Low concentrations of plasma citrulline and arginine have been reported in children under various pathological conditions. Hypothesis: Plasma citrulline and arginine levels undergo different kinetics during the early days of critical illness in children according to the severity of symptoms and can be correlated with other clinical and laboratory parameters associated with the SIR.
Patients and methodsA single-center prospective observational study was done in patients aged 7 days to 14 years admitted to PICU. Citrulline and arginine blood levels (blood in dry paper, analysis by mass spectrometry in tandem), acute phase reactants and clinical data were collected on admission, at 12h, 24h, 3 and 7 days.
ResultsForty-four critically ill patients were included and the control group was formed by 42 healthy children. The citrulline and arginine kinetic analysis showed: (1) citrulline falls significantly (p<0.05) at 12h of admission; levels remain low until day 7 and begin progressive increase again; (2) arginine is already lowered at 6h, although an earlier rise occurs (3rd day); and (3) the decrease of citrulline in the first three days of admission positively correlates with arginine kinetics. Bivariate analysis showed: (1) correlation of elevated citrulline on the 7th day with shorter duration of mechanical ventilation, lower PICU stay and lower occurrence of complications. The levels of citrulline still descended at day 7 are associated with increased CRP/procalcitonin elevation at first 24h; (2) the greatest decrease of arginine in the first 12h is associated with a longer PICU stay and greater number of complications and increase of acute phase reactants at 3 days.
ConclusionsThere are decreased levels of arginine and citrulline in the first days at PICU, with recovery at the 3rd and 7th day respectively, and a relationship between a greater decrease and a worse outcome and between a longer income and a higher serum CRP/procalcitonin.
Se ha documentado bajas concentraciones de citrulina y arginina plasmáticas en niños en diversas condiciones patológicas. Hipótesis: La cinética de citrulina y arginina plasmáticas durante la enfermedad crítica pediátrica se correlaciona con parámetros evolutivos clínicos y bioquímicos.
Pacientes y métodosEstudio observacional unicéntrico prospectivo en pacientes de 7 días a 14 años ingresados en unidad de cuidados intensivos pediátricos (PICU). Los datos bioquímicos y clínicos fueron recogidos al ingreso, a las 12h, a las 24h, al 3° y al 7° día.
Resultados44 pacientes críticamente enfermos fueron incluidos y un grupo control de 51 niños sanos. La citrulina desciende de forma significativa (p<0,05) a las 12h de ingreso con niveles bajos mantenidos hasta el día 7, comenzando un aumento progresivo después. La arginina ya está descendida a las 6h, aunque tiene una subida más precoz (día 3). La disminución de citrulina al tercer día se correlaciona directamente con la arginina. Hay correlación entre la elevación de la citrulina al séptimo día con menor duración de ventilación mecánica, menor estancia en (PICU) y menos complicaciones. Los niveles de citrulina aún descendidos el día 7 se asocian con un mayor aumento de PCR y procalcitonina en primeras 24h. La disminución de arginina en las primeras 12h se correlaciona inversamente con estancia más larga, mayor número de complicaciones y aumento de reactantes de fase aguda en día 3.
ConclusionesHay disminución de arginina y citrulina en los primeros días de la enfermedad crítica, con recuperación al tercero y séptimo día, respectivamente, y existe una relación entre mayor disminución y peor evolución.
Citrulline is a non-protein amino acid produced by the intestinal mucosa from glutamine and amino acid derivatives.1 Arginine is a conditionally essential amino acid and the most abundant nitrogen carrier in our body; it is obtained from dietary sources and endogenously synthesized in the kidney from citrulline in the urea cycle.2 Arginine has secretagogue (insulin, IGF-I, glucagon, prolactin), and timotrophic (increased production of lymphocytes and macrophages) effects. It is a precursor of various molecules of great importance in the compensatory mechanisms involved in the systemic inflammatory response syndrome (SIRS) as well, through specific enzymes with different functions, such as: arginase, arginine–glycine aminotransferase and nitric oxide synthase (NOS).
In systemic inflammatory response syndrome (SIRS) situations, an increased activity in inducible NOS (iNOS) calcium independent has been demonstrated. This leads, through vasodilation, to hypotension and septic shock; peroxynitrils released within this context generate tissue damage and myocardial depression. Activation of the inducible isoform causes arginine depletion which limits their availability and the activity of T cells leading to reduced response to infection. Recent reviews on intestinal barrier dysfunction have explored how the intestine, both as culprit and victim, influences the pathophysiology of SIRS.3
The gut is hypothesized to play a central role in the pathophysiology of critical illness and is frequently called the “motor” of the systemic inflammatory response. Perturbations to the intestinal barrier can lead to distant organ damage and multiple organ dysfunction syndrome (MODS). Small intestinal function in critically ill patients should ideally be assessed in order to determine the preferred feeding route, timing, and composition of enteral nutrition. Additionally, evaluation of small bowel function may lead to new insights aimed to maintain enterocyte integrity. Critically ill patients are likely to have impaired enterocyte function mainly as a consequence of diminished splanchnic blood flow associated with mucosal hyperpermeability and bacterial translocation, a pathological state believed to be pivotal in the development of sepsis and MODS.4
Low plasma citrulline and arginine concentrations have been described in children with various pathological conditions,5 many of them related to bowel problems.6 Decreased arginine levels have been demonstrated in sepsis in adult patients.7 Previous studies in critical adult patients have proposed arginine and citrulline as early mortality markers with contradictory results,8,9 with no similar data in children up to this time.
The aim of this study is to determine the correlation between plasma citrulline and arginine levels and severity and degree of SIRS.
Patients and methodsSingle-center prospective observational study. Patients enrolled were divided into two groups, one critically ill children group (Group A) and one control group formed by non-hospitalized healthy children with no known disease and with no active infection in the previous month (Group B). Group A was formed by patients admitted to PICU between January and May 2012 who fulfilled the inclusion criteria: age 7 days to 14 years, with expected minimum length of stay of 3 days and signed informed consent. Exclusion criteria were intestinal surgery, abdominal radiotherapy, intestinal inflammation or necrosis (enterocolitis, mucositis, etc.), development of pulmonary hypertension and age less than 7 days.
We reviewed clinical data (stay in PICU, duration of mechanical ventilation (MV), vasoactive support) and laboratory values (leucocytes, uric, C reactive protein (CRP), procalcitonin (PCT), albumin, arginine and citrulline). Samples for citrulline and arginine detection were collected on dry paper S&S 903 and analyzed by tandem-mass spectrometry, all of them at the end of the collection, performing duplicate determinations for checking test variability. The blood samples on paper were stored frozen at −20°C, keeping them dry and protected from light. Samples for other acute phase reactants were collected at admission, 12h, 24h, 3 days and 7 days. All samples were collected after 3h of fasting conditions, thus amino acid results represent postabsorptive conditions.
The Pediatric Risk of Mortality (PRISM) is a prognostic scoring system that was developed to set the physiologic variables required for pediatric intensive-care unit (PICU) mortality risk assessment and to obtain an objective weighing of the variables analyzed. Results are adjusted for age (months) and expressed as percentage (risk of mortality). The severity of respiratory dysfunction was measured by PaO2/FiO2 (PF) ratios, which require a daily arterial blood gas measurement.
We have considered neurological dysfunction if cerebral vascular injury (imaging test) has developed, or if regional cerebral tissue oxygen saturation decreased at least 20% from baseline for 15s (cerebral desaturation). It has been chosen as a marker of morbidity to require at least 1-week stay in the intensive care unit. Pulmonary dysfunction was set when PaO2/FiO2 was <300 and renal dysfunction when plasma creatinine was increased more than 20% when comparing with basal. Unfavorable evolution was defined when pulmonary, renal or neurological dysfunctions were set, when there was a need for two or more vasoactive drugs (hemodynamic instability) or if death finally occurred. Thus, we divided group A into two subgroups (A1: favorable condition; A2: unfavorable condition).
Informed consent was obtained from all subjects’ parents. Ethical approval for this study was provided by the Ethical Committee “CEI de Centro Provincial de Málaga” in 2011. A descriptive analysis was performed, expressing continuous variables as median and interquartile range (IQ) and categorical variables as frequencies and percentages. Variables with a normal distribution and equal variances were compared between the groups with an independent-sample t test. When a variable failed the normality or equal variance tests, the Mann–Whitney test was used for comparison. Comparison of means for favorable, unfavorable and control subjects was performed by means of an ANOVA test. A Spearman's ρ was used to correlate variables. Statistical significance was defined as a 2-tailed p 0.05.
ResultsA total of 44 patients were finally included in group A (32 in subgroup A1 and 12 in A2): 43.1% were males, median age was 7.3 months (IQ 2.9–41.7), pediatric risk of mortality score (PRISM) in the first 24h of admission was 6.65% (IQ 2.07–6.65) with an average length of stay in intensive care unit of 6.0 days (IQ 4–10). Mechanical ventilation was used in 90.2% of patients admitted, only 38.5% for longer than 24h; vasoactive drugs were employed in 50.8%. Hemodynamic instability was the main complication (17%), followed by respiratory distress (16%), renal dysfunction (14%), neurological impairment (5%) and nosocomial sepsis (5%), with no significant complication in 54% (24 patients); one patient died during follow-up.
Control group B was formed by 51 healthy non-celiac children, with normal liver and kidney (creatinine 0.38mg/dl) function and a mean age of 4.9±2.4 years, with normal 24-h fecal fat (2.2g/24h). Age adjustment has been performed by direct methods.
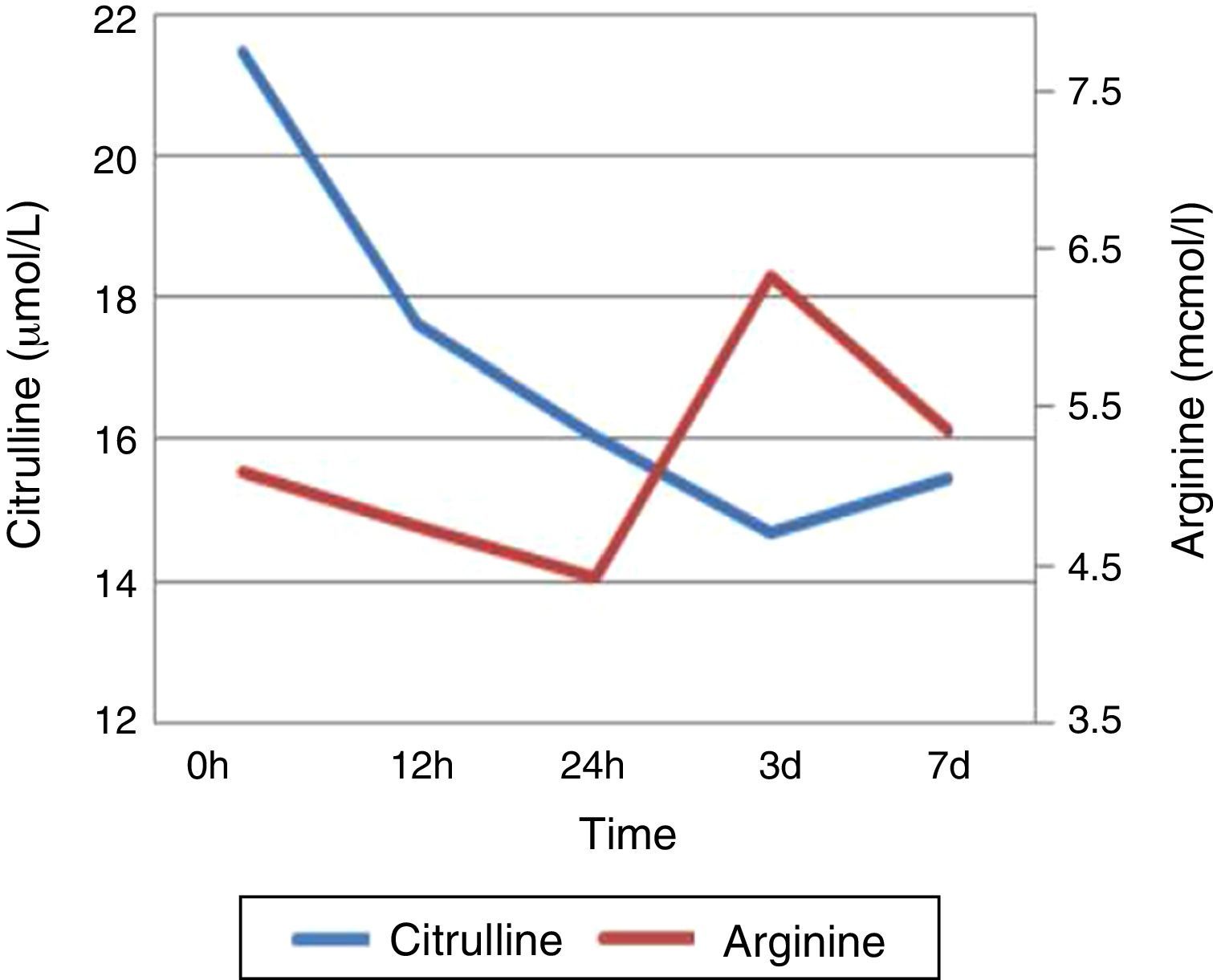
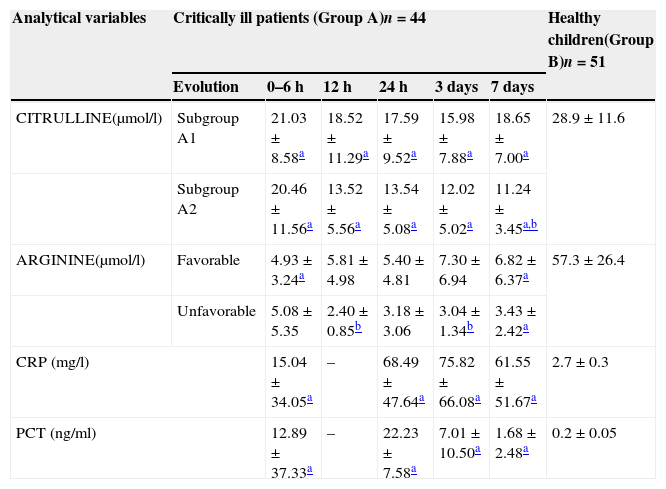
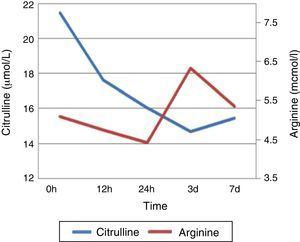
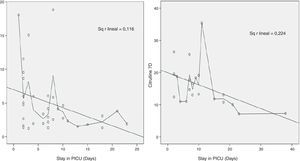
Table 1 shows plasma citrulline and arginine kinetics, allowing comparisons between healthy subjects and critically ill children. Control group maintains plasma citrulline levels always higher than critically ill children (28.9±11.6μmol/l, p=0.0001), and the same goes for arginine (57.3±26.4μmol/l, p=0.0001). Regarding citrulline, there is a significant decrease at 12h after admission (p<0.05), with maintained low levels until day 7. Arginine is already lowered in first 6h after admission, resulting in a further rise (day 3), remaining stable thereafter (Fig. 1). There is statistically significant direct correlation between citrulline and arginine at first 12h (p 0.049); besides, there is also a positive correlation between arginine levels at first 24h and citrulline at 12h, 24h and 3rd day (p 0.003, p 0.0001, p 0.049, respectively). Demographics for both subgroups in case group A were obtained and are shown in Table 2.
Kinetics for main study of analytical variables, when comparing healthy subjects and both groups of critically ill children (subgroup A1: favorable condition; subgroup A2: unfavorable condition).
| Analytical variables | Critically ill patients (Group A)n=44 | Healthy children(Group B)n=51 | |||||
|---|---|---|---|---|---|---|---|
| Evolution | 0–6h | 12h | 24h | 3 days | 7 days | ||
| CITRULLINE(μmol/l) | Subgroup A1 | 21.03±8.58a | 18.52±11.29a | 17.59±9.52a | 15.98±7.88a | 18.65±7.00a | 28.9±11.6 |
| Subgroup A2 | 20.46±11.56a | 13.52±5.56a | 13.54±5.08a | 12.02±5.02a | 11.24±3.45a,b | ||
| ARGININE(μmol/l) | Favorable | 4.93±3.24a | 5.81±4.98 | 5.40±4.81 | 7.30±6.94 | 6.82±6.37a | 57.3±26.4 |
| Unfavorable | 5.08±5.35 | 2.40±0.85b | 3.18±3.06 | 3.04±1.34b | 3.43±2.42a | ||
| CRP (mg/l) | 15.04±34.05a | – | 68.49±47.64a | 75.82±66.08a | 61.55±51.67a | 2.7±0.3 | |
| PCT (ng/ml) | 12.89±37.33a | – | 22.23±7.58a | 7.01±10.50a | 1.68±2.48a | 0.2±0.05 | |
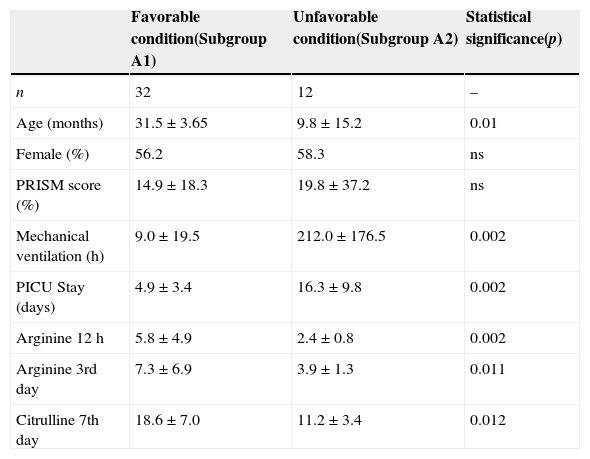
Demographics of group A, comparing those patients with favorable and unfavorable condition, and analytical statistical evaluation.
| Favorable condition(Subgroup A1) | Unfavorable condition(Subgroup A2) | Statistical significance(p) | |
|---|---|---|---|
| n | 32 | 12 | – |
| Age (months) | 31.5±3.65 | 9.8±15.2 | 0.01 |
| Female (%) | 56.2 | 58.3 | ns |
| PRISM score (%) | 14.9±18.3 | 19.8±37.2 | ns |
| Mechanical ventilation (h) | 9.0±19.5 | 212.0±176.5 | 0.002 |
| PICU Stay (days) | 4.9±3.4 | 16.3±9.8 | 0.002 |
| Arginine 12h | 5.8±4.9 | 2.4±0.8 | 0.002 |
| Arginine 3rd day | 7.3±6.9 | 3.9±1.3 | 0.011 |
| Citrulline 7th day | 18.6±7.0 | 11.2±3.4 | 0.012 |
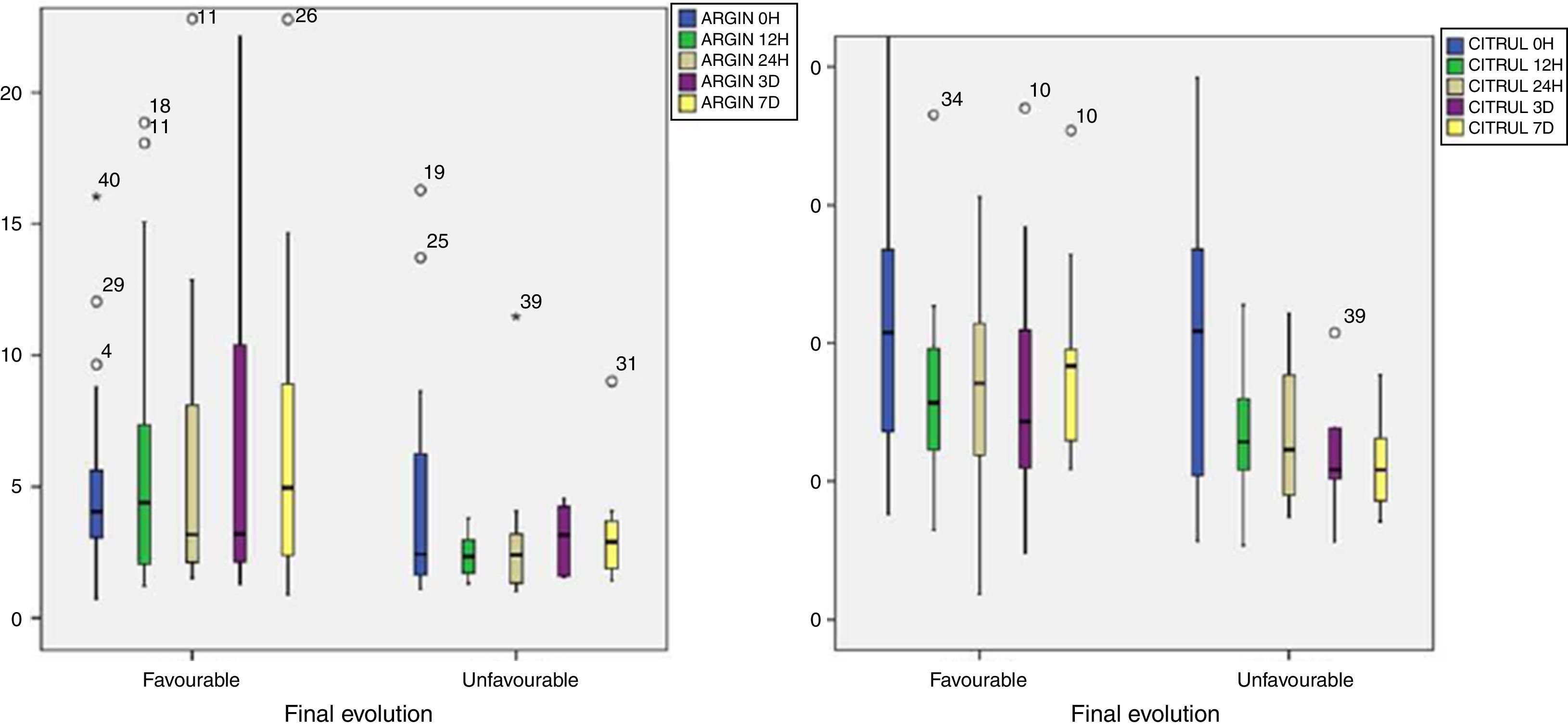
When comparing both groups of critically ill children (those with favorable and unfavorable evolution) it can be seen that there are statistically significant differences in arginine at 12h (p 0.002), arginine at 3rd day (p 0.011) and citrulline at 7th day (p 0.005), being always lower in unfavorable conditions.
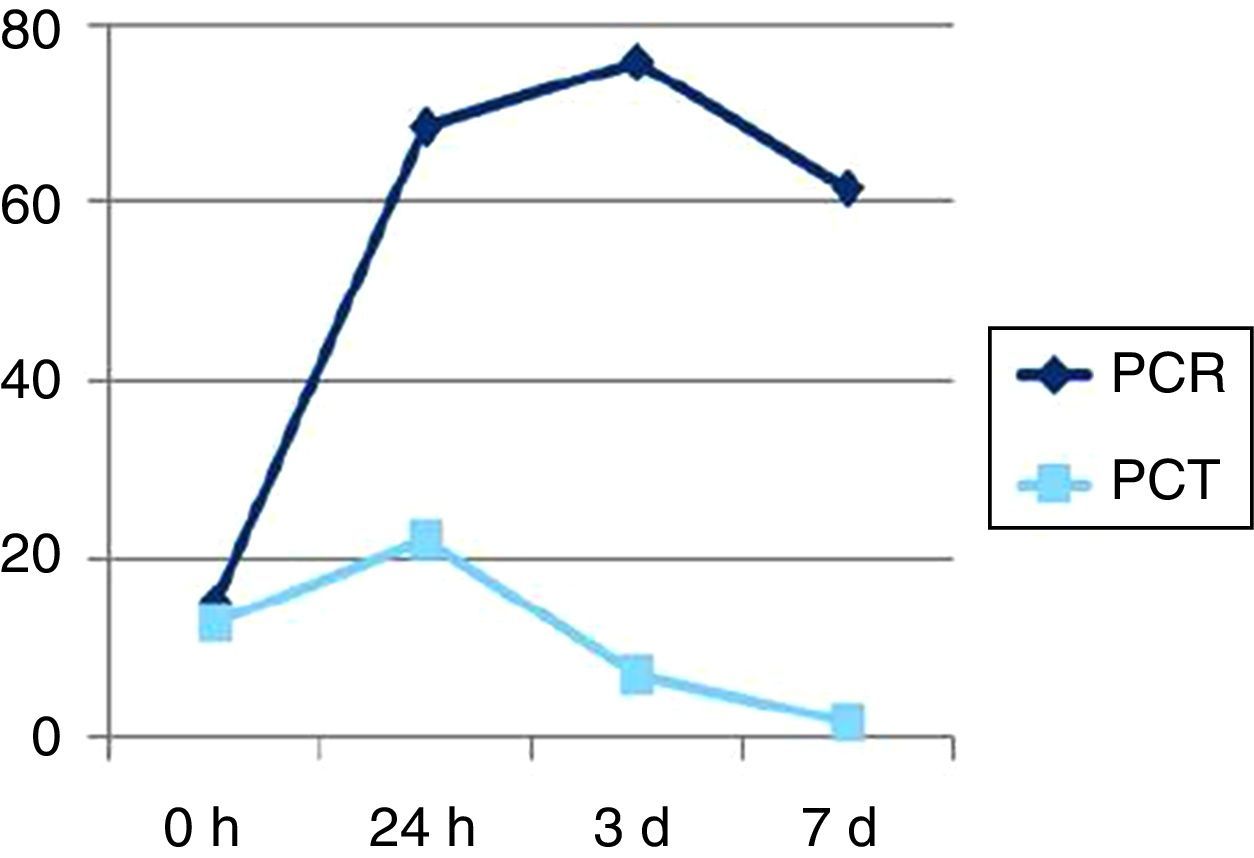
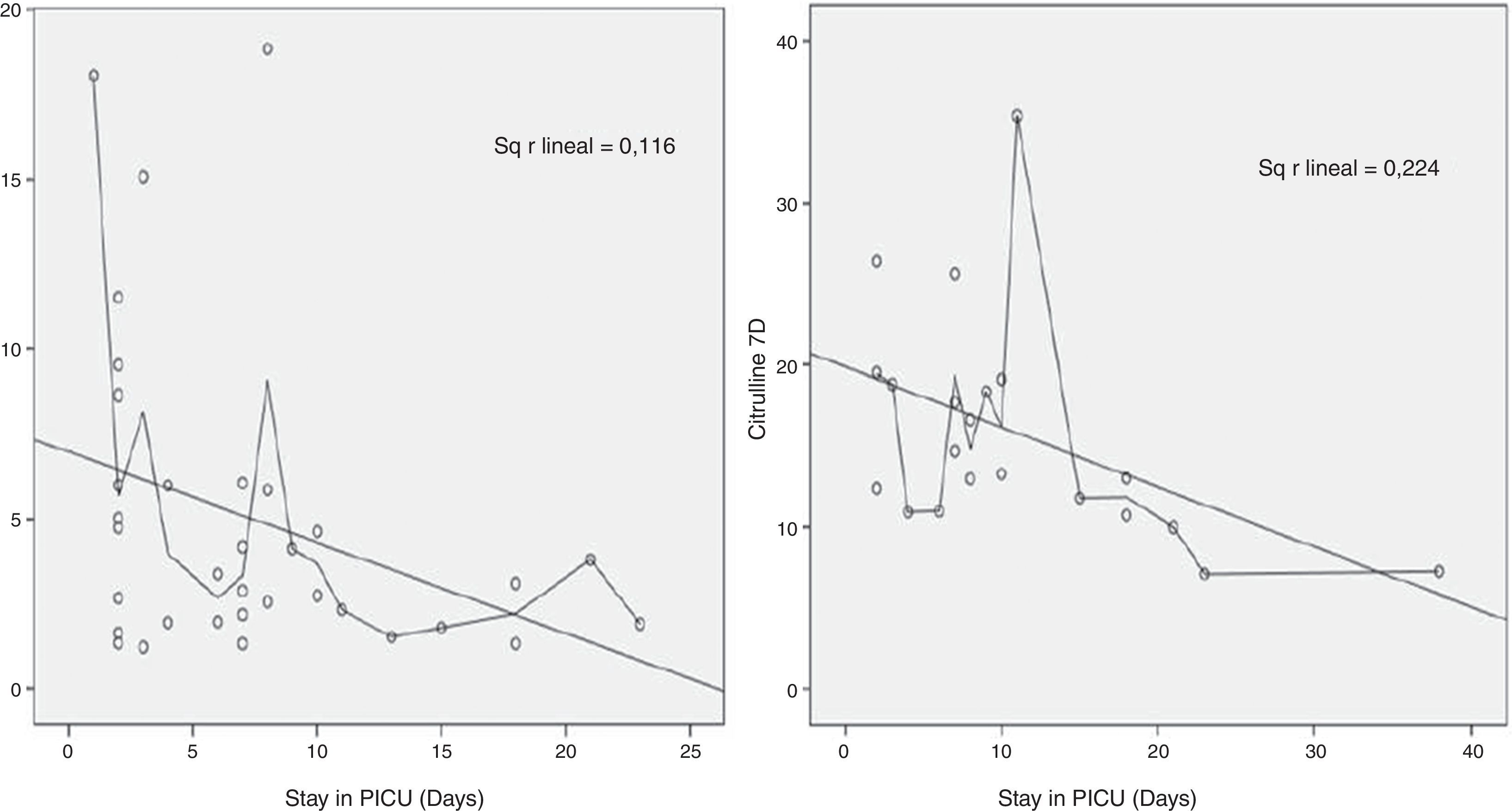
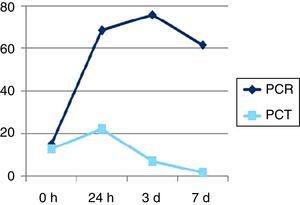
Fig. 2 shows differences in citrulline and arginine kinetics when looking at final evolution, with higher decrease in both variables when there is an unfavorable evolution, and Fig. 3 represents CRP and procalcitonin kinetics. There is a clear negative correlation between citrulline on 7th day (Fig. 4) and duration of MV (ρ=−0.6, p=0.005), stay in PICU (ρ=−0.5, p=0.021), and less occurrence of complications (ρ=−0.59, p=0.012). There is also a statistically significant negative correlation between arginine's largest decline in the first 12h and longer stay in PICU (ρ=−0.35, p=0.042) and more complications (ρ=−0.32, p=0.022).
Among the analytical correlations, citrulline maintained low at day 7 is associated with increased CRP (ρ=−0.47, p=0.033) and PCT at 24h (ρ=−0.67, p≤0.002). The largest the decline in arginine levels in first 12h is, the higher the increase of CRP at 3 days (ρ=0.40, p=0.06) and PCT at 3 days (ρ=−0.52, p=0.017).
DiscussionIn-depth studies of changes in arginine and citrulline metabolism in adult patients with sepsis are limited. In pediatric patients with sepsis, arginine metabolism was studied in detail by using stable isotopes.10 The age adjustment is a widely used technique in epidemiology to eliminate confounding bias introduced by the different age compositions of various populations and to facilitate a summary of data from specific rates. The most widely used method, known as direct-fit, proposed by Neison in 1844 and consists of calculating the weighted average of the age-specific rates, using as weights the composition of an arbitrary reference population.
As pulmonary hypertension is related with arginine levels, and influenced by carbamoyl phosphate synthethase polymorphisms; we did not select patients who were admitted to the unit suffering from pulmonary hypertension.
The reduction in plasma amino acid concentrations with inflammation is attributed, in large part, to an enhanced metabolic clearance of the released amino acids, probably facilitated by the liver for hepatic protein synthesis, gluconeogenesis, and urea synthesis.
In our series, plasma citrulline levels fall rapidly and are significantly below normal levels (control group) at 12h (usually considered as normal between 18 and 35μmol/l), maintaining lower levels than control subjects until 7th day. Arginine is already decreased in the first 6h when comparing with controls, with a faster increase (3rd day).
Normal plasma citrulline and arginine levels in children aged 1–48 months are ranged 4–52μmol/L and 14–147μmol/L respectively in published papers, which is quite similar to our results in the control group (28.9±11.6 and 57.3±26.4μmol/L, respectively). In some studies it has been proven that citrulline is similar in patients suffering from anorexia nervosa and in healthy people, which is explained by the fact that protein-caloric malnutrition does not depend on intestinal failure, therefore there is a low intake without loss of enterocitary mass.
In enterocytes, glutamine serves as the major source of energy; another metabolic fate of glutamine is conversion to citrulline. Because SIRS can affect gut function and integrity, alterations in glutamine metabolism may exist and lead to decreased citrulline production. Our results demonstrate lower plasma citrulline concentrations in SIRS, which may be in part a result of a defect in the metabolic conversion of glutamine to citrulline, decreased uptake of glutamine by the enterocyte but increased uptake by the liver, and/or shunting of glutamine to other metabolic pathways.
A study published in 200911 suggests the existence of increased proteolysis in sepsis, with a decreased arginine plasma concentration, suggesting inadequate de novo synthesis secondary to decreased citrulline production. Other studies in adults have proved that a state of severe inflammation greatly increases protein breakdown and arginase activity which decreases citrulline and de novo arginine production.7 These metabolic alterations greatly limit arginine availability, especially for NO production by the NOS3 enzyme. All of this explains why citrulline production, as a source of de novo arginine production, can be considered an important metabolic pathway and one of our main analytical objectives to be analyzed when starting the study. On the one hand, small bowel ischemia is related to acute reduction of enterocyte mass and loss of gut barrier function by epithelial lifting of villi. On the other hand, SIRS and sepsis could be linked to an acute dysfunction of enterocytes without enterocyte mass reduction.6
Increased arginine decline in the first 12h after admission is correlated with a longer stay in PICU, a greater number of complications and a greater increase in acute phase reactants such as CRP and PCT, at 3 days. This is similar to what Dick A van Waardenburg et al. published in Am J Clin Nutr 200712 (plasma concentrations of arginine and citrulline are low during the acute phase of critical illness in children and normalize again during recovery and they are strongly related to the severity of inflammation indicated by plasma CRP concentrations). Besides, plasma citrulline that is still lowered on day 7 is associated with increased CRP and PCT at 24h, longer duration of MV and PICU stay, as well as a higher incidence of complications.
The importance of the gut is further supported by the fact that diminished renal function does not affect de novo arginine production, even though the kidney is the main site of arginine production from citrulline.13 These metabolic alterations contribute to reductions in citrulline and arginine availability and offer the potential possibility for intervention to restore arginine metabolism in SIRS.
All these data indicate that inflammation induces changes in the amino acid profile, which are more pronounced/deeper when inflammation is severe. The influence of SIRS and acute renal failure on plasma citrulline concentration and the value of this concentration as an indicator of acute intestinal failure in critically ill patients must be further evaluated. According to our data, citrulline supplementation, as precursor of arginine, can enhance systemic citrulline and arginine availability in critically ill children and help to reduce the early decrease in arginine levels at 12h that is correlated with a worse outcome; however, further investigation is required to determine whether exogenous citrulline can actually support arginine metabolism in SIRS.14,15
ConclusionsThere are decreased levels of arginine and citrulline during the acute phase of pediatric critically ill patients, with delayed recovery from 3rd and 7th day onwards, respectively. There is a correlation between greater decrease with worse outcomes, longer stay in PICU and higher serum acute phase reactants (CRP, PCT). These results represent another way to demonstrate the inflammatory response in critically ill patients and the potential usefulness of arginine and citrulline as prognostic markers. Therefore, identifying ways to preserve intestinal integrity may be of paramount importance. Different peptides, such as glutamine, arginine and citrulline emerge as potential tools for modulation of intestinal inflammation and repair due to their roles in cellular proliferation, differentiation, migration, and survival.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Blasco-Alonso J, SánchezYáñez P, Rosa Camacho V, Camacho Alonso JM, Yahyaoui Macías R, Gil-Gómez R, et al. La cinética de la citrulina y la arginina y su valor como factor pronóstico en pacientes pediátricos críticamente enfermos. An Pediatr (Barc). 2015;83:257–263.
Presentation: Presentations of preliminary data at Spanish Society of Critical Care, (SECIP) in the National Congress held in Pamplona on May 2013.