Wilms tumour is the fourth most frequent tumour in paediatrics, following leukaemia, tumours of the central nervous system and neuroblastoma. Onset typically occurs between ages 3 and 4 years.1 The most frequent sign of its presence is the chance finding of an abdominal mass, and macroscopic haematuria is uncommon at onset. However, there is a form of nephroblastoma known as botryoid Wilms tumour in which this sign is frequently found due to the growth of the tumour towards the collecting duct system.2
We present the case of a boy aged 2 years, asymptomatic and with no personal or family history of interest, brought to the emergency department on the appearance of a blood clot in the diaper. The findings of the physical examination were unremarkable.
An abdominal ultrasound scan was performed, revealing a focal lesion in the right middle kidney extending into the renal pelvis and retrograde dilatation of the calyces. The evaluation was completed with a magnetic resonance scan with contrast, which detected a solid mass in the right renal pelvis measuring 50×47×36mm along the transvers, craniocaudal and anteroposterior axes and reaching the upper third of the ureter, infiltrating the parenchyma of the mesonephros and the inferior pole. The mass appeared heterogeneous and mildly hyperintense in T2-weighted images and hyperintense in T1-weighted images. The mass restricted diffusion and became enhanced on administration of contrast. The right renal calices and right ureter were dilated.
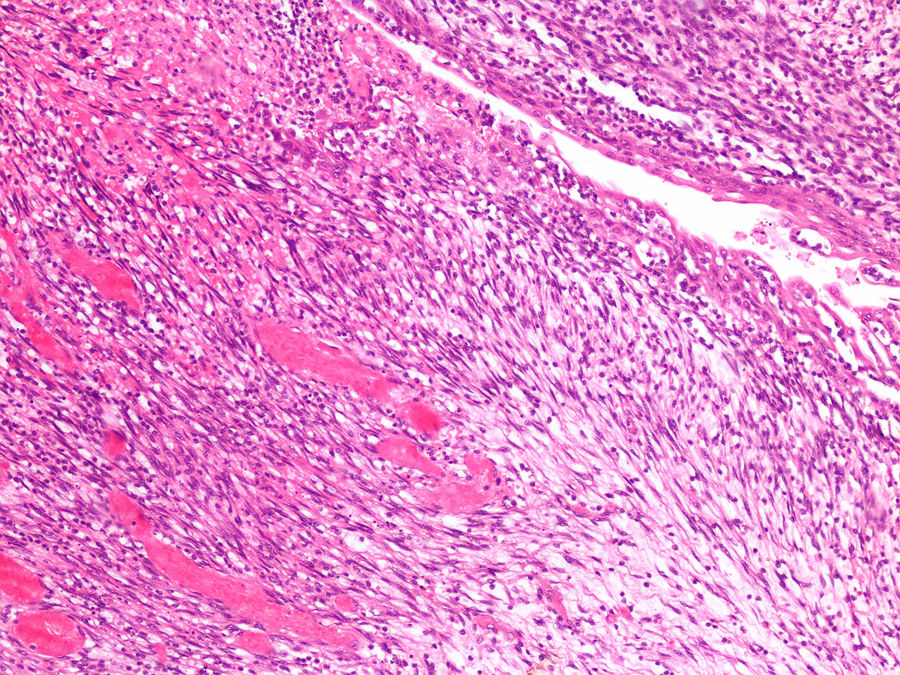
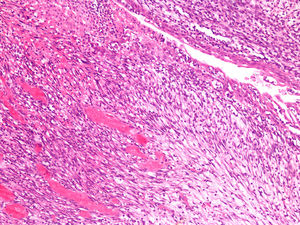
Due to the difficulty in establishing a radiological diagnosis, we decided to perform an ultrasound-guided percutaneous biopsy with a 16G needle. The findings of the pathological examination were compatible with Wilms tumour. The staging evaluation showed no metastasis. The patient received 4 weeks of chemotherapy with vincristine and actinomycin, followed by a right nephrectomy. The histological examination revealed stage II stromal nephroblastoma with infiltration of the renal sinus (Figs. 1 and 2). Later on, the patient completed treatment with 28 weeks of vincristine and actinomycin. At present, the patient remains disease-free 18 months after completing treatment.
Ninety percent of renal tumours in children are nephroblastomas. These tumours are usually found in the renal parenchyma. Nephrogenic rests (nodular collections of embryonal cells that persist beyond 36 weeks’ gestation) are considered precursors of nephroblastoma, as they are found in up to 40% of patients with this tumour and are not associated with any other renal tumours. They are classified as perilobar or intralobar based on their localization in the parenchyma. Intralobar rests involve abnormal development at an earlier stage and are less frequent, but they are more strongly associated with development botryoid Wilms tumour.3
Biopsies for confirmation of cases of Wilms tumour with typical clinical and radiological features are not performed routinely as part of the protocols of International Society of Paediatric Oncology Renal Tumour Study Group (SIOP-RTSG). Approximately 10% of cases manifest as a polypoid mass with a grape bunch appearance that invades the collecting duct system, developing a “botryoid” growth pattern. This usually leads to performance of biopsy for histological confirmation. In case a biopsy is scheduled, it is recommended that it is performed percutaneously with a 16G or 18G needle, avoiding excisional biopsies to avert overstaging.
The concept of “botryoid Wilms tumour” was introduced in 1981 to refer to this growth pattern.4 Initially it was believed that these tumours carried a poorer prognosis due to the assumption that the tumour invaded the collecting duct system. Later evidence demonstrated that in most cases the tumour does not infiltrate the wall of the excretory system.5 Several authors have proposed considering it a form with a better prognosis on account of the higher frequency of favourable histological features2 and the likelihood of an early diagnosis thanks to the frequent occurrence of macroscopic haematuria from an early stage.6 However, the 2 main research groups that study renal tumours (Children Oncology Group and International Society of Paediatric Oncology) have yet to recognise it as a subtype.
When it comes to the resection of Wilms tumour, the abdominal approach is the treatment of choice. To prevent spillage and seeding of the tumour in the ureter or bladder, especially in case of tumours located in the renal pelvis, it is recommended that the ureter be ligated as low as possible and always early in surgery, before any handling of the tumour.
We think it is important to contemplate the possibility of Wilms tumour in the differential diagnosis of any patient with a renal mass, even if it exclusively or mainly involves the collecting duct system. At present, the treatment and prognosis of Wilms tumour must be determined based on the histological subtype and the stage, without taking into account the botryoid growth pattern.2
Please cite this article as: Escalada Pellitero S, Azorin Cuadrillero D, Madero López L, Hernández-Marqués C. Hematuria asintomática como manifestación del tumor de Wilms botrioide. An Pediatr (Barc). 2020;92:370–371.