We present the case of a male infant aged 2 months who had been delivered vaginally in a public hospital at 36 weeks’ gestation, born to an untreated HIV-positive mother who was a drug user, had not received prenatal care and had developed a painless perineal chancre in the second trimester of pregnancy that resolved spontaneously within 2 weeks, with the mother not showing to the follow-up visit; the venereal disease research laboratory test (VDRL) was nonreactive at the time of delivery. The boy was asymptomatic at birth.
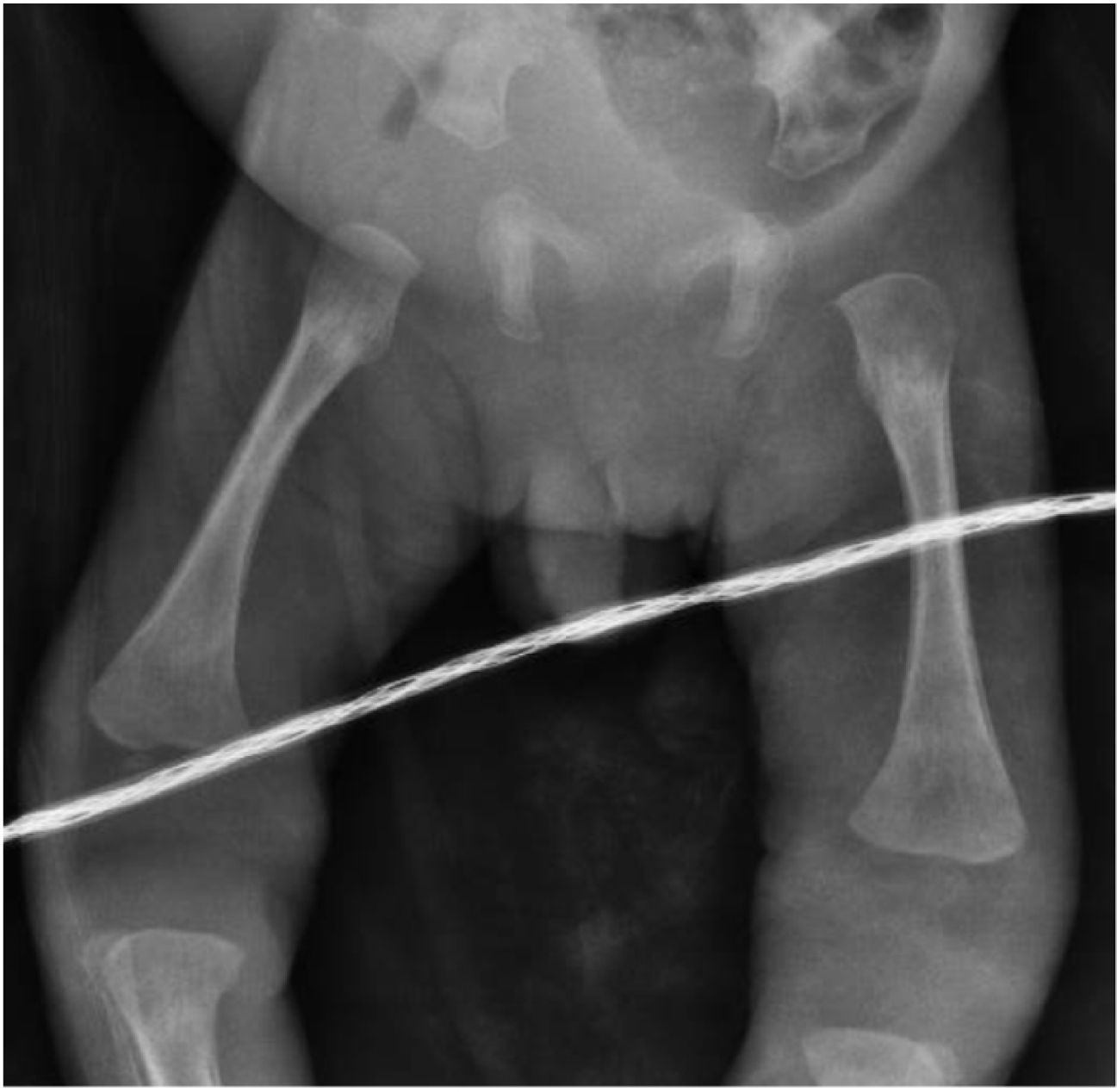
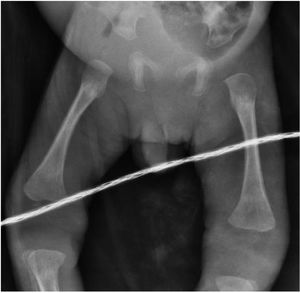
He was admitted due to bloody nasal discharge and dermal lesions with onset one month prior. The physical examination detected features suggestive of septic shock (heart rate, 180 bpm; respiratory rate, 50 bpm; temperature, 38.8°C), a low weight of 2.68kg (below the 3rd percentile, with a z-score of −5.5), bloody nasal discharge, cheilitis and generalised macular exanthema with hyperkeratosis and desquamation (Fig. 1) predominantly in the face, trunk and extremities and with palmoplantar involvement (Fig. 2), mild crepitus in the chest and abdomen and hepatosplenomegaly in absence of clinical features of ascites.
The findings of blood tests were reactive chemiluminescent immunoassay for detection of anti-Treponema pallidum antibodies (25.8 S/CO), anaemia (haemoglobin, 10g/dL), a leukocyte count of 9.4×103/mL, thrombocytopenia (95×103/mL), hypoglycaemia (58mg/dL), transaminasaemia (AST 554 U/L, ALT 135 U/L) with direct hyperbilirubinaemia (3.7mg/dL), hypoalbuminaemia (1.3g/dL) and an undetectable HIV viral load, and the radiographs evinced periostitis in the long bones (Fig. 3). Examination of a lumbar puncture sample revealed hypoglycorrhachia (28mg/dL), hyperproteinorrhachia (59mg/dL), sin pleocytosis y VDRL reactivo. The VDRL test in the mother was reactive (1:64).
The patient received a diagnosis of neurosyphilis and septic shock and was admitted for intensive care with initiation of a 14-day course of aqueous crystalline penicillin G sodium (200 000 IU/kg/day) that achieved a favourable outcome, so the patient was discharged due to clinical improvement.
Depending on the timing of transmission, syphilis can cause foetal death, prematurity or low birth weight.1,2 The case presented here demonstrates that no genital lesion should be neglected during gestation as it can have severe consequences for the offspring.
Conflicts of interestThe authors have no conflicts of interest to declare.
Informed consentWe obtained informed consent in writing from the parents for the publication of clinical information and images. A copy has been made available to the editor of the journal for review.