Tracheotomy in paediatric patients is a rare procedure. In this paediatric series, perioperative complications, mortality related to surgical procedure and overall mortality are analysed.
Patients and methodsThis is a retrospective study conducted from January 2003 to December 2013. Data were retrieved from patients who were tracheotomized and admitted to our PICU in the postoperative period.
ResultsData were collected from 25 tracheotomized patients admitted during the study period. The mean age was 31.3 months (median 14 months, range 1–144 months), and PICU length of stay was 53 days (median 37 days, range 1–338 days). Most patients (68%) had comorbidities prior to admission, with a higher prevalence of craniofacial anomalies/polymalformative syndromes (32%) and prematurity related disorders (12%) being observed. The most common aetiologies related to the procedure were congenital airway obstruction (16%) and several types of spinal cord injury (16%), followed by tracheobronchomalacia (12%) and subglottic stenosis (12%). Complications were detected in 40% of patients, with accidental decannulation being the most frequent. Accidental or unexpected decannulation occurred was present in as many as 20% of our patients, mainly in the first 24h after surgery. One patient died as a result.
ConclusionsThe postoperative course of a tracheotomy is associated with a high rate of complications, some of them related to life-threatening events.
La traqueotomía es un procedimiento poco frecuente en la Unidad de cuidados intensivos pediátricos (UCIP). Analizamos las complicaciones derivadas de la técnica, la mortalidad atribuible a la misma y la mortalidad global de los pacientes traqueotomizados.
Pacientes y métodosEstudio retrospectivo descriptivo durante el periodo comprendido entre enero del 2003 y diciembre del 2013 de los pacientes ingresados en la UCIP a los que se realiza una traqueotomía a lo largo de su ingreso.
ResultadosDurante el periodo analizado se recoge a 25 pacientes. La media de edad es de 31,3 meses (rango 1-144, mediana 14 meses) y la media de estancia en UCIP es de 53 días (rango 1-338 días, mediana 37 días). En su mayoría (68%) son pacientes con comorbilidades previas a su ingreso, destacando en frecuencia las anomalías craneofaciales/síndromes polimalformativos (32%) y problemas asociados a la prematuridad (12%). Las patologías más frecuentes que motivaron la realización del procedimiento fueron la obstrucción congénita de la vía aérea y diversas causas de lesión medular, seguido de traqueobroncomalacia y estenosis subglótica. Se detectaron complicaciones en el 40% de los pacientes, siendo la más frecuente la decanulación accidental. Presentaron durante el curso evolutivo una decanulación accidental el 20% de los pacientes, principalmente en las primeras 24h del postoperatorio, motivo por el que falleció uno de los pacientes.
ConclusionesLa realización de la traqueotomía es un procedimiento poco frecuente en la UCIP, aunque no exento de complicaciones, algunas de ellas de riesgo vital.
Tracheotomies are rarely performed in the Paediatric Intensive Care Unit.1 This technique is performed in the paediatric patient noticeably less frequently than in adults, where up to 10% of all patients who receive mechanical ventilation (MV) are tracheotomised.2 Over time, common indications for MV, such as the infectious acute inflammation of the airway, have now been replaced with others, such as MV dependency in chronic patients, severe airway obstruction due to congenital malformations, and thoracic wall weakness in neuromuscular patients.3–5 MV, therefore, is now used in both acute and chronic patients discharged with some kind of home respiratory support.
The complication rate associated with this technique is considered to be higher in children than in adults.6–8 However, both the frequency and type of complication, above all mortality, vary considerably between studies. Mahadevan et al.9 describe a global complications rate in these patients of 51%, with 2.5% of accidental decannulations, percentages that are similar to those found in other publications.10–12 Mortality directly attributable to MV ranges from 0.5% to 3% in different series, the most frequent causes being accidental decannulation and obstruction of the cannula.10,12–14 Global mortality of tracheotomised patients ranges from 7% to 40%, depending on the study.4,9,14
The purpose of this review is to analyse the tracheotomies performed in our unit in order to gain insight into the complications derived from the technique, the mortality attributable to it and the global mortality of tracheotomised patients. The purpose is also to compare our findings with those published in the most recent literature. The study was approved by the institutional review board of the Cruces University Hospital (Bilbao, Spain).
Patients and methodsWe conducted a retrospective chart review of patients admitted to the Paediatric Intensive Care Unit (PICU) of the Cruces University Hospital that underwent tracheotomy in the unit in the period between January 2003 and December 2014.
The patients were chosen after reviewing the records of patients discharged from the unit, selecting those whose diagnosis and/or techniques performed during admission showed a tracheotomy within the period covered by the study. In total, 26 patients were identified. One patient was excluded because his medical history was not available. The patients were included in the review, regardless of whether the procedure was urgent or elective and of the surgical technique used for placing and fixing the cannula.
The following variables were analysed – indication for tracheotomy, age, MV days prior to the tracheotomy, length of stay in the PICU, types of cannula (cuffed or simple) postoperative day for the first scheduled cannula replacement, and complications directly related to this procedure, mortality related to the technique and global mortality.
We also analysed a subgroup of patients with an episode of accidental removal of the tracheotomy cannula (accidental decannulation) with the purpose of finding possible differential factors in this subgroup with respect to the total.
Being a retrospective, non-interventionist study, informed consent was not requested from the parents/guardians.
For the statistical study, the Mann–Whitney eliminar test was used for independent samples. Data were analysed using IBM SPSS statistics (version 22.0).
ResultsPatients and indicationsDuring the 10-year study period, near 6000 patients have been admitted to the Unit, of which 30% received MV. Approximately 1500 were intubated and 25 of those underwent tracheotomy, which constitutes 1.5% of the intubated patients. Out of the 25 patients included in our series, 13 were boys (52%) and 12 girls (48%). The mean age was 31.3 months (median: 14 months, range: 0–12 years), 44% them were under the age of 1 year and 76% under the age of 3 years.
Airway obstruction was the most frequent indication for tracheotomy, 14 (56%) of the patients, while prolonged MV was the indication for tracheotomy in the remaining patients, 11 (44%).
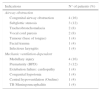
The different causes, divided in subgroups, are shown in Table 1.
Indications of tracheotomy.
| Indications | N° of patients (%) |
|---|---|
| Airway obstruction | |
| Congenital airway obstruction | 4 (16) |
| Subglottic stenosis | 3 (12) |
| Tracheobronchomalacia | 2 (8) |
| Vocal cord paresis | 2 (8) |
| Tumour (base of tongue) | 1 (4) |
| Facial trauma | 1 (4) |
| Infectious laryngitis | 1 (4) |
| Mechanic ventilation-dependent | |
| Medullary injury | 4 (16) |
| Prematurity (BPD) | 3 (12) |
| Extubation failure: cardiopathy | 1 (4) |
| Congenital hypotonia | 1 (4) |
| Central hypoventilation (Ondine) | 1 (4) |
| TB Meningoencephalitis | 1 (4) |
BPD: bronchopulmonary dysplasia; TB: tuberculosis.
Among the cases of airway obstruction, 4 (16%) were due to congenital factors (Pierre–Robin sequence, CHARGE syndrome, congenital microretrognathia without identification, Proteus syndrome), 3 due to post-MV subglottic stenosis, 2 presented severe tracheobronchomalacia uncontrolled with medical (continuous positive pressure in the airway) or surgical (aortopexy) treatment, 2 presented vocal cord paresis (one congenital, one post-MV), 1 base tongue tumour, one facial trauma, and 1 case secondary to obstruction due to infectious inflammation of the airway (laryngitis).
Among the cases of prolonged MV, 4 were secondary to medullary injury (1 poly-trauma, 1 intramedullary tumour, 1 posterior fossa decompressive post-neurosurgery ischaemic injury and 1 transversal myelitis), 3 cases of bronchopulmonary dysplasia, 1 cardiopathy with recurrent failures in extubation, 1 case of congenital hypotonia with respiratory failure, 1 case of Ondine's syndrome and 1 patient with tuberculous meningitis and MV-dependent severe brain injury.
As to the characteristics of the tracheotomy cannulas, 20% of them were cuffed. The first scheduled replacement was performed on the seventh postoperative day in most cases (92%), and the reason why the procedure was not performed on the seventh day in the other episodes is unspecified. In all cases, the first replacement was performed by an otolaryngologist.
The mean stay at the PICU for these patients was prolonged (53 days, median: 37, range: 1–338), given their chronic condition. Mean days on MV prior to ostomy was 48 days (range: 0–270).
Twenty-four tracheotomies were performed electively in the operating theatre; 1 was an emergency procedure in an otherwise healthy girl with symptoms of infectious laryngitis, due to intubation failure in the hospital of origin. None of the tracheotomies were performed percutaneously.
ComplicationsTen patients (40%) presented complications related to the tracheotomy procedure during their stay in the PICU (Table 2), 2 of them presenting more than 1 complication.
As for mild complications, 3 patients showed local infections resolved with treatment, and 1 presented stoma granuloma. No bleeding or significant neck wound from tube attachments were observed. Among the severe complications, 5 patients presented an episode of accidental decannulation, 3 presented air leak syndrome (pneumothorax/pneumomediastinum), 1 presented obstruction of the cannula and 1 died. The deceased patient died in the immediate postoperative period as a result of accidental decannulation with impossibility of recannulation.
Mortality attributable to tracheotomy complications was 4% (1 patient died due to accidental decannulation), while global mortality during hospital stay was 20% (4 patients, 16%, attributable to other causes unrelated to tracheotomy). During follow-up and to date, global mortality increased to 28% (7 patients) and 2 patients were lost to follow-up due to treatment in another centre.
No technique-related problems in scheduled cannula replacements, or infections described in other series, such as mediastinitis or sepsis were observed (Table 3).
Analysis of the accidental decannulations subgroup.
| Accidental decannulation (n=5) | General group (n=20) | p value | |
|---|---|---|---|
| Mean age (months) | 22.6±21 | 33.6±44.1 | 0.668 |
| Mean MV days prior to tracheotomy | 60±118.1 | 33.2±38.9 | 0.243 |
| Mean days admission PICU | 41.8±39.07 | 54±74.1 | 0.921 |
| Cuffed cannulas | 0 (0%) | 4 (20%) | 0.275 |
A comparative statistical analysis was performed between the group of patients that presented an episode of accidental decannulation (5 patients) and the rest of the patients (20 patients) to identify possible differential factors.
The mean age of the 5 patients that presented an episode of accidental decannulation was lower than that of the general group (22.6±21.06 v. 33.6±44.11 months). The mean length of stay in the PICU was similar in both groups (41.8±39.07 v. 54.2±74.1 days). The analysis shows that the average number of MV days prior to tracheotomy is clearly higher in the accidental decannulations group (60±118 v. 33.2±38 days), a difference due to the prolonged time on MV of one patient compared to the rest of the group (270 days). However, there was no difference between groups in terms of median MV days (30 v. 30 days). The most frequent indication for tracheotomy in the subgroup of patients that presented an accidental decannulation was tracheobronchomalacia (2 patients).
Among the variables analysed, no statistically significant differences were observed between both groups with regard to mean age, average number of MV days prior to performance of tracheotomy, or mean stay days in the PICU. In spite of the remarkable difference in the use of cuffed cannulas in the accidental decannulations group (0% v. 20% in the rest of the patients), this difference does not reach statistical significance, probably due to the insufficient sample size in the decannulations group.
In total, 80% of the patients who presented an accidental decannulation suffered cardiac arrest as a consequence, and 1 of them died. All of the accidental decannulation episodes occurred within the first 48h of the postoperative period, and 80% within the first 24h.
DiscussionTracheotomy in the paediatric patient is still an uncommon procedure1 (0.5%–2% of patients on MV) that is performed late in ventilated children, usually in the operating theatre.15 In our series, tracheotomised patients constituted approximately 1.5% of all intubated patients. The time when the tracheotomy is performed is still under debate in paediatrics. In adults, where there is a theoretical barrier of 7–10 days of MV, we found that current practice also varies, with rates that range between 5% and 24% of tracheotomies in intubated patients2,16,17 and with a mean of 9 and 12 ventilation days.18 Griffiths et al., in a meta-analysis that included 406 patients, observed that an early tracheotomy significantly reduced the duration of MV and the stay in the ICU.19
The duration of intubation in children is not predicative of the need for a tracheotomy.1 We now know that children can be on MV for months without important complications.12
A survey conducted among paediatric intensive care specialists showed that there is no consensus regarding the time at which a tracheotomy should be performed: 81% of respondents did not agree on indications and time. However, nearly 50% of doctors considered that the procedure was underutilised.20 In the Al-Samri et al. study6 on 70 paediatric tracheotomies, the mean duration (range) of MV before tracheotomy was 20 (0–140) days. In our series, mean MV days prior to tracheotomy was 48 (0–270) days.
Indications for tracheotomy have changed over the years. In the 1970s, inflammatory airway obstruction3,5 (epiglottitis and laryngotracheobronchitis) was the most frequent indication. Today, the main indications are airway stenosis, usually at subglottic level (70%), and prolonged MV (30%).9,11 In our series, 52% of patients had an airway obstruction, either congenital (24%) or subglottic stenosis (12%), and 44% were MV dependent. Only 1 patient required tracheotomy due to an acute infectious process.
To conclude, current indications could be reduced to fixed airway obstruction, airway toilet in ventilator-dependent patients, and predicted long-term use of MV6; although, as indicated by some authors, indications should be case-dependent.1 Non-invasive ventilation, together assisted coughing, is a recent alternative that is reducing the number of tracheotomies in ventilator-dependent patients.6
Tracheotomy is an invasive procedure associated with multiple complications, such as bleeding, infection, subcutaneous emphysema, pneumothorax and tracheal stenosis. Evidence has shown that technique-related morbidity and mortality in paediatric patients are 2–3 times higher than in the adult population.6–8 In our series, as well as in some others4,9,10 (22–77%), we observed a high number of complications (56%), with some patients presenting more than 1 complication. Accidental decannulation stands out due to its high incidence and severity. This occurred in 5 patients (20%). This figure is higher than that reported by Mahadevan et al.,9 where 2.5% of decannulations were observed. Out of the 5 decannulations, 1 patient died due to impossibility of intubation due to presentation of a false passage. This implies a mortality of 4% in this group, which is consistent with the rates reproted by Fraga et al.14 in the literature (0–6%). Interestingly, this was the only case of emergency tracheotomy, and was performed in a patient with acute pathology (laryngitis). This circumstance may have had, in part, a negative effect on the performance of the technique or the fixing of the cannula. It is important to mention the impact that the underlying disease (airway obstruction above the cannula) may have had in the severity of the respiratory failure at the time of the accidental decannulation, and the additional difficulty for orotracheal reintubation following the incident.
When analysing the surgical technique, tracheotomy performed with a vertical skin incision and a horizontal intercartilaginous incision does not seem to differ from the conventional procedure, in which a longitudinal skin incision and a vertical intercartilaginous incision are performed, in terms of mortality and complications.7 However, the surgical technique, as well as the material used to attach the cannula or the suture technique used,21 could be related to decannulations.13 The suture of the trachea to the skin is an important factor to facilitate recannulation in case of accidental decannulation. In our series, our surgical technique did not include this suture, a fact that facilitates recannulation. The deceased patient did not have a cuffed cannula, and neither did the other 4 patients with decannulations. Indications for cuffed cannulas are very limited in paediatrics.22 Cuffed cannulas were not indicated in any of our study patients with accidental decannulation, and we could find no studies where this was found to be a contributing factor to decannulation.
Continuing with the analysis of the accidental decannulations group, we observed that decannulated children are smaller, although the difference was not statistically significant. The age barrier regarding the number of complications, according to different references, is 1 year of age. According to Parrilla et al., complications in children under the age of 1 year are more frequent (48%) than in older patients (27%).4 The higher complication rate in younger children seems to be related to the internal radius of the trachea, which is smaller and more flexible. In fact, airflow through a tube is inversely proportional to the ratio raised to the fourth power.4 As a consequence, a slight reduction of the endotracheal diameter may cause a severe obstruction to airflow in the airway, which is why the airway obstruction complication is more frequent at this age.
This complication may occur at any time, particularly in older children and in children with respiratory assistance, partly influenced by the weight of the ventilator circuit. This may be avoided by using a cannula of adequate size and model,13 as well as the use of secure tracheotomy tube holders. Every new tracheotomy tube should be equipped with an active humidification device until the first change of cannula to prevent obstruction due to plugs secretions.13 Shinkwin et al. recommend that, if decannulation occurs within the first postoperative week, patients should be intubated and then the tracheotomy replaced in more stable conditions.23 All carers of tracheotomised children should be trained to face correctly with accidental decannulation.23 According to Berry et al.24 being under the age of 1, together with the association of congenital cardiopathies and prematurity are associated with a higher mortality in children with tracheotomy.
All the decannulations in our series occurred within the first 48h. This could be due to the degree of stoma maturation, healing and tunnelling.25 During this period, since the stoma is not organised the possibility of creating a false passage is higher than in more developed tracheotomies. Due to the foregoing, we consider that the critical period for decannulations lasts from the performance of the tracheotomy until the first cannula replacement.26 Many authors highlight the importance of postoperative care, the training level of nursing staff in charge of the patient at the time of decannulation27 and the need for an agreed protocol.6,23
The duration of hospital stay of these patients will depend on several factors, including the status of the patient, the availability of home care, financial resources, and the ability of parents and other carers to perform this complex task at home. Our patients were hospitalised for a median (range) duration of 37 (1–388) days.
To conclude, tracheotomy in childhood is related to a high rate of morbidity and mortality. The complication rate is considerable, with a technique-related mortality between 0 and 6%. Tracheotomy control, particularly within the first 48h, is essential. There is no clear consensus regarding indications for and multidisciplinary care of the tracheotomy. Multicentre co-operative studies are required to reach a consensus on the care of tracheotomised paediatric patients.
Conflict of interestThe authors declare that there are no conflicts of interest.
Please cite this article as: García-Urabayen D, López-Fernández YM, Pilar-Orive J, Nieto-Faza M, Gil-Antón J, López-Bayón J, et al. Análisis de las traqueotomías en cuidados intensivos pediátricos durante el periodo 2003–2013. An Pediatr (Barc). 2016;84:18–23.