Junctional ectopic tachycardia (JET) is one of the most frequent arrhythmias that develop after surgical intervention of congenital heart disease. It is characterised by abnormal automaticity within the auriculoventricular (AV) node manifesting as narrow QRS tachycardia, usually associated with AV dissociation and haemodynamic instability. Conventional management consists of the rational use of inotropes, moderate hypothermia, correction of electrolyte abnormalities, optimization of sedation/analgesia, restoration of atrioventricular synchrony with a pacemaker and antiarrhythmic drugs. In general, treatment protocols include amiodarone as the first-line drug.1 In refractory cases, a second drug may need to be added and, in some cases, low cardiac output may require support with extracorporeal membrane oxygenation (ECMO).
Ivabradine is a drug that acts on the I(f) (“funny”) current by blocking hyperpolarization-activated cyclic nucleotide-gated (HCN) channels at the sinus and AV nodes,2 reducing their intrinsic automaticity and without a negative inotropic effect. It has been used successfully for treatment of inappropriate sinus tachycardia and of patients with dilated cardiomyopathy and chronic heart failure resistant to beta-blockers. It has also proven effective for treatment of congenital JET,3,4 although the evidence on its use for refractory postoperative JET is scarce.5,6
We present 3 cases that illustrate the efficacy ivabradine for treatment of postoperative JET refractory to conventional treatment. Table 1 presents the characteristics of these cases. Implementation of conventional treatment measures, including antiarrhythmic therapy (amiodarone in all cases, combined with esmolol in one), failed to bring the heart rate (HR) below 170 bpm, which prevented restoration of atrioventricular synchrony with a pacemaker. Ivabradine, delivered through a nasogastric tube, was added at a dose of 0.1 mg/kg/12 h in the context of sustained haemodynamic instability. We defined haemodynamic instability as tissue hypoperfusion despite an increase in the vasoactive-inotropic score and/or volume expansion. It was considered “sustained” when it lasted more than 4 h past the onset of JET (during which the loading dose of amiodarone was administered to prevent adverse events). In a mean time of 180 min following the loading dose, the HR had decreased to a mean of 145 bpm, which allowed restoring atrioventricular synchrony through AV pacing. After implementation these measures, there was a clear improvement in cardiac output. Treatment with ivabradine continued for a mean of 3.3 days, with a mean time elapsed to conversion to sinus rhythm of 64 h. We did not observe any significant adverse effects in any of the patients.
Characteristics of the patients that received ivabradine for management of JET.
| Patient 1 | Patient 2 | Patient 3 | |
|---|---|---|---|
| Age at onset of JET (m) | 2.5 | 5 | 5.6 |
| Reason for admission | Cardiac surgery with ECC | Cardiac surgery with ECC | Cardiac surgery with ECC |
| Cardiological diagnosis | Heterotaxia, right isomerism. Complete unbalanced AV septal defect with mitral atresia, hypoplastic left heart, double outlet right ventricle, pulmonary atresia, non-confluent pulmonary arteries with origin at BCT and aortic arch | Complete AV septal defect | ASD, VSD, pulmonary valve stenosis |
| Surgery | Aortic valve valvuloplasty, unifocalization of pulmonary arteries. EXIT to ECMO due to severe ventricular failure | Complete repair | Complete AV septal defect |
| Onset of JET | Immediate | Immediate | Complete repair |
| Maximum HR (bpm) | 210 | 220 | 200 |
| HR after initiation of ivabradine (bpm) | 120 | 160 | 160 |
| Time to significant decrease of HR (min) | 240 | 60 | 180 |
| Time to conversion to sinus rhythm (h) | 48 | 48 | 96 |
| Inotropic support at initiation of JET (µg/kg/min) | Epinephrine 0.05 | Epinephrine 0.05 | Epinephrine 0.05 |
| Milrinone 0.6 | Milrinone 0.6 | Dopamine 6 | |
| Norepinephrine 0.1 | Milrinone 0,6 | ||
| Antiarrhythmic treatment and general supportive measures prior to ivabradine | Amiodarone 5 mg/kg | Amiodarone 5 mg/kg | Amiodarone 5 mg/kg |
| Esmolol 250 µg/kg/min | Reduction in vasoactive drugs | Reduction in vasoactive drugs | |
| Reduction in vasoactive drugs | Cooling (34.5°) | Cooling (34°) | |
| Cooling (34°) | Deep sedation | Deep sedation | |
| Deep sedation | Neuromuscular blockade | Neuromuscular blockade | |
| Neuromuscular blockade | |||
| Duration of ivabradine (d) | 3 | 4 | 3 |
| Initial dose of ivabradine (mg/kg/12 h) | 0.1 | 0.1 | 0.1 |
| Adverse effects | None | None | None |
ASD, atrial septal defect; AV, atrioventricular; BCT, brachiocephalic trunk; bpm, beats per minute; d, days; ECC, extracorporeal circulation; ECMO, extracorporeal membrane oxygenation; h, hours; HR, heart rate; JET, junctional ectopic tachycardia; min, minutes; PM, pacemaker; VSD, ventricular septal defect.
Since ivabradine acts on the pathogenic mechanism of postoperative JET, it may be an effective therapeutic option for management of JET refractory to conventional antiarrhythmic drugs. There is ample experience on its use in adults and the evidence of its use in children is growing. Despite the potential limitation in critical patients of the exclusive enteral route of administration, our experience shows that it can achieve an effective reduction in HR in a mean time of less than 180 min (range described in the literature: 50–300 min).5 Although the initial dose of ivabradine is not well established for the paediatric population, the current literature suggests starting with a dose of 0.05 mg/kg/12 h,3,5 and the maximum reported dose of 0.14 mg/kg/12 h. Sinus bradycardia is the most widely documented adverse event associated with ivabradine, a condition that can be easily treated in the immediate postoperative period with temporary epicardial pacing. Due to its potential to prolong the QT interval, especially in association with other drugs, it is important to perform ECGs at regular intervals.
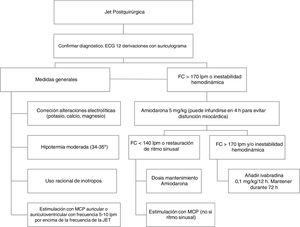
Although our experience in the use of ivabradine in this context is limited, we believe that it may be a safe and effective treatment option due to its rapid action and few adverse effects. For this reason, we recommend its early administration for treatment of refractory postoperative JET (Fig. 1), titrating the dose based on the clinical response, tolerability and QTc.
Please cite this article as: López Fernández E, Montañes Delmas E, Granados Ruiz MÁ, Oviedo Melgares L, Ramos Casado V. Uso de ivabradina en el tratamiento de la taquicardia ectópica de la unión tras cirugía cardiaca. An Pediatr (Barc). 2021;95:118–120.