Recently, the United Kingdom Health Security Agency warned of an unusual increase in the number of infections by Streptococcus pyogenes in children, which had increased from 186 cases in previous years to 851 cases, predominantly of upper respiratory tract infections, but with an increase in invasive group A streptococcus infections as well. The most frequently reported potentially severe diseases were pneumonia, necrotising fasciitis, sepsis and fulminant septic shock.1 As a result, there has been an increase in the number of paediatric deaths associated with this pathogen.
Acute epiglottitis refers to the inflammation of the epiglottis and adjacent structures, causing abrupt obstruction of the upper airway and constituting a respiratory emergency. Its aetiology is usually infectious, and Haemophilus influenzae type B (HIb) is the most frequent causative agent. However, thanks to the implementation of universal childhood vaccination against HIb, epidemiological trends have changed, and there has been a decrease in the incidence of disease. There have been reports of cases caused by other emerging organisms, such as other H. influenzae types, Staphylococcus aureus, Streptococcus pneumoniae and pyogenes, in addition to some viruses and fungal species.2–4
In this article, we report a case of acute epiglottitis caused by S. pyogenes and review the current literature on the subject.
The patient was a girl aged 7 years with no history of interest and correctly vaccinated that presented to the emergency department with breathing difficulty that had worsened over the past few hours. It was associated with flu-like symptoms, including sore throat and fever of up to 39 °C of one week’s duration. At 48 h from onset, the patient had an influenza B antigen test that turned out positive. On arrival, the paediatric assessment triangle indicated that the patient was unstable and had respiratory failure. In the assessment, the patient was conscious and aware, exhibited maximum use of accessory muscles, a tripod position, sialorrhoea and a nasal voice, with global hypoventilation and stridor and inspiratory and expiratory wheezing.
The patient received supplemental oxygen through a non-rebreather mask. Treatment with salbutamol in continuous nebulization and intravenous steroid therapy was prescribed. The patient was transferred to the paediatric intensive care unit (PICU) to initiate respiratory support with non-invasive ventilation. Intravenous magnesium sulphate, nebulised ipratropium bromide and oseltamivir were added to the treatment. Despite optimal treatment, the severe respiratory distress persisted and the inspiratory wheezing became more pronounced. The suspicion of laryngitis or epiglottitis prompted initiation of treatment with nebulised adrenaline and empirical antibiotherapy with cefotaxime. The plain radiograph of the neck evinced narrowing of the airway. Epiglottitis was suspected, and given the progressive worsening of the patient, the decision was made to intubate her, with observation of a swollen epiglottis. The inserted tracheal tube was two sizes smaller than the size corresponding to her age, and was connected to an invasive mechanical ventilation device, which achieved resolution of respiratory distress.
The complete blood count and chemistry panel revealed leucocytosis with neutrophilia and elevation of acute phase reactants (C-reactive protein [CRP], 159.19 mg/L and procalcitonin [PCT], 100 ng/mL). Later on, S. pyogenes was isolated from cultures of blood and endotracheal aspirate samples. Clindamycin was added to the treatment regimen until the antibiotic susceptibility test results became available. On day 4, an evaluation in the department of otorhinolaryngology revealed that the upper airway continued to be significantly swollen, and the patient remained intubated through day 6, after which she underwent extubation without complications. The patient was discharged after completing 10 days of treatment with intravenous cefotaxime.
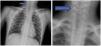
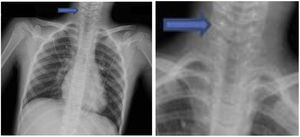
Epiglottitis should be considered in any paediatric patient presenting with acute upper airway obstruction. Anteroposterior radiographs of the neck show a narrowing of the air column known as the “hourglass sign” (Fig. 1) and lateral radiographs show the “thumb sign” produced by the swelling of the airway. Thus, tracheal intubation is one of the measures known to reduce mortality if implemented at an early stage, especially in the paediatric population, compared to watchful waiting. Supraglottic airway management devices, such as laryngeal masks, must be avoided. If intubation is not successful, the patient must undergo an emergency cricothyroidotomy.5
In the case of acute airway obstruction associated with fever, elevation of acute phase reactants and/or manifestations suggestive of sepsis, an infectious bacterial agent should be considered as the primary infectious cause. Given the current increase in the incidence of infection by S. pyogenes, it is important to include it in the initial differential diagnosis.2
The characteristic presentation associated with invasive infection by S. pyogenes is relatively easy to identify: fever with leucocytosis and neutrophilia and/or elevation of acute phase reactants. However, suspecting S. pyogenes as the aetiological agent may be challenging unless the patient exhibits the characteristic scarlatiniform rash. Once S pyogenes is identified, the empirical treatment can be switched to penicillin, with addition of clindamycin in severe cases.6 Given the current increase in the incidence of infection by S pyogenes in children, it is essential to maintain a high level of suspicion.
Conflicts of interestThe authors have no conflicts of interest to declare.