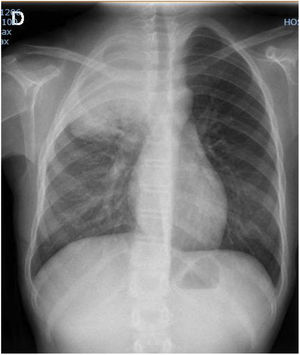
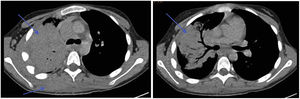
We present the case of a female patient aged 11 years, previously healthy, who presented with an interscapular mass, right-sided omalgia and constitutional syndrome of 6 months’ duration.1 The salient findings of the complete blood panel were leucocytosis with left shift and elevation of the erythrocyte sedimentation rate (ESR) and lactate dehydrogenase (LDH). The imaging evaluation confirmed a pulmonary pseudotumour extending beyond the lung with lung consolidation (Fig. 1, X-ray; Fig. 2, CT scan).
Chest CT scan. Lung consolidation in apical and posterior segments of the right upper lobe with central air bronchogram and peripheral hepatization. Moderate lymph node enlargement in the right paratracheal, right hilum and subcarinal regions. Diffuse enlargement of soft tissues with poorly defined borders involving the apical and posterior wall of the right hemithorax, traversing the intercostal spaces and extending into the right paraspinal musculature.
The evaluation continued with fibreoptic bronchoscopy and bronchoalveolar lavage, which ruled out endobronchial lesions. The Mantoux and serology tests were negative. Examination of a biopsy of the extrapulmonary lesion evinced proliferation of fibrohistiocytic cells, without atypia, suggestive of an inflammatory or granulomatous disease or pseudotumour.
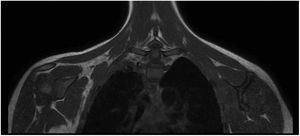
A 28-day course of empiric antibiotherapy (cefotaxime and cloxacillin)2 achieved resolution of the mass. The follow-up radiological evaluation, at 8 months (Fig. 3, MRI) evinced marked radiological improvement with residual pseudotumour tissue, rather than fibrotic tissue or scarring, in the right apical pleura and the posterior musculature of the upper right thorax. The patient was asymptomatic and the lung function tests were normal.
Inflammatory myofibroblastic tumour is usually treated with surgical resection,3 although in some cases the lesion stabilises or even regresses, as was the case of our patient. In other cases, the mass becomes invasive at the local level and requires other treatments, such as steroid therapy, radiation or chemotherapy.
FundingThis research did not receive any external funding.
Conflicts of interestThe authors have no conflicts of interest to declare.