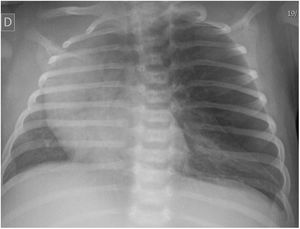
A neonate was referred to our hospital at 13 days post birth for assessment of dyspnoea. In the referring hospital, the complete blood count results had been normal, while the blood gas analysis revealed respiratory acidosis and the chest radiograph findings (Fig. 1) were compatible with pneumothorax.
However, the physical examination did not evince the expected severity, finding a mild increase in the work of breathing and cyanotic spells limited to intense crying.
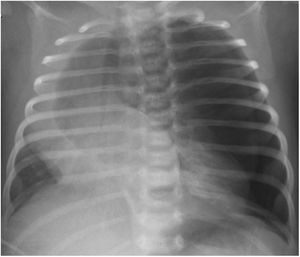
After drainage, the condition of the infant worsened abruptly with shifted cardiac sounds and marked hypoventilation of the affected hemithorax. A new chest radiograph (Fig. 2) detected a tension pneumothorax in addition to the pre-existing lesion.
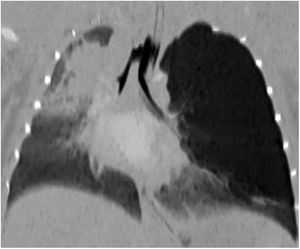
The change in the patient’s condition prompted the performance of a computed tomography scan (Fig. 3; Appendix B, video 1), which resulted in the definitive diagnosis of congenital lobar emphysema.
At the time of this writing, after undergoing lobectomy via thoracotomy in the department of paediatric surgery, the patient is asymptomatic, and the check-ups performed to date have evinced normal development.
Congenital lobar emphysema is an infrequent disease caused by alterations in lung development that result in air trapping through a “ball-valve” mechanism.1
At the time of diagnosis, it is common to mistake congenital lobar emphysema with pneumothorax,2,3 so it is important to take the former into account in the differential diagnosis and perform additional tests as needed. Although the sonographic features of this disease have yet to be established, a lung ultrasound scan could have been useful in this case, as it would not have shown the characteristic pattern of pneumothorax.
Previous meeting: this case was presented at the Spring Meeting of the Sociedad de Pediatría de Asturias, Cantabria y Castilla y León (SCCALP); April 29-30, 2022; Avilés, Spain.