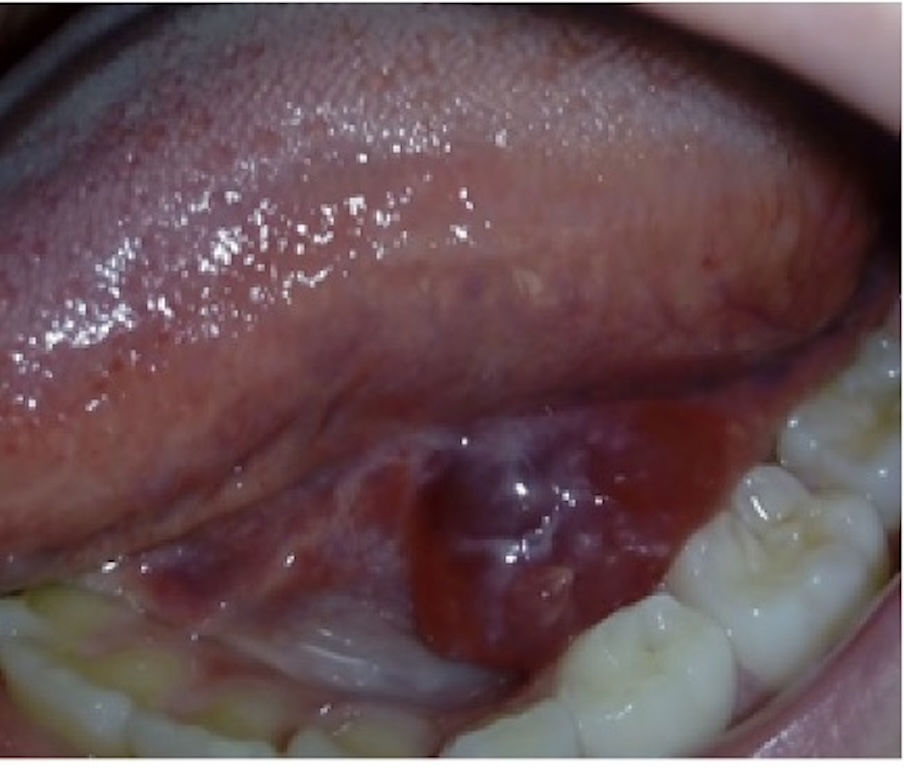
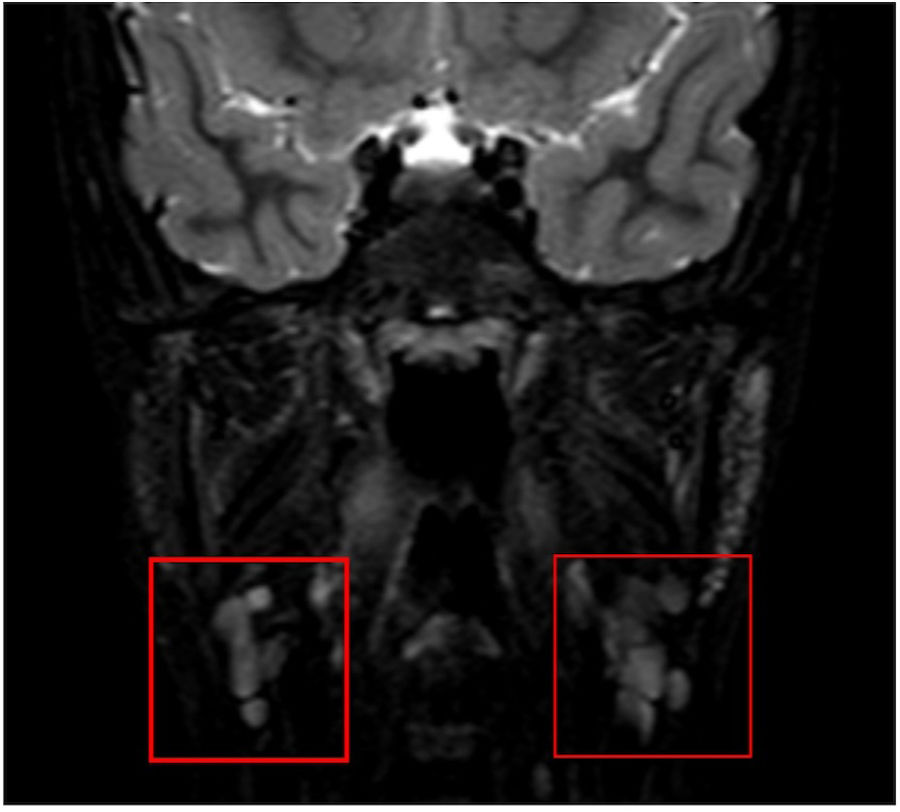
We present the case of a girl aged 9 years referred to our department of pediatric surgery due to recurrent swelling at the base of the tongue with onset five months prior. The examination revealed a fluid-filled tumefaction (Fig. 1). The histopathological assessment confirmed the presence of a unilocular mucous retention cyst with chronic sialadenitis, including acinar atrophy, ductal ectasia and lymphoplasmacytic infiltration. An MRI scan showed bilateral small cysts in the sublingual glands, consistent with simple ranulas, and a multicystic appearance of the parotid glands suggestive of benign lymphoepithelial lesions associated with Sjögren syndrome (SS) (Fig. 2). Laboratory tests revealed elevation of antinuclear antibodies (1:640), high anti-SSA antibody levels (>240 U/mL), and mild elevation of rheumatoid factor (32 IU/mL). Other tests, including serum angiotensin-converting enzyme, protein electrophoresis, immunoglobulin subclasses, complement levels, cryoglobulins, anti-dsDNA, anti-SSB, and anti-U1RNP, were all within normal ranges. The Schirmer test confirmed severely decreased tear production (< 5 mm). The patient later developed sicca syndrome, which improved with symptomatic treatment.
Sjögren syndrome is a rare autoimmune disease in pediatric patients, and its early diagnosis can be challenging. Recurrent ranulas may be an early manifestation of ductal damage in SS.1,2 Therefore, in these cases, imaging of the salivary glands and comprehensive immunological studies should be considered to assess for underlying conditions such as SS.3