The resuscitation of the newborn in the delivery room requires high capacities and occurs frequently in an unexpected way. Many professionals trained in pediatrics as pediatric residents will work posteriorly in pediatric units with delivery rooms and will perform neonatal resuscitation only occasionally. Skills acquired in practice or resuscitation courses deteriorate over time.
Material and methodsDescriptive observational study through a survey to pediatricians trained in neonatology at a tertiary hospital in Madrid, and who completed their residency period between 2009 and 2016. Questions about their training in resuscitation and their usual work in the delivery room.
ResultsOut of 179 surveys sent, 140 pediatricians (78,2%) answered it. 73.6% took a training course in neonatal resuscitation during the residency. There was a progressive increase in the number of residents who did the course during the study period. 74.3% have worked after residency in assistance at birth. 40.7% have taken a refresher course in neonatal resuscitation.
ConclusionsTraining in neonatal resuscitation has increased and been consolidated during the training process for pediatric residents. A high percentage of pediatricians work after residency in pediatric units with delivery rooms, less than half of these professionals having been recycled in neonatal resuscitation. Recycling and periodic training seem interesting options to improve the performance of these professionals in the delivery room.
La reanimación del recién nacido en sala de partos requiere altas capacidades y se produce con frecuencia de manera inesperada. Muchos profesionales formados en pediatría mediante el método de residencia, trabajarán a posteriori en unidades pediátricas con paritorio y realizarán reanimación neonatal solo de forma ocasional. Las competencias adquiridas en la práctica o los cursos de reanimación se deterioran con el tiempo.
Material y métodosEstudio descriptivo observacional a través de una encuesta a pediatras formados en neonatología de un hospital terciario de Madrid, y que finalizaron su residencia entre los años 2009 y 2016. Preguntas acerca de su formación en reanimación y su trabajo habitual en paritorio.
ResultadosCiento cuarenta pediatras contestaron la encuesta de 179 encuestas enviadas (78,2%). El 73,6% realizó un curso de formación en reanimación neonatal durante la residencia, objetivándose un incremento progresivo en el número de residentes que lo realizaron durante el periodo de estudio. El 74,3% ha trabajado tras la residencia en la asistencia al nacimiento. El 40,7 % ha realizado algún curso de reciclaje en reanimación neonatal.
ConclusionesHa aumentado y se ha consolidado la formación en reanimación neonatal durante el proceso de formación de residentes de pediatría. Un alto porcentaje de pediatras trabajan tras la residencia en unidades pediátricas con paritorio, habiéndose reciclado menos de la mitad de esos profesionales en reanimación neonatal. El reciclaje y el entrenamiento periódico parecen opciones interesantes para mejorar la actuación de estos profesionales en sala de partos.
It is estimated that 10% of newborn infants require some assistance to start breathing at birth1,2 and up to 1% require cardiopulmonary resuscitation (CPR) (chest compressions with or without administration of adrenaline).3 When it comes to preterm infants, nearly 80% of those with birthweights under 1500 g require some form of stabilization or resuscitation to achieve adequate lung recruitment.4,5
Approximately 1 out of 500 neonates require stabilization manoeuvres unexpectedly, so the need for resuscitation is often unpredictable.6 A high-risk birth yielding a seriously compromised infant can occur in any type of hospital, and all professionals involved in labour and delivery must be prepared to stabilize newborn infants.1 Intervention in the first moments of life can affect the survival and outcomes of these infants7 and therefore have a significant impact on the future of these patients and their families.
Several studies have evinced that soon after adequate training in resuscitation there is a decline in the acquired skills,6 which suggests that it may be necessary to offer refresher trainings in the subject at regular intervals.6,7
In Spain, neonatal resuscitation is usually taught as part of the curriculum of medical interns/residents in paediatrics. However, this training is not mandatory and there are no updated guidelines as to how and when it should be delivered and whether regular refresher training is necessary.
Our hospital has been offering neonatal resuscitation training courses since October 2008, but it was not until February 2010 that the courses were accredited by the Sociedad Española de Neonatología (Spanish Society of Neonatology, SENeo) and the Spanish Council of Cardiopulmonary Resuscitation Council through the Spanish Group on paediatric and Neonatal CPR, establishing a standardised training curriculum to be delivered by instructors trained by the Neonatal Resuscitation Group of the SENeo. The residents in paediatrics that were trained in the field of neonatology in our hospital started to participate in these courses in 2011.
Material and methodsObjectives and hypothesisThe primary objective of the study was to analyse the training in neonatal resuscitation of paediatric residents trained in our hospital and to identify how many of them needed to stabilize infants in the delivery room after the training and how many underwent additional accredited neonatal resuscitation trainings. The secondary objective was to assess whether surveyed paediatricians perceived a need for refresher trainings after they completed their medical education. Our hypothesis was that most paediatricians, after finishing their residency period, were at some point involved with the delivery room, despite which initial and refresher trainings on neonatal resuscitation are infrequent.
Study sample and designWe conducted a cross-sectional, observational and descriptive study through a survey of paediatricians that completed their residency in Spain between 2009 and 2016 in our hospital or who received at least part of their training in Neonatology in the Hospital Gregorio Marañón (level III C8) for a period of at least 3 months.
Data collectionWe submitted questionnaires via electronic mail along with information about the study, and data collection adhered to the Organic Law 5/1992 of 29 October on the Regulation of Digital Handling of Personal Identifiable Data. Participants expressly consented to the use of the data for scientific purposes.
SurveyWe developed a questionnaire to collect information on the following:
- –
Residency period: years during which participants were doing their medical residency, hospital of origin, participation in neonatal resuscitation trainings accredited by scientific societies.
- –
Post-residency period (work as paediatrician): involvement in neonatal care at any point; frequency of involvement in neonatal care, answer options: never, occasional (at least 5 times a month), frequent (5–10 times a month) and very frequent (more than 10 times a month); type of manoeuvres performed; current job related to neonatal care; participation in neonatal resuscitation refresher courses.
- –
Perception of the need for regular updating of neonatal resuscitation skills.
We submitted the questionnaires and accepted responses between July and September of 2016. The questionnaire can be found in Appendix 1.
Statistical analysisWe conducted a descriptive analysis of categorical data expressed as absolute frequency and percentage distributions and broken down in groups based on the year of completion of the medical residency period. We analysed the linear trend in the frequency of training courses through time using the chi square test. We considered p-values of less than 0.05 statistically significant with a probability of a type II error of 20%. The statistical analysis was performed with the Stata® software (StataCorp LLC, College Station, Texas, USA).
ResultsIn the period under study, a total of 231 medical residents were trained in paediatrics at the Hospital Gregorio Marañón, of them 149 were residents in the hospital or residents from hospitals that collaborated with Hospital Gregorio Marañón in training in neonatology. The remaining 82 paediatricians were residents from other Spanish hospitals on away rotations.
We contacted a total of 183 paediatricians via electronic mail. Four candidates did not receive the email or the questionnaire due to an automated error of the email system. Of the 179 paediatricians that received the questionnaire, 140 submitted responses (78.2%).
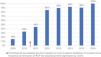
Table 1 summarises the results of the survey pertaining to participation in neonatal resuscitation trainings both during the residency and after. Of all respondents, 103 (73.6%) participated in a neonatal resuscitation training accredited by the SENeo during the residency. The percentage of paediatricians that participated in such a training during the residency increased as years went by, as can be seen in Fig. 1. The increase in CPR training during the period under study was statistically significant (Mantel–Haenszel chi = 44.88; P < 0.01).
Participation in neonatal resuscitation trainings by year of residency completion.
| Year of residency completion | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | Total |
|---|---|---|---|---|---|---|---|---|---|
| Respondents, n (% total surveyed) | 13 (9.3%) | 12 (8.6%) | 18 (12.8%) | 13 (9.3%) | 19 (13.6%) | 26 (18.6%) | 21 (15%) | 18 (12.8%) | 140 (100%) |
| CPR training during residency, n (% total in year group) | 2 (15.4%) | 4 (33.3%) | 8 (44.4%) | 11 (84.6%) | 17 (89.5%) | 24 (92.3%) | 19 (90.4%) | 18 (100%) | 103 (73.6%) |
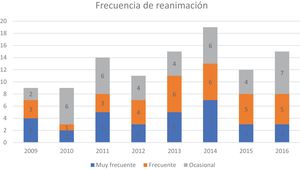
After completing the residency, 104 of the 140 respondents (74.3%) had worked in settings where they managed births on a regular basis (Table 2). The percentages that had performed some form of stabilization or resuscitation manoeuvres in the delivery room were: 37% occasionally, 32% frequently and 31% very frequently (Fig. 2). As for the required manoeuvres, 6.5% reported they only needed to administer continuous positive airway pressure (CPAP), while 25% reported use of ventilation with positive end-expiratory pressure (PEEP), 23% endotracheal intubation and 45% chest compressions with or without administration of adrenaline (Fig. 3).
Need to perform resuscitation after the residency.
| Year of residency completion | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | Total |
|---|---|---|---|---|---|---|---|---|---|
| Total respondents | 13 (9.3%) | 12 (8.6%) | 18 (12.8%) | 13 (9.3%) | 19 (13.6%) | 26 (18.6%) | 21 (15%) | 18 (12.8%) | 140 (100%) |
| CPR training post residency (% total in year group) | 5 (38.4%) | 9 (75%) | 9 (50%) | 7 (53.8%) | 10 (52.6%) | 11 (42.3%) | 4 (19%) | 2 (11.1%) | 57 (40.7%) |
| Performed resuscitation after completing residency | 9 (69.2%) | 9 (75%) | 14 (77.8%) | 11 (84.6%) | 15 (78.9%) | 19 (73%) | 12 (57.1%) | 15 (83%) | 104 (74.3%) |
Of all respondents to the survey, 53.6% reported that their clinical practice was related to neonatal and maternity care at the time of the survey.
Fifty-seven paediatricians (40.7%) reported participating in neonatal resuscitation courses after the residency (Fig. 4). Of all paediatricians that had received CPR training during the residency, 41 (39.8%) participated in a refresher training after completing the residency.
When it came to the perceived need of training in resuscitation, 99.3% of paediatricians agreed that refresher courses were necessary after completing the residency, and only 1 paediatrician responded answered that refresher trainings were not necessary.
DiscussionTo our knowledge, based on a review of the literature, there have not been recent studies conducted in Spain analysing training on neonatal resuscitation during or after the residency in paediatrics. We also did not find data on the proportion of paediatricians that needed to perform resuscitation manoeuvres in clinical practice after completing their medical education.
The findings obtained from analysing the responses of 140 paediatricians support our hypothesis, since 74.3% of paediatricians reported carrying out neonatal resuscitation in the delivery room, many only occasionally (37%) and others as part of their regular clinical practice. Another outstanding finding was that a large percentage of paediatricians had to use advanced life support measures for infant stabilization (45% of those who reported engaging in resuscitation), measures that are rarely used in the delivery room and that require a clear understanding of the CPR sequence in addition to adequate skill in leading and coordinating its implementation.
These findings confirm the relevance and need of accredited training not only during the medical education and residency period, but also later, and regular training through refresher courses is a good approach for the purpose of reinforcing the knowledge, skills and teamwork required for adequate resuscitation.
Previous studies have shown that theoretical knowledge and practical skills in neonatal resuscitation deteriorate rapidly when they are not put into practice, and every author suggests the need of refresher trainings at regular intervals, especially in individuals that only engage in resuscitation occasionally.1,5,9–17
Neonatal care is a high-acuity speciality that requires competence in clinical decision-making and complex procedures. This can make training in this field challenging and stressful.18 Early delivery of high-quality CPR is one of the most important predictors of survival and future sequelae in any victim of cardiopulmonary arrest.19,20
Historically, resuscitation in the delivery room was based on the subjective judgment of the rescuer rather than rigorous scientific evidence, and there was little technical innovation that could improve care.9 At present, consensus guidelines and recommendations on neonatal CPR are updated periodically. The International Liaison Committee on Resuscitation (ILCOR) meets every 5 years to publish neonatal resuscitation clinical practice guidelines.9,21,22 In Spain, the ILCOR guidelines are subsequently reviewed, debated and published by the Neonatal CPR group of the SENeo in a consensus-based process that yields a manual and several other publications.4,23
According to the guidelines for neonatal resuscitation programmes, training of medical staff improves the outcomes of resuscitation at birth, increasing the implementation of evidence-based measures and reducing the use of potentially harmful traditional measures.10,24,25 Practicing resuscitation skills regularly is important for reliable and optimal neonatal care delivery.1,9 Health care staff that perform CPR, receive feedback and undergo training frequently achieve better outcomes, although the skills vary between individuals.1 A Cochrane review from 201511 found that standardised formal resuscitation training programmes, compared to basic newborn care or basic neonatal resuscitation achieved a reduction in early neonatal and 28-day mortality in developing countries.
In Spain, training in neonatal resuscitation is not mandatory, nor is subsequent periodic retraining in refresher courses. The official state bulletin (BOE) of 14 October 2006 published the text of Regulation SCO/3148/2006 of September 20th, on presented the official educational curriculum for the speciality of paediatrics and its subspecialities and announced its approval, and the section that outlined the contents of the curriculum included training on neonatal resuscitation, although it did not specifically mandate participation in formal and accredited courses on the subject.
We believe that neonatal resuscitation is a crucial element in the education of paediatricians and their future clinical practice, so we decided to analyse trends in neonatal resuscitation in the residency period.
The increased frequency of neonatal CPR training in the paediatrics residency observed through the years may be due to the growing importance attributed to this content by the faculty with the introduction of neonatal resuscitation trainings accredited by the SENeo in our hospital in 2011, the interest of residents themselves in receiving training in this area and institutional development of measures to improve patient safety and assess quality of care. The introduction of an ongoing education programme in any field promotes development of consensus-based training curricula held to quality standards and the equally important development of standard criteria that lead to improvements in morbidity, mortality and patient outcomes while reducing health care costs related to preventable diseases or complications.
Since 2011, our unit has been gradually introducing full courses in basic and advanced neonatal resuscitation accredited by the SENeo for paediatrics residents training in neonatology in our hospital. As a result, since 2013 > 90% of these residents have completed accredited trainings. In recent years, the institutional bodies responsible for the residency programme have been giving more importance to resuscitation training courses.
There is evidence that the theoretical knowledge and practical skills acquired in resuscitation trainings deteriorate over time.10 As would be expected, this decline is particularly marked in individuals that do not practice resuscitation on a regular basis. Some studies have found that this decline starts 3 months26 after the initial training, although other studies detected it after 6–12 months.6 Mosley and Shaw12 assessed whether students retained the airway management and ventilation skills taught in neonatal resuscitation courses after their successful completion, and found that these skills started to deteriorate a few months after completion of training. Duran et al.27 found that intubation skills had declined significantly 1 year after completing the training. Kovacs et al.28 found that airway management skills declined rapidly after the initial training and that practice by means of simulation combined with feedback at regular intervals were effective for maintenance of advanced airway management skills.
The retention of theoretical knowledge, assessed with instruments like the tests published by the American Heart Association, seems better compared to the rapid decline of practical skills.12–14 In a prospective study conducted in residents in paediatrics, Patel et al.29 evidenced this discrepancy in the decline of theoretical knowledge versus practical skills, suggesting that competence in one of these areas does not necessarily entail competence in the other.
There is also evidence that refresher training and reassessment of CPR competence 6 months after a training significantly improves retention of knowledge and skills.15 Establishing the minimum frequency of trainings required to maintain adequate competence in CPR would be beneficial.17 In a study designed to assess the effect of different time intervals between regular trainings on the retention of basic CPR skills, Berden et al.17 found that skill retention remained stable through regular refresher trainings at 3- or 6-month intervals, suggesting that trainings at 12-month intervals are not frequent enough.
González Inciarte et al.16 recommended an annual refresher after conducting a study about paediatric CPR in residents in paediatrics. Based on their findings, the authors concluded that efforts should be made to ensure that staff is qualified to perform resuscitation and that training on the subject should be mandatory for every health care professional. However, at present there is no consensus, in Spain or internationally, on whether refresher trainings are necessary or what their frequency should be. In the United Kingdom, health care professionals involved in neonatal resuscitation had to be recertified every 4 years (United Kingdom Resuscitation Council).6
Recommendations notwithstanding, only 40.7% of respondents reported having received training on resuscitation after completing the residency, even though the vast majority of surveyed paediatricians agreed on the importance of reinforcing neonatal resuscitation knowledge and skills through refresher trainings.
The objectives of neonatal resuscitation courses are to facilitate the dissemination of standardised recommendations accepted at the international level, optimising clinical practices in neonatal resuscitation and acquisition of technical skills to minimise the risk to patients.4,12 A survey conducted in hospitals of all levels in Spain found significant improvements both in equipment and in the stabilization measures used in the delivery room, in adherence with international guidelines, following the nationwide introduction of a policy for training in neonatal CPR.30
A key characteristic of CPR courses is that they also teach and reinforce care coordination and teamwork, which are essential elements in real-world resuscitation.12,25
There are several limitations to our study. First, we did not establish a quantitative definition of “very frequently”, “frequently”, “occasionally” for answering the question whether respondents had performed CPR after completing the residency. We tried to remedy this limitation a posteriori by asking respondents again and providing specific numbers for each of these categories, but only 39% of participants responded to this new query. Another aspect to consider is that the study was conducted in a single hospital, which carries a risk of selection bias, although it is should also be taken into account that the hospital trains residents that come from the entire Spanish territory.
ConclusionWe believe that training in neonatal resuscitation is essential not only during the medical residency, but also thereafter, as many paediatricians are involved in maternity care and need to perform resuscitation in the delivery room. Given that the need for resuscitation in the delivery room can be unpredictable, crucial and stressful, training in neonatal resuscitation is essential not only during the medical residency but also later on, as many clinicians may have contact with the delivery room and need to perform resuscitation measures. Since the need for resuscitation may be unpredictable, crucial and stressful, especially for clinicians that only perform CPR occasionally, regular training and updating of skills may be a beneficial approach to improve performance. Changes in regulations regarding initial training and continuing education would be useful to pursue the goal of making them mandatory and ensuring their funding within medical education, both as part of the residency curriculum and thereafter.
Our study may serve as a stepping stone towards a larger analysis at the national level to assess the current situation of accredited training in neonatal resuscitation in the residency period and the subsequent involvement of paediatricians in neonatal care and the need for periodical updating of skills.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Pescador Chamorro MI, Zeballos Sarrato SE, Marsinyach Ros MI, Zeballos Sarrato G, Márquez Isidro EM, Sánchez Luna M. Formación, experiencia y necesidad de reciclaje en reanimación neonatal. Encuesta a pediatras. An Pediatr (Barc). 2022;96:122–129.
Previous presentation: The study was presented at the XXVI Congress of Neonatology and Perinatal Medicine; September 27–29, 2017; Zaragoza, Spain.