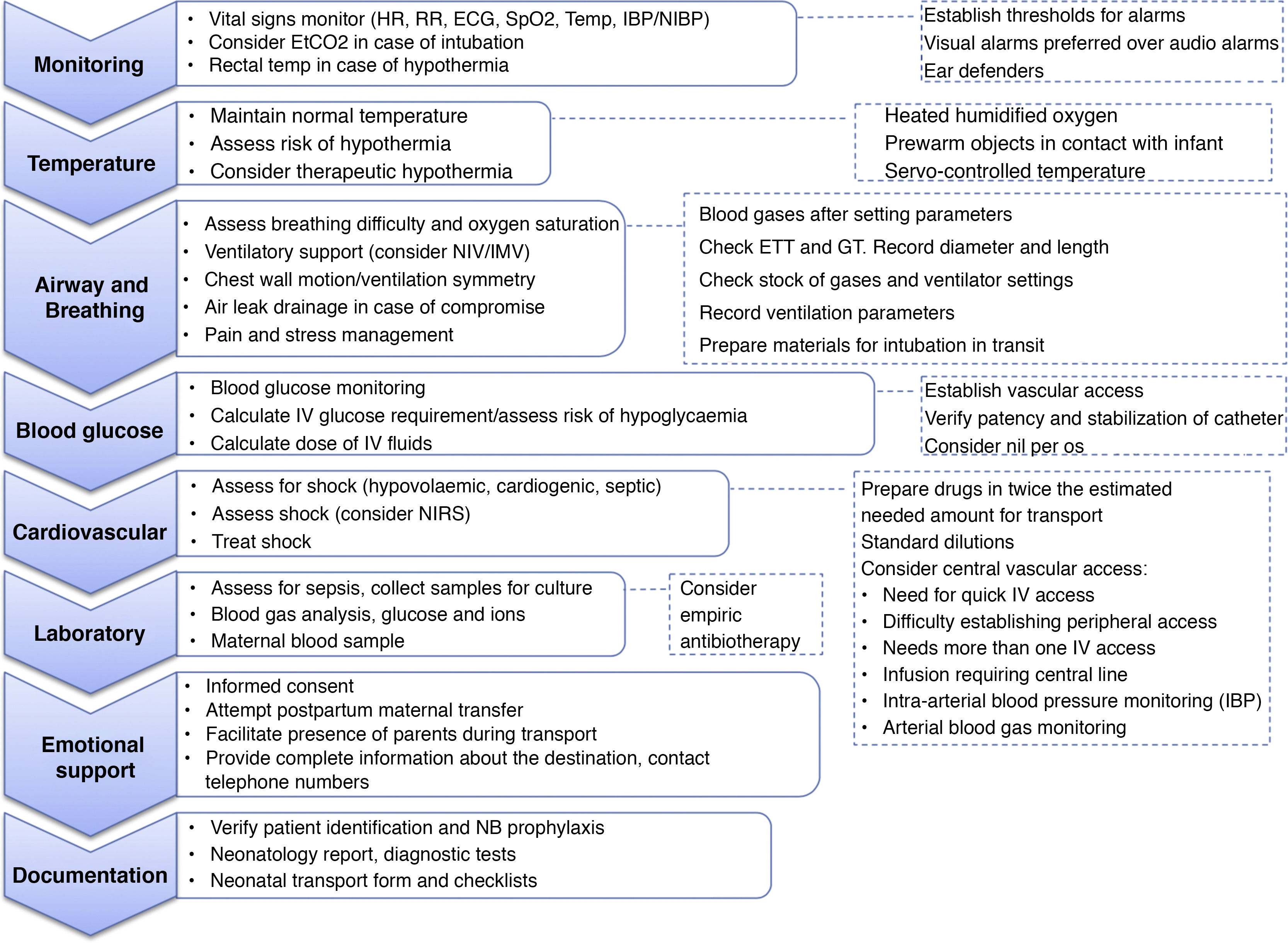
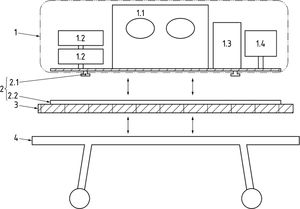
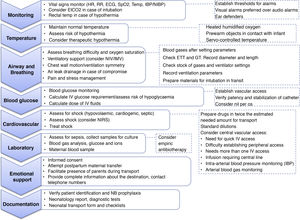
Leaving aside the available equipment and technology, the guiding principles of neonatal care are improving safety through the standardization of procedures and eradicating preventable adverse events, which entails controlling body temperature, securing the airway and ventilatory support, placement of catheters for intravenous access and drainage, haemodynamic stabilization with maintenance of glucose levels in the normal rage and family support (Fig. 3). The stabilization of the critical NB must adhere to the ABCDE protocol and the staff should be constantly re-evaluating the support and care provided to the infant. The breathing of the patient should be evaluated to determine whether it is possible to transport the infant under noninvasive ventilation applying appropriate selection criteria27 (Table 6); administration of surfactant and/or inhaled nitric oxide or placement of a chest tube may be necessary before transport. If available, high-frequency oscillatory ventilation may be indicated for stabilization of the most critically ill infants.28
Pretransport stabilization.
ECG, electrocardiogram; EtCO2, end-tidal carbon dioxide; ETT, endotracheal tube; GT, gastric tube; HR, heart rate; IBP, invasive (intra-arterial) blood pressure; IMV, invasive mechanical ventilation; IV, intravenous; NB, newborn; NIBP, noninvasive blood pressure; NIRS, near infrared spectroscopy; NIV, noninvasive ventilation; RR, respiratory rate; Rx, X-ray; SpO2, oxygen saturation; temp, temperature.
Criteria for considering non-invasive mechanical ventilation during transport.
| Inclusion criteria |
| Respiratory distress or chronic pulmonary disease |
| Stable with NIV > 2 h |
| Chest radiograph for adequate lung expansion |
| FiO2 < 0.5 or decreasing and PaCO2 < 60 mmHg and stable |
| pH > 7.3 and table |
| Transport team comfortable with patient status |
| Exclusion criteria |
| Pulmonary hypertension unresponsive to iNO |
| Poor lung expansion on upper levels of NIV support |
| HFOT ≥ 6 Lpm |
| CPAP ≥ 8 cmH2O |
| NIPPV with RR ≥ 20 bpm or PIP ≥ 20 cmH2O or PEEP ≥ 7 cmH2O |
| HFNC with MAP ≥ 8 cmH2O |
| Persistent apnoea |
| Sepsis with poor cardiac output |
| Surgical problems: diaphragmatic hernia, trachea-oesophageal fistula, intestinal obstruction, necrotising enterocolitis, gastroschisis, omphalocele |
| Significant acidosis: |
| Respiratory: pH < 7.25 or PaCO2 > 60 mmHg |
| Metabolic: pH < 7.20 and BE > 10 mEq/L |
| Transport team uncomfortable moving patient on NIV |
| Pretransport assessment |
| Breath sounds, RR, depth of respiration, retractions |
| Positions of palpable edge of liver at right costal margin |
| Recovery of SpO2 after brief loss of NIV support |
| Stability of patient during repositioning, suctioning, and examining |
| If changing NIV technique: |
| Wait minimum of 30 min to access stability |
| Obtain chest radiograph to assess lung expansion |
| Measure blood gas before departure |
| Monitoring during transport |
| HR, ECG, RR, NIBP, IBP, preductal and postductal SpO2, EtCO2, PtcO2 |
| Peripheral(x2) or central vascular access |
| Blood: ABB, glucose, electrolytes |
| Physical examination before and during transport |
ABB, acid-base balance; BE, base excess; CPAP, continuous positive airway pressure; ECG, electrocardiogram; EtCO2, end-tidal carbon dioxide; FiO2, fraction of inspired oxygen; HFNC, high flow nasal cannula; HFOT, high-flow oxygen therapy; HR, heart rate; IBP, invasive (intra-arterial) blood pressure; iNO, inhaled nitric oxide; MAP, mean airway pressure; NIBP, noninvasive blood pressure; NIPPV, nasal intermittent positive pressure ventilation; NIV, noninvasive ventilation; PaCO2, partial pressure of carbon dioxide; PEEP, positive end-expiratory pressure; PIP, peak inspiratory pressure; PtcO2 transcutaneous oximetry; RR, respiratory rate; SpO2, peripheral oxygen saturation.
Adapted from Null et al.28
Providers must be acquainted with the ventilator and the selected modality of support and should be capable of making adjustments as required by environmental and clinical changes during transport. The difficulty of assessing chest wall motion and performing lung auscultation during transport due to mechanical vibration and background noise must be taken into account. Adequate stocking of batteries and gas canisters is important to ensure the supply of power and medical gases during transfers and ambulance transport.28 The use of checklists during intubation and other procedures can shorten the execution time and improve success rates.29
Depending on the timing and means of transport, there may be important fluctuations in body temperature. In the case of transported NBs with hypoxic-ischaemic encephalopathy, active hypothermia is key to achieve the target temperature on arrival to the RH and minimises the risk of overcooling compared to passive hypothermia. Portable devices to monitor brain function may allow assessment of the patient during stabilization in units lacking equipment, although they cannot be used to monitor the patient and consider changes in management during transport due to vibration artifacts.28
The concept of time-dependent outcome is relevant in NBs requiring immediate surgical intervention or urgent advanced life support that can only be provided in an intensive care setting. An ongoing re-evaluation of the care plan, the anticipation of complications, technical skills and care team cohesiveness are key factors in the successful stabilization of the patient.
Neonatal transport and COVID-19Despite the apparent rarity of vertical transmission of SARS-CoV-2, the transport group of the Società Italiana di Neonatologia recommends approaching each possible case as confirmed, even if the SH defines it as suspected. The only additional equipment required is personal protective equipment, although fitting specific filters in the valves of the ventilator. The partition between the cab and the patient compartment should be kept closed.30
The European Society of Paediatric and Neonatal Intensive Care (ESPNIC) has recommended handling incubator transports as if they were open stretcher transports as regards the use of personal protective equipment.31,32 It also recommended placing the NB in a suitably sized plastic bag to reduce the need for heating or humidification as well using port hole covers to minimise air leaks. Although it is not aligned with the principles of family-centred care, transporting infants without the parents, whether symptomatic or not, is also recommended to protect the transport team.
ConclusionsThe first hours of life of an ill or preterm newborn infant are crucial to the outcome of the patient, and therefore delivery should take place in a hospital with the necessary resources to manage the corresponding level of complexity. When this is not the case, the neonate must be provided with optimal, professional transport to a facility that can offer the required care. The training and coordination of the neonatal transport team and the resources at its disposal are key to guarantee transport under adequate conditions. Each transport team must perform data collection and documentation of any incidents during transport to allow quality assessment and identification of opportunities for improvement in order to increase patient safety throughout the transport process.
Conflicts of interestThe authors have no conflicts of interest to declare.
The members of the Neonatal Transport Committee of the Sociedad Española de Neonatología (SENeo) are Olalla Rodríguez Losada, Laura Sánchez García, Teresa Esclapés Giménez, Rafael Gómez Zafra, Miguel Ángel Cortajarena Altuna, Marta Costa Romero, Miguel Ángel García Cabezas, Beatriz Curto Simón, Natalia Mandiá Rodríguez, Félix Morales Luengo, Javier Díez-Delgado Rubio, Marta Sardá Sánchez, Luis Pérez Baena, Isabel Sanz Ruiz, Isabel de las Cuevas Terán and Raquel Jordán Lucas.
The members of the Standards Committee of the SENeo are María L. Couce Pico, Héctor Boix Alonso, María Cernada Badía, María Gracia Espinosa Fernández, Noelia González Pacheco, Alejandro Pérez Muñuzuri, M. Dolores Sánchez-Redondo Sánchez-Gabriel and Ana Martín Ancel.
Please cite this article as: Jordán Lucas R, Boix H, Sánchez García L, Cernada M, de las Cuevas I, Couce ML. Recomendaciones sobre el perfil de competencias y estándares del sistema de traslado neonatal en España. An Pediatr (Barc). 2021;94:420.
Appendix Alists the members of the Neonatal Transport Committee of the Sociedad Española de Neonatología (seNeo) and the Standards Committee of the SENeo.