An infant born at 34 weeks and weight adequate for gestational age, without risk of infection, presented with a generalized vesicular rash (Fig. 1), negative for Nikolsky’s sign, with involvement of genitals, palms, soles (Fig. 2) and oral mucosa.
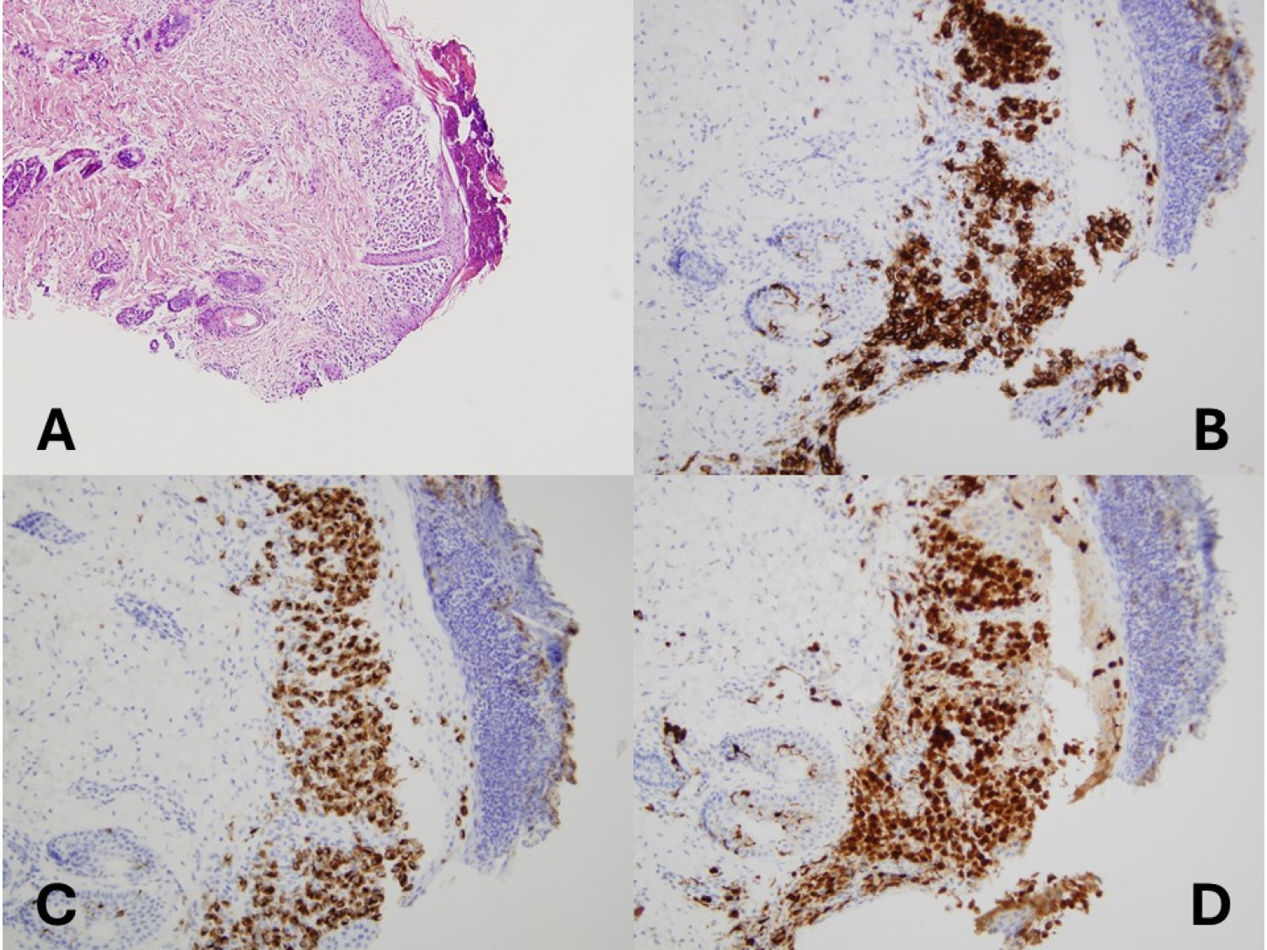
Due to suspicion of infection (TORCH syndrome) or an autoimmune etiology (pemphigus, epidermolysis bullosa), antibacterial, antifungal and antiviral therapy was initiated until the results of culture turned out negative. The results of the biopsy examination led to diagnosis of Langerhans cell histiocytosis, while molecular testing was negative for BRAF variants.
The workup did not evince any form of extracutaneous involvement.
Langerhans cell histiocytosis is a disease with a broad clinical spectrum that can affect a single organ or manifest with multisystemic involvement.1
The diagnosis is histological and based on the presence of an inflammatory infiltrate with abnormal Langerhans cells (CD1a+, S100+, CD207+) (Fig. 3A–D). The presence of the BRAF variant is associated with the most aggressive forms of disease, with an increased risk of refractory disease and disease reactivation.
Clinical suspicion of this disorder is important in neonates presenting with cutaneous involvement, as was the case of our patient, due to its therapeutic and prognostic implications.2,3 In cases that resolve spontaneously or with exclusive cutaneous involvement, the treatment is symptomatic, while cases with systemic involvement require chemotherapy.
In this case, the patient has not received any form of systemic treatment to date, with the exception of one instance of hospital admission for systemic antibiotherapy due to the potential superinfection of skin lesions that continue to progress in the form of outbreaks in absence of extracutaneous involvement.