Childhood obesity is associated with a high risk of cardiovascular disease and early mortality. This paper summarises the currently available evidence on the implications of dietary factors on the development and prevention of obesity in paediatric patients. Evidence-based recommendations are: promote the consumption of slowly absorbed carbohydrates and reduce those with a high-glycaemic-index, avoid intake of sugar-sweetened beverages. Fat may provide up to 30–35% of the daily energy intake and saturated fat should provide no more than 10% of daily energy intake; reduce cholesterol intake, avoid formula milk with a high protein content during the first year; promote higher fibre content in the diet, reduce sodium intake, and have at least four meals a day, avoiding regular consumption of fast food and snacks.
La obesidad infantil determina un riesgo elevado de enfermedad cardiovascular. Este artículo realiza una actualización sobre el papel que los factores dietéticos tienen sobre el desarrollo y la prevención de la obesidad en este grupo de edad. Según la evidencia científica, las recomendaciones recogidas son: promover el consumo de hidratos de carbono de absorción lenta y disminuir aquellos con índice glucémico alto, evitar el consumo de bebidas azucaradas, limitar el consumo de grasas a un 30% de las calorías totales diarias y el de grasas saturadas a un 7-10%, reducir la ingesta de colesterol, evitar durante el primer año las fórmulas con alto contenido proteico, aumentar la ingesta de fibra, reducir el aporte de sodio y realizar al menos 4 comidas al día evitando el consumo regular de comida rápida y de snacks.
When it comes to the prevention of childhood obesity, there is evidence that interventions consisting of dietary measures result in a mild reduction in body mass index (BMI).1 For this reason, this article of the Obesity Working Group of the Sociedad Española de Endocrinología Pediátrica (Spanish Association of Paediatric Endocrinology) aims at establishing evidence-based recommendations on energy balance, consumption of macro- and micronutrients, and dietary patterns for their application in everyday clinical practice.
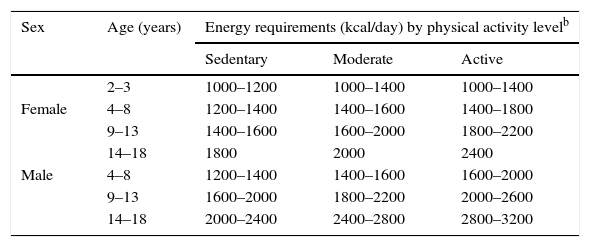
Energy balanceIn the paediatric age group, energy intake must fit the requirements for adequate growth. Energy balance plays an essential role in the development of obesity, and while it is influenced by various factors, these are often difficult to measure.2 Based on equations for estimating calorie requirements, we have estimated energy requirements by age, sex and activity level (Table 1).3 In this regard, a sustained positive energy balance of 70–160kcal/day has been documented in paediatric patients with progressive weight gain, which suggests that small dietary and lifestyle changes would suffice to prevent weight gain in this population.4
Estimated energy requirements for sex, age and activity level.a
| Sex | Age (years) | Energy requirements (kcal/day) by physical activity levelb | ||
|---|---|---|---|---|
| Sedentary | Moderate | Active | ||
| 2–3 | 1000–1200 | 1000–1400 | 1000–1400 | |
| Female | 4–8 | 1200–1400 | 1400–1600 | 1400–1800 |
| 9–13 | 1400–1600 | 1600–2000 | 1800–2200 | |
| 14–18 | 1800 | 2000 | 2400 | |
| Male | 4–8 | 1200–1400 | 1400–1600 | 1600–2000 |
| 9–13 | 1600–2000 | 1800–2200 | 2000–2600 | |
| 14–18 | 2000–2400 | 2400–2800 | 2800–3200 | |
Energy requirements are calculated based on the median for weight and height for each age group and sex.
Sedentary: only the activity associated to day-to-day life. Moderate: activity including the equivalent of walking 2.4–4.8 kilometres (km) a day at a pace of 4.8–6.4km/h in addition to activity associated with day-to-day life. Active: activity including the equivalent of walking 4.8km a day at a pace of 4.8–6.4km/h in addition to activity associated with day-to-day life.
Rapidly absorbed carbohydrates (CHOs) may be associated with adiposity development, whereas slowly absorbed (low-glycaemic index) CHOs are not.2 Thus, it has been observed that a diet rich in low-glycaemic index CHOs can achieve a reduction in waist circumference, HOMA (homeostasis model assessment) indices, BMI and triglyceride levels, and that the decrease in BMI is significantly greater than that achieved with a diet rich in high-glycaemic index CHOs.3 This effect on insulin resistance markers could contribute to reducing the risk of metabolic syndrome in obese children and youth. Similarly, there is evidence that intake of slowly absorbed CHOs is associated with lower concentrations of C-reactive protein (CRP) and interleukin 6,5 both of which are involved in the low-grade inflammation associated with obesity. On the other hand, it has also been observed that rapidly absorbed CHOs produce a lesser satiety than slowly absorbed CHOs in obese as well as normal-weight individuals.6
As for sugary drinks, it has been demonstrated that avoiding their consumption and replacing them with water or sugar-free drinks prevents weight gain in obese individuals, although the effect is very small on their normal-weight peers.7 Furthermore, there is evidence that children that habitually consume sugary drinks between meals have significantly higher weights than children that do not consume them.7
LipidsLipids are the macronutrients that contribute the most to a positive energy balance, as they carry double the energy than the same amount of proteins or CHOs, and the energy cost of storing lipids is a tenth of the cost of storing CHOs or proteins.
Higher consumption of fats in the paediatric age group is associated with increases in body weight and fat mass.2 In the first six months of life, lipids contribute 40–60% of the total calories, and their intake must be reduced gradually between ages 6 months and 3 years,8 after which it is recommended that lipids do not contribute more than 30% of the total calories, restricting saturated fats to 7–10% of the total energy intake and the cholesterol intake to a maximum of 300mg/day.2,8 The remaining 20% of the energy contributed by lipids must come from monounsaturated and polyunsaturated fats, avoiding consumption of trans fats.3 These measures have been associated with a reduction in overall cholesterol, low-density-lipoprotein (LDL) cholesterol, body weight and various insulin resistance markers.9 Similarly, it has been observed that in infants aged 6–12 months, a lower intake of saturated fatty acids combined with an increase in polyunsaturated fatty acids results in lower overall and LDL cholesterol levels, which demonstrates that, even in the first year of life, the amount as well as the quality of dietary lipids have an effect on the serum levels of different lipoproteins.10
The literature also shows that supplementation with linoleic acid in prepubertal children with excess weight decreases weight gain.11 However, the role of the different types of lipids in the development of obesity in children and youth remains unclear, and the safety and efficacy of interventions with medium-chain triglycerides and conjugated linoleic acid in this population needs to be investigated.2
ProteinsExcessive consumption of protein in the first year of life is associated with future weight gain.12 Thus, a study found that infants fed in the first year of life with formulas with a lower protein content had lower BMIs and were at lower risk of obesity at school age, as happens with breastfed infants.13 Recent data for Spain show a protein intake exceeding twice the dietary reference intake in children aged less than 3 years,14 while excess intake of protein as well as CHOs combined with decreased lipid intake is significantly associated with an increase in BMI independent of energy intake.15
Starting at age 2 years, the data on the association between dietary protein intake and weight gain are contradictory. On one hand, a strong positive correlation has been found between high protein intake (>16% of the daily energy intake) and future development of obesity.16 However, other studies show that a high-protein diet is associated with a decrease in fat mass and an increase in lean mass, especially in relation to the amount and combination of arginine and lysine.17
MicronutrientsCalcium and vitamin DDaily calcium requirements vary depending on age: 700mg in children aged 1–3 years, 1000mg between ages 4 and 8 years, and 1300mg between ages 9 and 18 years. When it comes to the association between calcium intake and obesity, the evidence has shown a negative correlation between intake and the development of obesity. Two mechanisms may account for this: on one hand, calcium interferes with the intestinal absorption of fats, and on the other, increased intracellular calcium results in increased lipolysis.18
Studies in adolescents provide scarce data on the association between calcium intake and weight control.19 Moreover, interpreting the results of these studies is difficult, as there are other variables at play, such as dietary control or the association of exercise, and the duration of followup in these studies was short.
The inverse correlation between BMI and vitamin D levels is well known, and the prevalence of vitamin D insufficiency is higher in patients with overweight or obesity compared to normal-weight individuals.20 Although the evidence available to date is not sufficient to establish a direct causal relationship between excess weight and low vitamin D levels, two mechanisms have been proposed to explain their association: on one hand, vitamin D would accumulate in fatty tissues due to its lipophilic nature, and on the other, excess body fat would interfere with its synthesis in a process mediated by leptin.20 Thus, vitamin D levels should be monitored in patients with excess weight in order to ensure adequate dietary intake and sun exposure.20
SodiumThere is evidence that higher sodium intake correlates to greater weight gain in the paediatric age group, especially among females, and this finding is associated with various angiotensin-converting enzyme polymorphisms.21 It is important to note that a higher sodium intake may be associated with higher energy intake, which could be a confounding factor. Furthermore, it has been described that lower dietary sodium intake is associated to lower blood pressure in paediatric patients, so that dietary interventions could be used to address this risk factor for cardiovascular disease.3
IronIron deficiency is associated with an increase in body fat mass and the development of a chronic inflammatory process that may increase the risk of obesity and its complications.22,23 Thus, despite similar iron intakes, obese children have lower serum iron levels. This finding is related to abnormalities in iron absorption that result from the chronic inflammation associated with obesity,23 in which hepcidin plays a key role; hepcidin is an inhibitory factor in intestinal iron absorption mediated by leptin, and its levels are elevated in obese individuals.23 Similarly, an inverse correlation between iron status and insulin and CRP levels has been described in obese children, so that CRP levels could be used as a negative predictor of iron status independent of the BMI.22
MagnesiumThere is evidence that overweight and obese children have lower concentrations of magnesium compared to their normal-weight peers.24,25 Furthermore, an inverse correlation has been established between serum magnesium levels and various cardiovascular risk markers, such as BMI, waist circumference, blood pressure and fasting insulin.24 There is also evidence of decreased dietary magnesium intake in obese children, so increasing magnesium intake may be helpful in preventing the development of insulin resistance and type 2 diabetes mellitus in this population.25
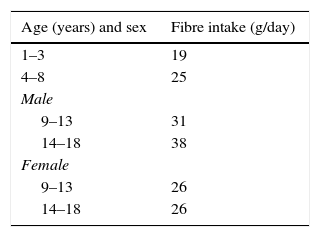
FibreIn the paediatric population, fibre intake has been associated with beneficial effects on weight control: its intake is associated with a decrease in body fat mass, especially abdominal fat.26 On the other hand, in carbohydrate metabolism, insoluble fibre decreases the postprandial glucose concentration and improves insulin sensitivity.26Table 2 gathers the recommendations for fibre intake in children and adolescents.
Recommended fibre intake for ages 2–18 years.
| Age (years) and sex | Fibre intake (g/day) |
|---|---|
| 1–3 | 19 |
| 4–8 | 25 |
| Male | |
| 9–13 | 31 |
| 14–18 | 38 |
| Female | |
| 9–13 | 26 |
| 14–18 | 26 |
An increased number of daily eating occasions may contribute to obesity by promoting excessive energy intake, although the data on this subject are contradictory.27 Most of the data show an inverse correlation between daily number of eating occasions and the risk of obesity, with individuals that have higher eating frequencies also having lower BMI, waist circumference and fasting insulin values despite consuming more calories per day.27 Several hypotheses have been proposed to account for these findings:
- •
An increase in dietary thermogenesis due to increased eating frequency.
- •
A higher meal frequency is associated with decreased hunger and an increased satiety response.28
- •
Frequent eaters may be more likely to have less abdominal fat, as the latter is associated with fasting insulin and triglyceride levels.27
- •
Individuals that eat more frequently tend to be more physically active and make healthier food choices, which may be confounding factors.
Breakfast is defined as the first meal of the day, ingested prior to the initiation of daily activities within 2h of waking up. The number of individuals that skip breakfast has increased in recent years, and regular breakfast consumption decreases with increasing age. Parents play an essential role in the development of healthy dietary habits, and there is evidence that breakfast consumption in parents is positively correlated to breakfast consumption in children.
Some studies have shown an inverse correlation between the frequency of breakfast consumption and BMI in children and adolescents, so that those that skip breakfast would be at higher risk of overweight and obesity.29 Other studies have failed to demonstrate this association after accounting for confounding factors such as physical activity and energy intake, among others.30 Some of the potential beneficial effects of breakfast are:
- •
Higher nutritional quality in food choices for other meals, with higher consumption of fresh produce and fruits.31
- •
A protective effect through improved appetite control and nutrient profiles. Thus, skipping breakfast may be associated with increased hunger later in the day, a higher energy intake or the selection of foods with higher energy density, although the latter is still under debate.32
- •
Beneficial effects on cognitive functioning, as research has found that attention and visual memory decrease when children skip breakfast.33
Recently, some authors have questioned whether breakfast is the most important meal of the day, suggesting that it is just one more meal and introducing concepts such as duration of the overnight fast.34 It has even been proposed that skipping breakfast may have beneficial effects, as intermittent fasting causes periods of ketosis with its associated appetite suppression effect, which may result in a lower energy intake.34 Other studies have analysed breakfast composition, showing that a high-protein breakfast would improve satiety and result in decreased food intake throughout the day through modulation of gastrointestinal hormone secretion.35
Fast food consumptionFast food is easily obtainable food designed for quick preparation and consumption. Although they are not necessarily associated, the concept of fast food is usually synonymous with “junk food”. It is characterised by being served in large portions, a high energy density, a higher saturated and trans fat content, a higher glycaemic index, a lower fibre content and greater palatability, which may lead to increased weight gain.36 The consumption of fast food has increased in recent years due to technological advances in food preparation and storage, the rapid expansion of the fast food industry, and the increased participation of women in the workforce. Most studies conclude that increased consumption of fast food is associated with increased weight gain.36
Meal compositionSnack consumptionA snack is defined as an eating episode during which the food is served in smaller amounts and with a less structured composition than meals. Snacks are usually energy-dense, with a high sugar and fat content and low nutritional value (candy, cookies, salty foods, etc.). Snack consumption has become habitual in children and adolescents, and it is believed to have contributed to the increase in obesity.37 One study found a higher prevalence of overweight and obesity in individuals that consumed three or more snacks a day due to higher energy intake.37 Other authors consider that snacking per se does not predispose to excess weight, as despite the increase in the number of eating occasions the energy intake in each is lower, and the increased eating frequency is associated to a reduction in insulin secretion with the corresponding beneficial metabolic effects.38
As for the timing of snacking, there is evidence supporting that consumption of snacks in the afternoon and evening is associated with an increase in BMI. This finding is related to three factors: the lower dietary thermogenesis due to increased insulin resistance and decreased whole-body fat oxidation in the evening, slower gastric emptying in the evening, and lastly, that evening snacks are frequently consumed in front of the television or at the computer, which is associated with consumption of energy-dense foods.37
Portion sizesPortion sizes have increased in recent years, a trend that has been associated with the increase in the prevalence of overweight and obesity in the paediatric population, although a causal relationship has not been clearly established.39 Most studies conclude that there is a positive correlation between body weight, portion sizes and energy intake.40 While the increase in portion sizes could have a detrimental effect on weight, increasing the size of fruit and vegetable portions may contribute to a higher intake of these healthy foods and a decreased overall energy density of the foods served during meals.
Final recommendationsIn conclusion, having reviewed the scientific literature, the working group would like to emphasise the following aspects:
- •
A diet rich in slowly absorbed carbohydrates with limited intake of carbohydrates with a high glycaemic index must be promoted.
- •
Sugary drinks should be avoided, and consumption of water should be encouraged.
- •
Lipids should not exceed 30% of the total energy intake, and saturated lipids should be limited to 7–10% of the total calories, reducing the intake of cholesterol and avoiding trans fats.
- •
Infant formulas with a high protein content should be avoided in the first year of life.
- •
High sodium intake should be avoided due to the associated risk of obesity and high blood pressure.
- •
A diet rich in fibre should be recommended due to its potential beneficial effects, and specifically for its impact on weight control.
- •
Children aged more than two years should have a minimum of four meals a day.
- •
Breakfast must be encouraged and promoted, with emphasis on adequate composition and nutritional quality.
- •
Fast food should not be consumed on a regular basis.
- •
Consumption of meals at regular hours should be encouraged, and snacks should consist of healthy foods and preferably be consumed in the early hours of the day.
- •
Portion sizes should be appropriate for the age and size of the child. Parents should be informed of appropriate portion sizes through a variety of educational strategies.
The authors have no conflicts of interest to declare.
Please cite this article as: Palomo Atance E, Bahíllo Curieses P, Bueno Lozano G, Feliu Rovira A, Gil-Campos M, Lechuga-Sancho AM, et al. Recomendaciones del Grupo de Trabajo de Obesidad de la Sociedad Española de Endocrinología Pediátrica sobre hábitos de alimentación para la prevención de la obesidad y los factores de riesgo cardiovascular en la infancia. An Pediatr (Barc). 2016;84:178.