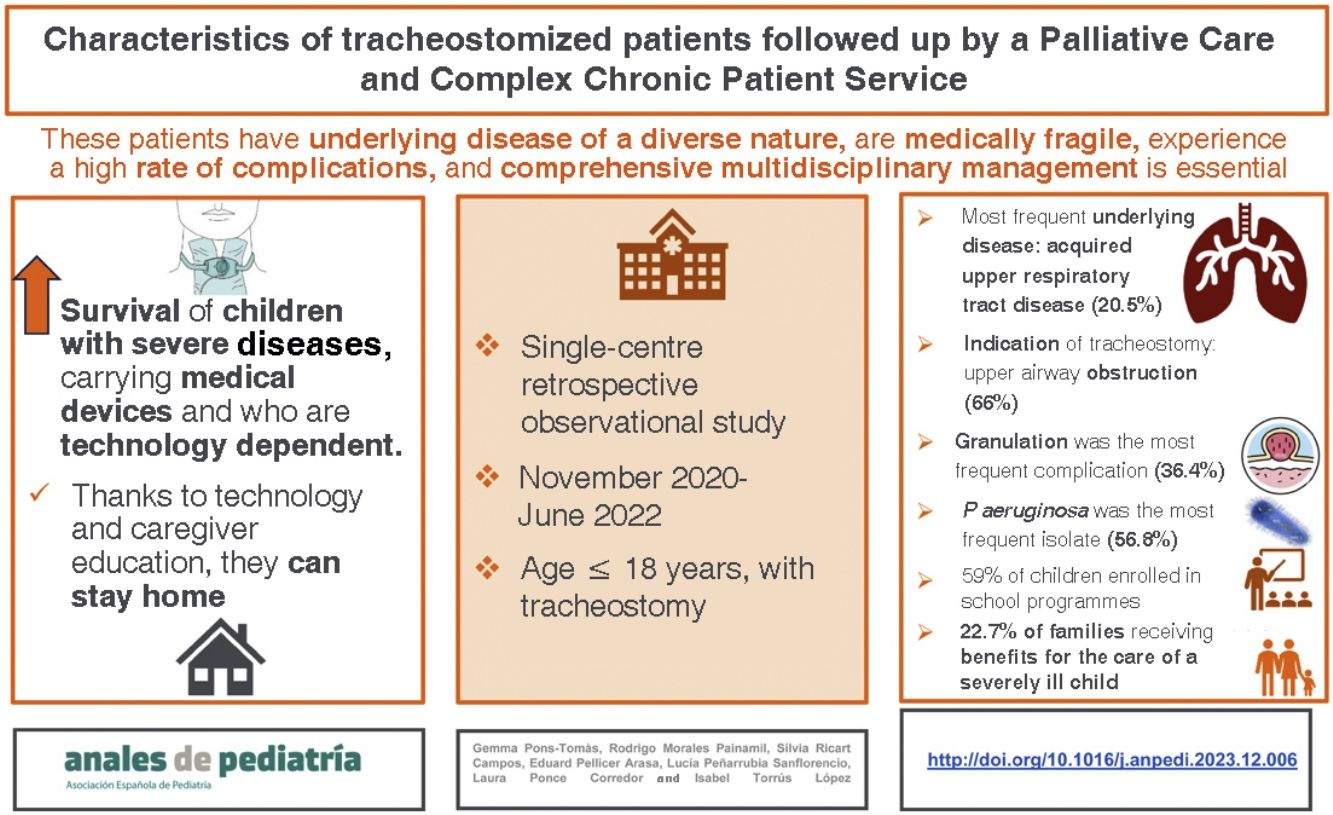
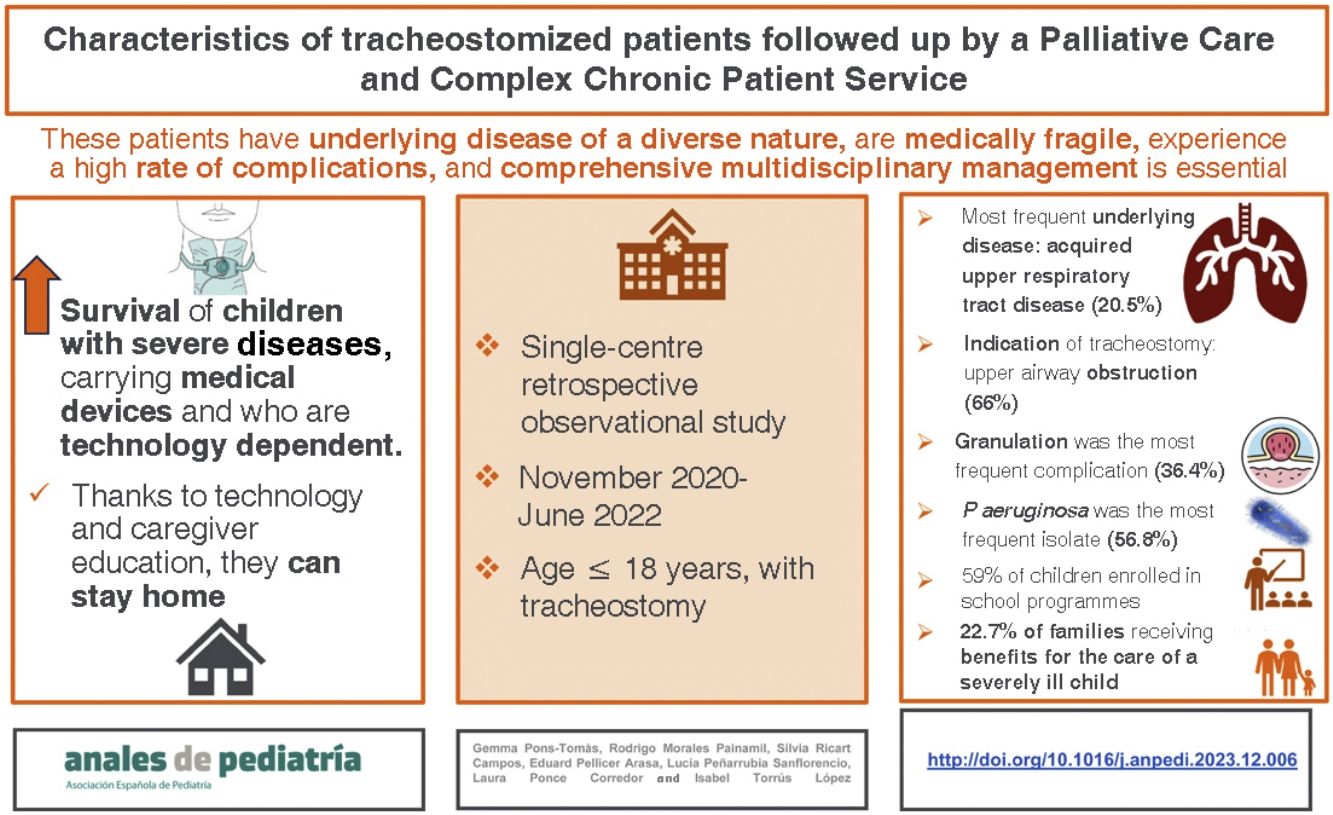
In recent years, there has been an increase in the number of children with tracheostomies. The objective was to describe the characteristics of paediatric patients with a tracheostomy followed up by the Department of Palliative Care and Chronic Medically Complex Illness (DPCCMCI) of a tertiary care hospital.
MethodsSingle-centre retrospective observational study in patients aged less than 18 years with a tracheostomy followed up by the PCCCPS of a tertiary care hospital (November 2020-June 2022). We analysed epidemiological, clinical, microbiological and social data by reviewing the health records.
ResultsThe sample included 44 tracheostomized patients. The most frequent underlying disease was acquired upper airway disease (20.5%). The most common indication for tracheostomy was upper airway obstruction (66%). Bacterial isolates were detected in 84% of the tracheal aspirates, among which P. aeruginosa was the most frequent (56.8%). The most frequently prescribed antibiotic was ciprofloxacin (84%). In addition, 18.1% of the patients received at least 1 course of intravenous antibiotherapy and 29.5% received more than 3 systemic antibiotic regimens in the past 20 months. Fifty-nine percent of the children were schooled: 38.6% attended a regular school, 15.9% a special needs school and 4.5% were home-schooled. We identified social difficulties in 53.7%. Also, 22.7% of the families received financial support to care for a child with severe illness.
ConclusionsBecause of the complexity of caring for tracheostomized children, integral and coordinated management is essential. Schooling is possible and safe if caregivers are trained.
En los últimos años se ha objetivado un incremento de niños portadores de traqueostomía. El objetivo del estudio es describir las características de los pacientes pediátricos traqueostomizados en seguimiento por el SAPPCC de un hospital de tercer nivel.
MétodosEstudio unicéntrico, observacional y retrospectivo que incluyó pacientes ≤18 años portadores de traqueostomía atendidos por el SAPPCC de un hospital de tercer nivel (noviembre 2020-junio 2022). Se analizaron datos epidemiológicos, clínicos, microbiológicos y sociales mediante la revisión de la historia clínica.
ResultadosSe incluyeron 44 pacientes traqueostomizados. La patología de base más frecuente fue la patología de vía aérea superior adquirida (20,5%), siendo la obstrucción de vía aérea superior (66%) la indicación más frecuente de traqueostomía. El 84% presentaron aislamientos bacterianos en aspirado traqueal y P.aeruginosa (56,8%) fue el microorganismo más frecuentemente aislado. El antibiótico sistémico más prescrito fue el ciprofloxacino (84%). Un 18,1% de los pacientes recibió como mínimo una tanda de antibioterapia endovenosa y un 29,5% recibieron más de 3 pautas de antibiótico sistémico en los últimos 20 meses. Un 59% de los niños estaban escolarizados: 38,6% en escuela ordinaria, 15,9% en escuela de educación especial y 4,5% en domicilio. Se identificó familia en crisis en el 53,7% de los pacientes y un 22,7% de las familias disponían de la prestación por Cuidado de Menores con Enfermedad Grave.
ConclusionesDada la complejidad de los niños traqueostomizados, es fundamental un manejo intergral y coordinado. La escolarización es posible y segura si se capacita a sus cuidadores/enfermeras escolares.
In critically ill adult patients, placement of a tracheostomy tube is a frequent procedure. In paediatric care it is much less frequent on account of its technical complexity and the high rate of complications.1,2 Advances in neonatal and paediatric intensive care have achieved an increase in survival of children with severe diseases. Tracheostomy is a procedure that can increase both survival and quality of care in patients who require prolonged mechanical ventilation (MV): it improves interactions between children and their families, increases comfort and reduces the need for sedation and the risk of withdrawal. In addition, early tracheostomy can reduce the severity of oral aversion and metabolic needs, improving growth and developmental outcomes.1 However, the complexity of these patients poses a challenge.3 Most are critically ill, medically complex and have underlying diseases that require the use of medical devices.4 The most frequent indications for tracheostomy are bypassing upper airway obstruction, facilitating suctioning for airway clearance and the need for long-term MV.5
Children with tracheostomies are considered medically fragile because they may develop complications that constitute life-threatening emergencies.6 Intra- and post-operative complications include haemorrhage, infection, pneumothorax, mucus plugging and accidental decannulation. Potential late complications include formation of granulation tissue, mucus plugging, accidental decannulation, bleeding and tracheomalacia.3
Paediatric tracheostomy care chiefly involves tracheostomy suctioning, stoma care and tracheostomy tube cleaning.7 Children with long-term tracheostomies who in the past would have remained in hospital can now return home thanks to advances in technology8 and training of their caregivers.
Few studies in the literature offer a description of the comprehensive followup-of tracheostomised paediatric patients. Most articles present clinical data and do not delve into the impact on the family in socioeconomic terms such as social vulnerability, language barriers or school problems.
Due to the particular characteristics noted above, in our tertiary care women’s and children’s hospital, all paediatric patients with a tracheostomy are followed up by the Department of Palliative Care and Chronic Medically Complex Illness (DPCCMCI).
The aim of this article is to describe the clinical and social profile of paediatric patients with tracheostomy followed up by the DPCCMCI in the last two years.
Material and methodsWe conducted a single-centre retrospective observational and descriptive study including all paediatric patients with a tracheostomy managed by the DPCCMCI of a tertiary care hospital between November 2020 and June 2022. The parents or legal guardians of included patients signed the informed consent to participation.
The data were collected through the review of electronic health records.
To describe patient profiles, we collected quantitative and qualitative data on demographic, clinical, microbiological and social variables. The demographic variables included age, sex, and date of tracheostomy procedure. The clinical variables included the underlying disease, indication of tracheostomy, swallowing disorders, feeding modality, need of MV and/or oxygen therapy, use of a speaking valve or cap, frequency of tube changes, complications and date of decannulation. The microbiological variables included the microorganisms isolated from tracheal aspirate samples, with cultures performed only in the presence of symptoms suggestive of tracheobronchitis (fever, cough, increased in secretions). The Department of Microbiology of the hospital considers that isolates in a tracheal aspirate culture are clinically significant when there is a predominant bacterium that is also a potential airway pathogen. Antimicrobial susceptibility testing is performed in isolates of cultures considered as significant. The decision to interpret the presence of the identified pathogen as colonization versus infection rested with the clinician in charge. We also documented the prescription of antibiotherapy through the nebulised, oral or intravenous route.
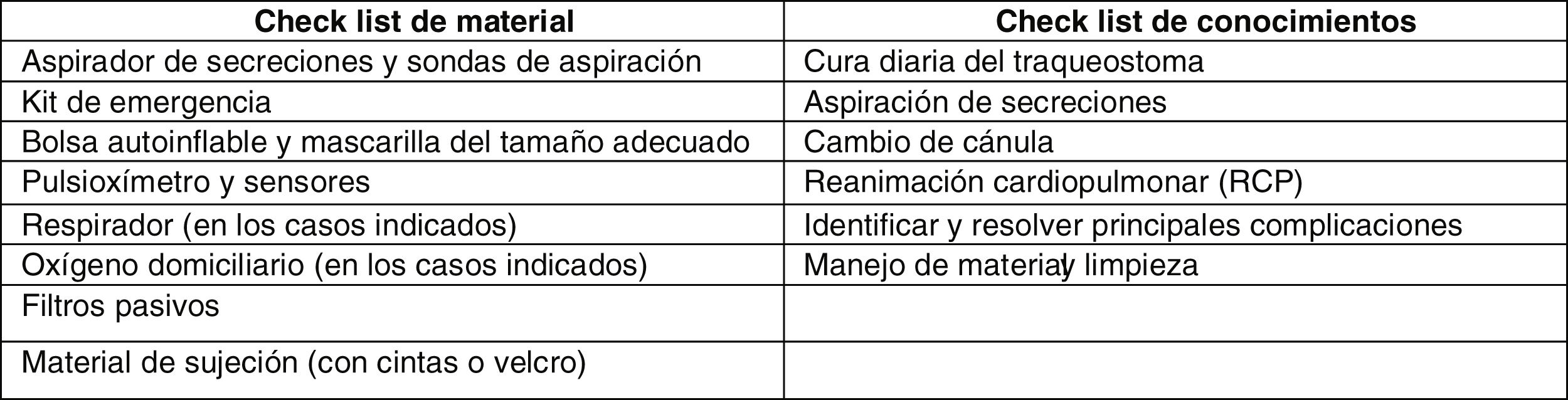
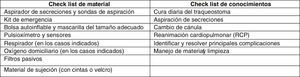
When it came to social variables, we collected information regarding the education provided to families, social risk, requests for care for the paediatric patient, type of schooling and the presence of language barriers. Education on the management of tracheostomy was delivered to the primary caregivers of the patient (usually the parents), at least 2 carers per patient. This training started during the patient’s stay in the paediatric intensive care unit (PICU), carried out by paediatric intensive care specialists and nurses, right after the procedure, and continued during the stay in the paediatric ward (nurses and doctors of the paediatric ward, department of pulmonology and the DPCCMCI). Families received an informational brochure on the care of children with tracheostomy, a document developed in the hospital that is modified as changes and updates are introduced in the management of these patients. Before discharge, the primary caregivers of the child were assessed using a checklist on equipment and theoretical knowledge (Fig. 1).
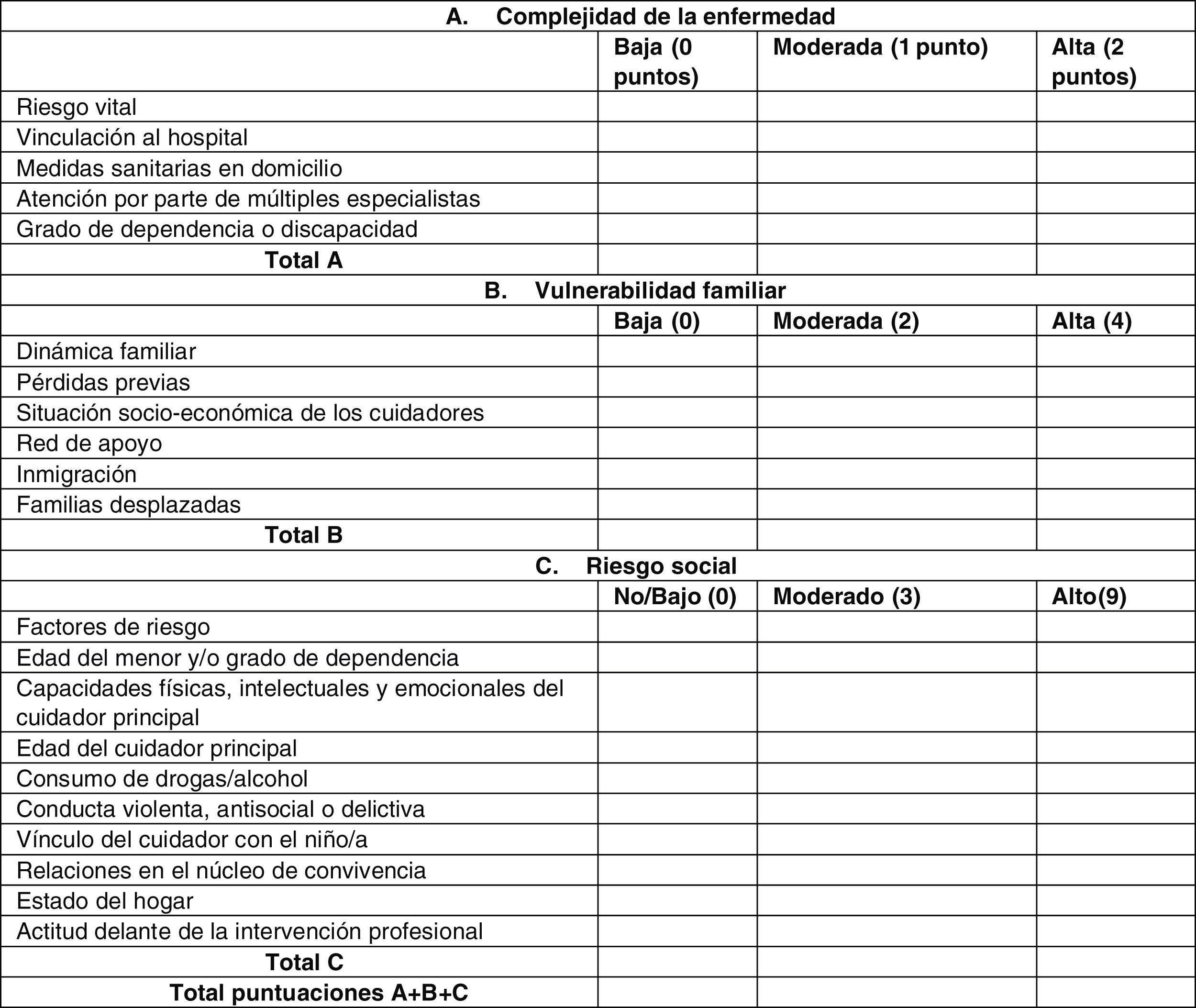
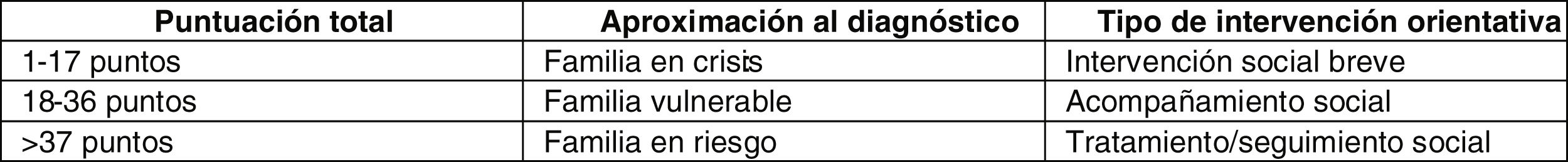
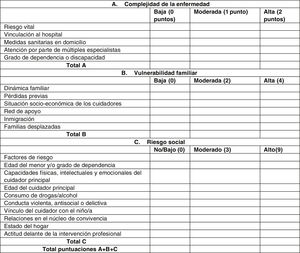
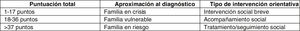
Social risk, in the absence of validated scales, was assessed using a guidance tool applied by the Department of Social Work of the hospital to guide social diagnosis and intervention in paediatric chronic illness (ADISMIC scale: Aproximación Diagnóstica e Intervención Social en la Enfermedad Infantil Crónica)9 (Fig. 2). The social worker of the DPCCMCI passed the scale to each family at the beginning of follow-up, soon after the tracheostomy procedure.
ADISMIC scale used to guide social diagnosis. Each item is scored as absent/low, moderate or high. Group (A) categories refer to the complexity of disease, group (B) categories to family vulnerability and group (C) categories to social risk. The total sum of the scores in the three sections gives an approximate social diagnosis and suggests the type of social work intervention that may be implemented (see Fig. 3).
We entered the data into an Excel spreadsheet formatted for the purpose. The statistical analysis was conducted with the software package SPSS, version 24. We conducted a descriptive analysis of the data, expressing quantitative variables in terms of the mean or median and interquartile range (IQR) and qualitative variables as percentages. The study was approved by the research ethics committee of the hospital.
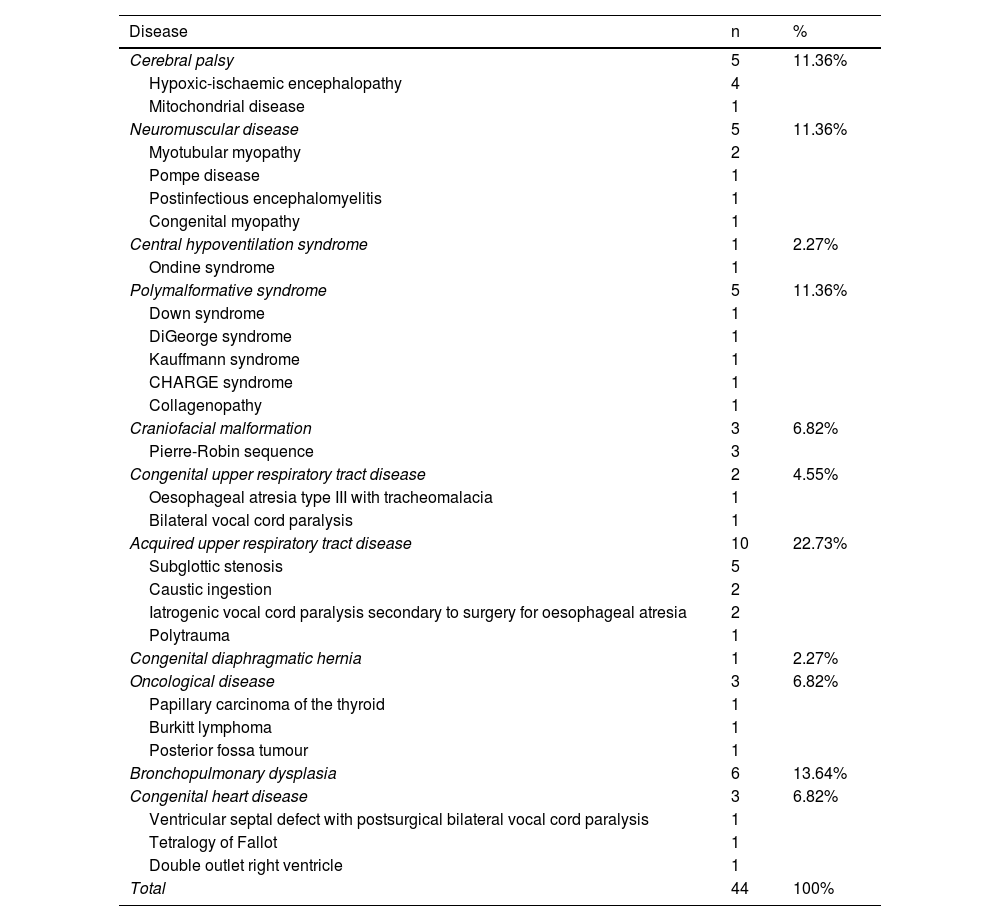
ResultsPatient characteristics and complicationsOf the total of 210 patients followed up by the DPCCMCI of a tertiary care hospital, 44 (20%) had tracheostomy. The median age of these patients was 7.9 years (IQR, 3.85–11.84) and 73% were male. The median age at performance of the tracheostomy procedure was 5.62 months (IQR, 2.6–28.8). The most frequent underlying disease was acquired upper respiratory tract disease (10 patients; 23%).10Table 1 details the underlying diseases in the sample. Sixty-five percent of the patients had swallowing disorders. The feeding modality was oral in 46% of patients, nasogastric (NSG) or gastrostomy tube feeding in 36% and mixed (both modalities) in 18%.
Underlying disease diagnosis in the cohort.
| Disease | n | % |
|---|---|---|
| Cerebral palsy | 5 | 11.36% |
| Hypoxic-ischaemic encephalopathy | 4 | |
| Mitochondrial disease | 1 | |
| Neuromuscular disease | 5 | 11.36% |
| Myotubular myopathy | 2 | |
| Pompe disease | 1 | |
| Postinfectious encephalomyelitis | 1 | |
| Congenital myopathy | 1 | |
| Central hypoventilation syndrome | 1 | 2.27% |
| Ondine syndrome | 1 | |
| Polymalformative syndrome | 5 | 11.36% |
| Down syndrome | 1 | |
| DiGeorge syndrome | 1 | |
| Kauffmann syndrome | 1 | |
| CHARGE syndrome | 1 | |
| Collagenopathy | 1 | |
| Craniofacial malformation | 3 | 6.82% |
| Pierre-Robin sequence | 3 | |
| Congenital upper respiratory tract disease | 2 | 4.55% |
| Oesophageal atresia type III with tracheomalacia | 1 | |
| Bilateral vocal cord paralysis | 1 | |
| Acquired upper respiratory tract disease | 10 | 22.73% |
| Subglottic stenosis | 5 | |
| Caustic ingestion | 2 | |
| Iatrogenic vocal cord paralysis secondary to surgery for oesophageal atresia | 2 | |
| Polytrauma | 1 | |
| Congenital diaphragmatic hernia | 1 | 2.27% |
| Oncological disease | 3 | 6.82% |
| Papillary carcinoma of the thyroid | 1 | |
| Burkitt lymphoma | 1 | |
| Posterior fossa tumour | 1 | |
| Bronchopulmonary dysplasia | 6 | 13.64% |
| Congenital heart disease | 3 | 6.82% |
| Ventricular septal defect with postsurgical bilateral vocal cord paralysis | 1 | |
| Tetralogy of Fallot | 1 | |
| Double outlet right ventricle | 1 | |
| Total | 44 | 100% |
We classified the reason for performance of tracheostomy into chronic respiratory failure (15 patients; 34%) or upper airway obstruction (29 patients; 66%). Thirty-six percent were ventilator-dependent and 11% required oxygen therapy. Fifty-nine percent used a speaking valve or tracheostomy cap.
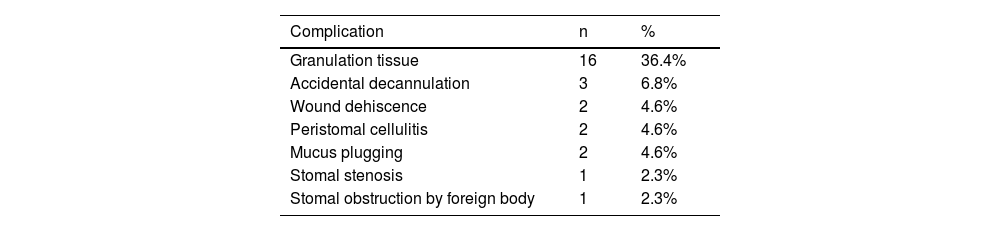
Complications developed in 61% of the patients. Late complications were most frequent: granulation tissue (16 patients; 36.4%) and accidental decannulation (3 patients; 6.8%). Two patients (4.6%) had an early complication, tracheostomy wound dehiscence. Table 2 presents the rest of the complications.
At the time of this writing, 16 patients (36.3%) have undergone decannulation, of whom 75% (12 patients) had tracheocutaneous fistula requiring surgical closure. In these patients, upper airway obstruction was the main indication of tracheostomy (68%), followed by need of prolonged MV in the rest. In the subset who underwent decannulation, the mean duration of tracheostomy was 2.3 years (range, 6 months-7.4 years).
There was one death during the study period, which resulted from arrhythmia as a complication of the underlying disease of the patient. One of the patients was lost to follow-up due to transfer to another hospital.
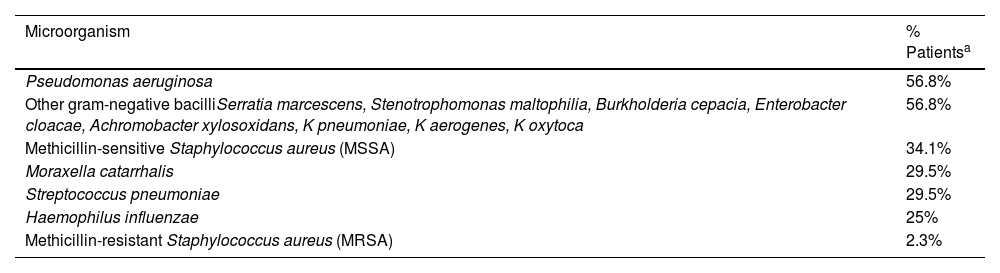
Microbiological isolates and antibiotherapyIn 84% of patients, bacteria were isolated from tracheal aspirate cultures, and coinfection by more than one microorganism was common. The pathogen isolated most frequently was Pseudomonas aeruginosa (56.8%) followed by other gram-negative bacilli associated with hospital-acquired infection (56.8%) and methicillin-sensitive Staphylococcus aureus (34.1%). In the patients with P aeruginosa isolates, 8% of the isolates were multidrug resistant. Table 3 presents the rest of the isolated microorganisms.
Culture isolates in the cohort.
| Microorganism | % Patientsa |
|---|---|
| Pseudomonas aeruginosa | 56.8% |
| Other gram-negative bacilliSerratia marcescens, Stenotrophomonas maltophilia, Burkholderia cepacia, Enterobacter cloacae, Achromobacter xylosoxidans, K pneumoniae, K aerogenes, K oxytoca | 56.8% |
| Methicillin-sensitive Staphylococcus aureus (MSSA) | 34.1% |
| Moraxella catarrhalis | 29.5% |
| Streptococcus pneumoniae | 29.5% |
| Haemophilus influenzae | 25% |
| Methicillin-resistant Staphylococcus aureus (MRSA) | 2.3% |
Nebulised antibiotherapy was delivered to 22.73% of the patients in the past 20 months. The goal of treatment was to reduce the incidence of respiratory exacerbations. The courses of antibiotherapy were prolonged (minimum of 6 months), using tobramycin on an intermittent course (on for 28 days, off for 28 days) or daily colistin.
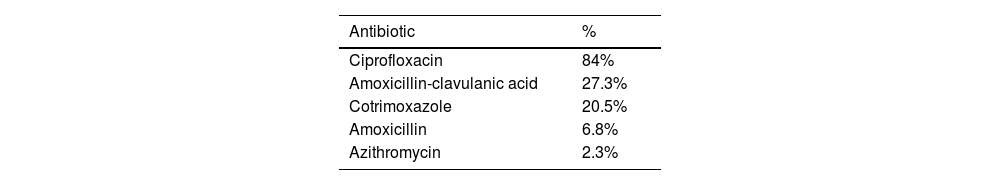
During the study period, oral antibiotics were prescribed to 95% of the patients. The antibiotic selection was based on the tracheal isolates in the past year. The most frequently prescribed antibiotic was ciprofloxacin (84%) followed by amoxicillin-clavulanic acid (27.3%). Table 4 presents detailed information on oral antibiotic prescription. In the sample and period under study, 29.5% of the patients received more than 3 courses of oral antibiotherapy.
In addition, 18.1% received at least one course of intravenous antibiotherapy in the past 20 months.
Social and educational aspectsTracheostomy tube changes by family. Before patients with a tracheostomy were discharged home, training was delivered to families, in 55% of cases to the mother and father.
The tracheostomy tube was changed every 7 days in 45% of the patients and every 14 days in 41% (especially in older children). The parents changed the tracheostomy tube, first with support from the DPCCMCI and autonomously once they had the necessary skills. The setting where tube changes were performed was the home in 90% of patients, the hospital in 7% and a primary care centre in the remaining 3%.
Schooling. Fifty-nine percent of children were enrolled in school: 17 in a conventional school (38.6%), 7 in a special education school (15.9%) and 2 in a home education programme (4.5%). Of the 18 children not enrolled in school, 15 (83.3%) were aged less than 3 and therefore not subject to compulsory education. Children aged more than 3 years who were not enrolled in school had multiple difficulties including severe intellectual disability, remaining at home under their parents care . Children who attended conventional schools were accompanied by a caregiver trained in the basic management of a child with a tracheostomy. The special needs caregiver was appointed by the Department of Education and trained by DPCCMCI nurses. In special education schools, 3 patients had been allocated a school nurse that had also been trained by the DPCCMCI. One of them experienced accidental decannulation at school which was quickly resolved by the school nurse.
Assessment of family risk. Based on the score in the ADISMIC scale, families were classified as being in crisis (22/42) or vulnerable/at risk (17/42), while the risk could not be assessed in 3 families due to missing information in the scale.
A language barrier existed in 36% of the families. Lastly, 22.7% received benefits for caring for a severely ill child.
DiscussionFew studies in the literature have described the profile of paediatric patients with tracheostomy tubes. Al-Samri et al.11 defined the clinical course in 72 children with tracheostomy over a 17-year period. They classified the indications for tracheostomy into 3 groups: upper airway obstruction in a specific anatomical site (45%), upper airway obstruction associated with a complex medical condition (33%) and need of access to lower airways for long-term ventilation (22%). The most frequent indication was obstruction due to subglottic stenosis (21%) or in the context of a complex craniofacial syndrome (21%). In our sample, the most frequent indication was also upper airway obstruction (66%), chiefly subglottic stenosis and vocal cord paralysis. Therefore, most patients in the cohort were not ventilator-dependent. It is important to take into account the advances achieved in the past 30 years in non-invasive home mechanical ventilation ,12 which has allowed a reduction in the performance of tracheostomy in patients who require long-term ventilation.
The most frequent complications in our study were granulation tissue, in agreement with the findings of Lubianca Neto et al.13 in a systematic review of cases ranging from 1978 to 2020. The authors reported a mean rate of complications of 40%, with cutaneous lesions and granulation tissue being the most frequent types, as was the case in our series.
Respiratory infections, including tracheobronchitis and pneumonia, are common in paediatric patients with tracheostomies and are associated with antibiotic prescribing and a high rate of hospitalization.14 In most children with an artificial airway, the trachea is colonised by a broad range of bacteria that are not present in the healthy pharyngeal microbiome. A study conducted in 93 children with long-term tracheostomies in the United States15 found a predominance of gram-negative bacteria. Still, 55.9% of patients had cultures positive for methicillin-resistant S aureus (MRSA) and the prevalence of MRSA and of methicillin-sensitive S aureus (MSSA) was higher in the first year following tracheostomy placement and decreased thereafter. In contrast, the prevalence of P aeruginosa remained relatively stable, with detection in 60%–80% of the patients, regardless of the time elapsed since the procedure. In our sample, the most prevalent microorganism was P aeruginosa, followed by other nosocomial gram-negative bacilli and, third in frequency, MSSA, with a lower prevalence of MRSA compared to case series in the United States.
Paediatric patients with tracheostomies frequently receive systemic broad-spectrum antibiotics. In our study, most patients had received a course of systemic antibiotherapy in the past 20 months, and ciprofloxacin was the agent prescribed most frequently. Nearly 30% of the patients had received 3 or more courses of systemic antibiotherapy in the past 20 months. The use of broad-spectrum antibiotics increases the risk of antimicrobial drug resistance, promoted by frequent exposure to antimicrobials in health care settings that serve as reservoirs for these microorganisms. They also have adverse effects, most frequently diarrhoea.14 It is important to give careful consideration to the indication of treatment for bacteria isolated from tracheal aspirate specimens, as their presence may be limited to airway colonization. The possibility of not initially treating a respiratory exacerbation with antibiotics should also be considered, since viral etiology is more frequent in pediatrics. If the patient is stable and exhibits no other signs of bacterial infection, watchful waiting should be contemplated. If antibiotherapy is initiated, early discontinuation should be considered if bacterial infection is not confirmed by culture, and otherwise, antibiotic de-escalation based on the results of susceptibility testing.
The decision to discharge home a child with a tracheostomy requires careful planning.16 There are few published data on the follow-up of these patients by multidisciplinary paediatric chronic medically complex condition units. The DPCCMCI in our hospital is staffed by paediatricians, nurses, social workers, psychologists and spiritual counsellors to deliver comprehensive care to patients and coordinate services at different levels of care, chiefly primary care and specialised medical care. Patients with tracheostomy are referred to the DPCCMCI once the procedure has been performed to provide support through the training of families, discharge planning and management, post-discharge outpatient follow-up and coordination of out-of-hospital services.
Paediatric tracheostomy has an impact on the life of both the patient and the family, described by Hopkins et al.17 in a case series in the United Kingdom. The authors found a deleterious effect on quality of life, sleep, social life and work. Defining the social needs of paediatric patients is difficult, as there are no validated scales for the paediatric age group to help make a social diagnosis and develop an intervention plan. In our study, we analysed social risk through the ADISMIC scale and found that more than half of the families were in crisis and the rest at risk. In nearly 25% of families, one of the caregivers was exclusively dedicated to the care of the child, as the child required continuous in-person care. This was incompatible with work, so these families received benefits for caring for the ill child. The high percentage of families with a language barrier (36%) must also be taken into account when training families, as it is an additional difficulty.
More than half of the patients in the study were enrolled in school, and most of them attended conventional schools, with the percentage rising to 89.6% if we only take into account children in the age range in which schooling is compulsory. Children attending conventional schools were accompanied by a caregiver trained on basic tracheostomy care, a task performed by nurses in the DPCCMCI without which it would not be possible to guarantee the safety of the patient in the school setting. Few studies in the literature focus on the schooling of children with tracheostomy. Patel et al.18 assessed the school experience of children with tracheostomy tubes: more than half of the schools did not have any properly trained staff, in 2 cases the parents did not know whether the school had such staff and 5 school did have a school nurse or an adequately trained teacher, but they were not always available. The authors concluded that it was important to improve coordination of care with schools as part of the multidisciplinary management of these children.
ConclusionAn increasing number of children with a broad diversity of underlying diseases require tracheostomy, and the main indication for it is bypassing upper airway obstruction. They are fragile patients with a high risk of complications, so it is essential to train families and to ensure comprehensive and coordinated care. The social analysis of the families included in the study evinced that more than half were in crisis, which reflects the impact of a child with a tracheostomy on the family and highlights the importance of addressing the social needs of these patients. For this reason, models of care by multidisciplinary teams that offer comprehensive follow-up and coordination between services and different levels of care, such as children's medically complex diseases units, are necessary. Schooling of children with tracheostomies is possible and can be safe if caregivers and/or school nurses are trained on the management and care of tracheostomies.
Ethical considerationsThe study was approved by the Ethics Committee for Research with Medicines of the Fundació Sant Joan de Déu. ECRM Code: PIC-39-21.
FundingThis research did not receive any external funding.
Conflicts of interestThe authors have no conflicts of interest to declare.