Congenital lobar emphysema used to be treated surgically. Congenital lobar hyperinflation is the currently recommended term, as it involves pathologically healthy lung tissue, which is why conservative management may be an option. Four cases of diagnosed congenital lobar hyperinflation are presented in which conservative treatment was chosen due to their clinical stability. Their outcome has been satisfactory with progressively normal radiology.
El enfisema lobar congénito suele tratarse quirúrgicamente. Actualmente, se recomienda el término de hiperinsuflación lobar congénita, ya que se trata de un tejido pulmonar anatomopatológicamente sano, motivo por el que el manejo conservador puede ser una alternativa válida. Se presentan 4 casos diagnosticados de hiperinsuflación lobar congénita en los que se optó por el tratamiento conservador debido a su estabilidad clínica y en los que la evolución de los mismos ha sido satisfactoria con normalidad radiológica progresiva.
Congenital malformations of the lung and airways constitute a broad spectrum of developmental anomalies, some of which may remain asymptomatic and be discovered accidentally in imaging studies.1
Although they are not rare, their frequency is difficult to determine precisely; percentages from 7.5 to 18.7% have been published.2 They are responsible for a substantial amount of morbidity in neonates, infants, children and even adults and represent the second leading cause of early mortality among infants after anomalies of the cardiovascular system.3
Congenital lobar emphysema or hyperinflation is a malformation related to a cartilage or connective tissue anomaly (50%). This disorder gives rise to a ball-valve mechanism permitting inflow of air but obstructing outflow.2 It arises most frequently in the upper lobe of either lung and occasionally in the middle lobe of the right lung or in other areas, and can be observed from birth.4
Surgery (lobectomy) is usually considered the first-choice treatment in symptomatic patients.1
After reviewing clinical histories (with prior authorisation from the parents and/or guardians), we present four cases which were managed conservatively, not surgically, given the patients’ clinical stability.
Clinical casesPatient 1An infant aged 3 months, with no clinical history of interest, attended the accident and emergency department with signs of respiratory distress, preceded by catarrh of the upper air passages on the previous days. The chest X-ray and CT scan showed an area of lobar hyperinflation at the left upper lobe (LUL) (Fig. 1).
Once the manifestations of acute respiratory infection had been resolved, she became asymptomatic, and it was decided to pursue conservative treatment with follow-up at a paediatric respiratory clinic.
Her evolution was satisfactory, with no further acute clinical exacerbations. Chest radiology was normal at age 6. She remains asymptomatic at 17, with normal respiratory function tests.
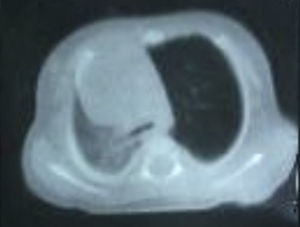
Patient 2Newborn male aged 20 days, with no personal history of interest, attended the accident and emergency department after 24h of presenting symptoms characterised by weakness, vomiting, fever, and test results compatible with urinary tract infection. No respiratory symptoms reported apart from noisy breathing. Clinically stable, with adequate tolerance to oral intake and no respiratory compromise, and hypoventilation observed in upper left field. A chest X-ray showed hyperinflation of the left hemithorax with contralateral mediastinal shift (Fig. 2); the CT scan confirmed a marked LUL hyperinflation with constriction of vessels compatible with obstructive emphysema, indicative of lobar emphysema of the LUL.
The study was completed by performing flexible bronchoscopy, revealing a left main bronchus that was structurally and functionally normal, except at the distal level (carina at bifurcation of LUL and lingula), where a collapse of the bronchial lumen – estimated at 80–90% – was observed, due to redundant mucosa and substantial malacia. Given the absence of respiratory effects on the patient, after resolving the infectious process which motivated his admission it was decided to discharge him from hospital with conservative treatment of the emphysema and follow-up of his clinical evolution. The patient is currently 7 months old, is asymptomatic and attends the paediatric respiratory clinic for periodic checkups.
Patient 3Infant aged 3 months, with no personal or family history of interest, attended the accident and emergency department after 5 days of showing symptoms consisting of frequent congested cough, fever of up to 38.8°C in the last 48h, increasing respiratory distress and refusal of food in the last few hours. In the examination, the most notable finding was a tachypnoea of 60bpm with sub- and intercostal retractions and with wheezing and SaO2 to ambient air of 92%; respiratory auscultation revealed global hypoventilation with crackling in both pulmonary fields. The chest X-ray showed widespread hyperinflation in both lungs and LUL, with herniation across the midline. Nasal mucus tested positive for RSV so the patient was admitted with a diagnosis of bronchiolitis and suspected congenital lobar hyperinflation; and evolved favourably with conservative treatment.
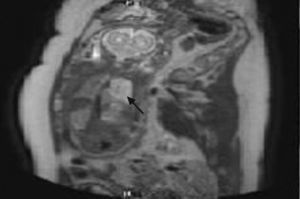
The study was completed with chest CT scan (Fig. 3) and flexible bronchoscopy, revealing marked obstruction of a bronchus in the LUL (estimated at 80% of the lumen) due to malacia of the wall, with subsegmental bronchi also malacic. Non-specific signs of bronchial hyperreactivity were observed throughout the whole examination. Given the patient's respiratory stability, the option chosen was conservative management. During follow-up (current age: 10 months), there have been no incidents and the patient is asymptomatic.
Patient 4Infant aged 24 days, with no personal history of interest, diagnosed prenatally (at 19 weeks) (Fig. 4) with suspected cystic lung disease, attending scheduled appointment at the paediatric respiratory clinic to complete study. The infant was asymptomatic, and the only notable result of the examination was a slight hypoventilation in the left hemithorax on auscultation. The chest X-ray showed increased density at the left parahilar level, and the chest CT scan lung hyperlucency in much of the LUL (apical posterior and anterior segments, not affecting the lingula), with reduction in the number and diameter of vessels, findings consistent with obstructive emphysema, the first diagnostic possibility considered being congenital lobar hyperinflation. At the age of 6 months the patient's clinical situation is stable, with no respiratory compromise.
DiscussionCongenital lobar emphysema, more properly called congenital lobar hyperinflation, is probably the result of a bronchial anomaly that gives rise to a ball valve effect in which air can flow into the parenchyma of the affected lobe but the outflow of that air is impeded.1,3 The term “hyperinflation” is preferred rather than “emphysema” as it is a pulmonary parenchyma that in most cases is healthy; that is, an area of pulmonary parenchyma in which the only disorder is hyperinflation but that is histologically normal. Emphysema is an anatomical/pathological term and is therefore confined to those cases in which the parenchyma is affected.
The symptoms tend to manifest themselves at birth in 33% of cases, during the first month of life in 50% and the majority by the age of one. The rest may manifest themselves as chance findings.5,6 It is diagnosed by radiological means, chest CT scan being the method of choice, as it enables possible associated mediastinal anomalies responsible for the condition to be excluded. The technique of multislice CT with virtual bronchoscopic reconstruction has been used with good results in some cases,7 although flexible bronchoscopy currently remains the most reliable diagnostic procedure for identifying some of the possible anomalies, such as bronchomalacias, that can cause localised hyperinflation.8
At present, despite the more widespread use of prenatal diagnostic tests (ultrasound scans and especially magnetic resonance imaging), it remains very difficult to identify and in most cases diagnosis is postnatal, since it requires ventilation to manifest itself.9
As for treatment, lobectomy of the affected lobe has traditionally been considered the treatment of choice in these patients.10 Although it is true that surgical intervention is curative, in cases that are not life-threatening and where the patient is clinically stable conservative treatment is an option, especially if the bronchoscopic examination is normal.11–13 This procedure can be followed by gradual resolution of the condition, and in the long term lung growth is usually normal.14
Broncho-pulmonary anomalies vary widely in their clinical expression, and up till now surgical treatment has been the first therapeutic option.
In the case of “congenital lobar emphysema”, given normal pulmonary parenchyma, if the patient is asymptomatic or the respiratory exacerbations are adequately tolerated, conservative management should be the treatment of choice, although it is true that some cases are real emergencies and urgent surgical treatment would therefore be justified.
“Congenital lobar emphysema” as a term coupled with lobectomy remains a subject of debate.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Hermoso Torregrosa C, Moreno Medinilla E, Pérez Ruiz E, Caro Aguilera P, Pérez Frías FJ. Hiperinsuflación lobar congénita: manejo conservador como alternativa terapéutica. An Pediatr (Barc). 2014;81:45–48.