Poisonings account for 0.3% of pediatric emergency department visits,1 and pharmaceuticals are the substances most frequently involved in these episodes. Vitamin D is the most widely used dietary supplement in the pediatric age group.2 In March 2019, the Spanish Agency of Medicines and Medical Devices (AEMPS) warned of an increase in the cases of intoxication associated with preparations containing cholecalciferol in children and calcifediol in adults notified to the Spanish pharmacovigilance system, attributed to errors in the prescribing, dispensation or administration of the drug.3
We conducted a retrospective descriptive study in the pediatric emergency department of a tertiary care hospital that included patients aged 0–16 years treated between January 2010 and December 2024 for excessive vitamin D intake who were identified through the review of electronic health records. The study was approved by the Research Ethics Committee of the hospital. We analyzed epidemiological characteristics, clinical manifestations and the management in the emergency department.
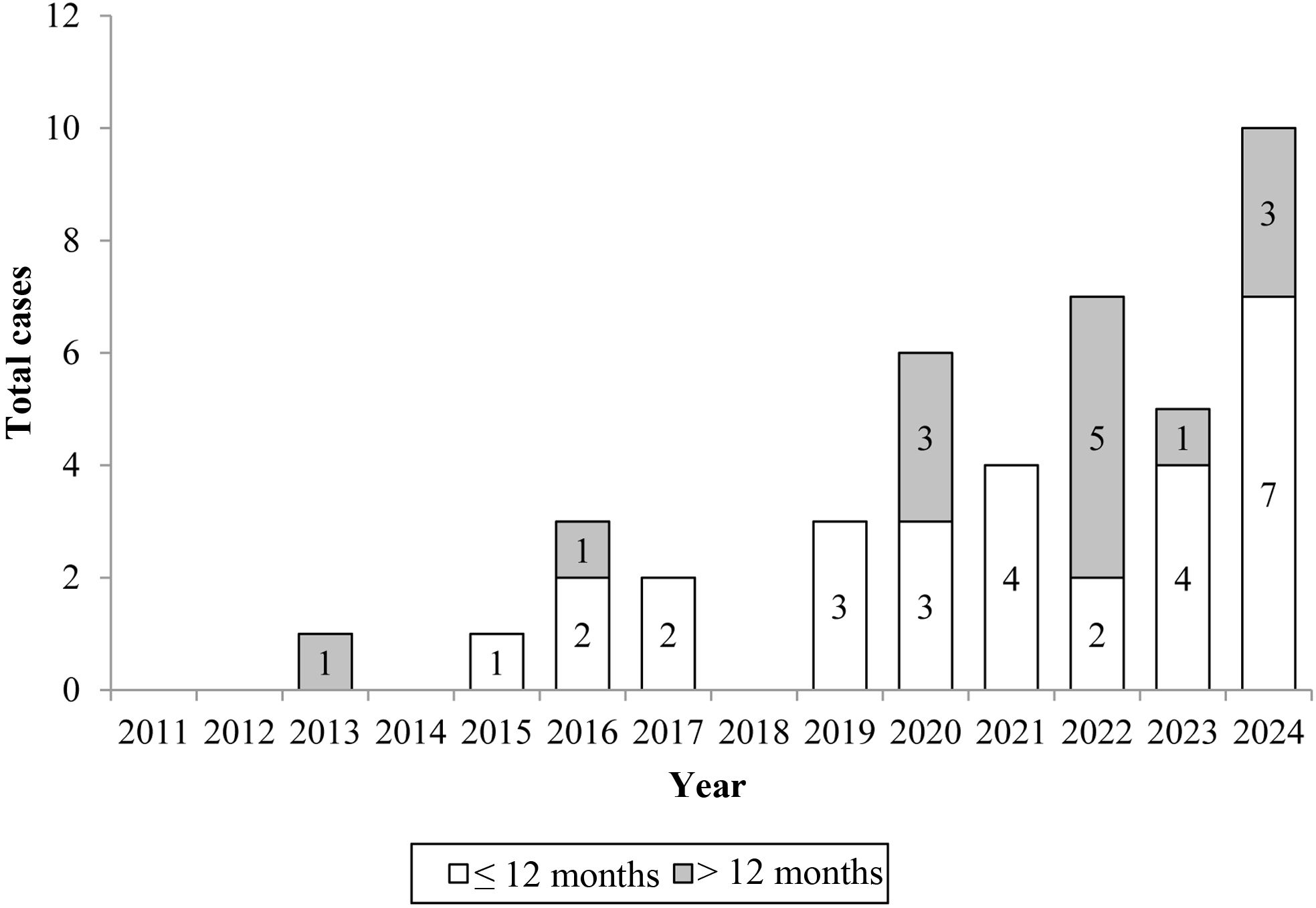
The sample included 42 patients (54.2% male, 45.2% female) with a median age of 4.2 months (IQR, 1.2–24). We found an increase in cases in the last 5 years, peaking in 2024, and as well as an increasing frequency in patients aged more than 12 months (Fig. 1). In 54.2%, the excessive intake was attributed to dosing errors made by the caregivers, in the remaining cases, the excessive intake was considered accidental. A majority of the involved formulations were suspensions (90.2%), the rest were capsules. Twenty-five patients (59.2%) received a single dose (median, 1227.2 IU/kg; IQR, 300–2381) and 17 (40.2%) repeated doses (median cumulative dose, 7211.2 IU/kg; IQR, 5142.2–15 151.2; median daily dose, 505.2 IU/kg; IQR, 190.2–952.2). In the latter group, the time elapsed to the emergency department visit was 21 days (IQR, 8–30), and the median age was lower compared to the single-dose group (2.2 vs 12 months; P = .228). Of all patients, 95.2% were asymptomatic, one had abdominal pain (2.2%) and two vomiting (4.2%).
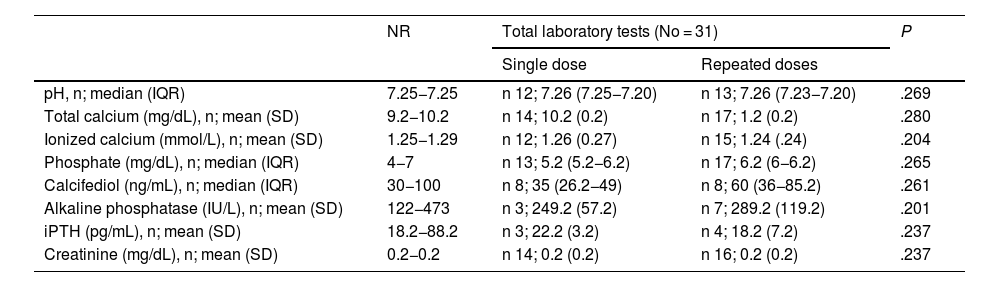
Laboratory tests were done in 31 patients (73.2%). The total calcium level exceeded the upper limit of normal (>10.2 mg/dL) in 6 cases (19.2%), and the ionized calcium level (>1.29 mmol/L) in 20 cases (64.2%), with the latter being significantly more elevated in patients who received repeated doses. The level of calcifediol was measured in 16 patients, with abnormal results (>100 ng/mL) in two (12.2%). The level of intact parathyroid hormone was measured in seven patients (22.2%), and was below normal (<18.2 pg/mL) in two of them (28.2%). None of the patients had elevated serum creatinine levels (Table 1).
Salient laboratory findings in cases of excessive vitamin D intake.
| NR | Total laboratory tests (No = 31) | P | ||
|---|---|---|---|---|
| Single dose | Repeated doses | |||
| pH, n; median (IQR) | 7.25−7.25 | n 12; 7.26 (7.25−7.20) | n 13; 7.26 (7.23−7.20) | .269 |
| Total calcium (mg/dL), n; mean (SD) | 9.2−10.2 | n 14; 10.2 (0.2) | n 17; 1.2 (0.2) | .280 |
| Ionized calcium (mmol/L), n; mean (SD) | 1.25−1.29 | n 12; 1.26 (0.27) | n 15; 1.24 (.24) | .204 |
| Phosphate (mg/dL), n; median (IQR) | 4−7 | n 13; 5.2 (5.2−6.2) | n 17; 6.2 (6−6.2) | .265 |
| Calcifediol (ng/mL), n; median (IQR) | 30−100 | n 8; 35 (26.2−49) | n 8; 60 (36−85.2) | .261 |
| Alkaline phosphatase (IU/L), n; mean (SD) | 122−473 | n 3; 249.2 (57.2) | n 7; 289.2 (119.2) | .201 |
| iPTH (pg/mL), n; mean (SD) | 18.2−88.2 | n 3; 22.2 (3.2) | n 4; 18.2 (7.2) | .237 |
| Creatinine (mg/dL), n; mean (SD) | 0.2−0.2 | n 14; 0.2 (0.2) | n 16; 0.2 (0.2) | .237 |
Abbreviations: iPTH, intact parathyroid hormone; NR, normal range.
An electrocardiogram was performed in 16 patients, all with normal findings. The care team contacted the Instituto Nacional de Toxicología (INT, National Toxicology Institute) in 20 cases (47.2%). Six patients received activated charcoal (14.2%) and three fluid therapy (7.2%); one of the latter, an infant who had accidentally ingested 20 000 IU, was the only patient admitted to hospital. The discharge recommendations included discontinuation of vitamin D supplementation in 30 patients (71.2%), avoiding exposure to sunlight in nine (21.2%) and restricting dairy intake in five (11.2%). An outpatient ultrasound scan was ordered in nine cases (21.2%), with no evidence of nephrocalcinosis in any.
Excessive vitamin D intake is rare in children, although notifications of vitamin D overdose have increased in recent years.4 This may be due to lifestyle changes in the pediatric population, for instance, the decreased exposure to sunlight, which increases the risk of vitamin D deficiency and rickets.5 In this context, an increase in the cases of accidental exposure is to be expected, especially among older children. In our emergency department, visits related to excessive vitamin D intake doubled in 2024 compared to 2023, with a considerable increase in children aged more than 12 months. Some of the potential contributors are the wide availability of oral formulations, the active screening for vitamin D deficiency in primary care and the scarcity of public information on the safe intake range. In older children, other potential contributors would include the greater number of prescriptions—frequently with no basis on the current evidence—and the increasing frequency with which measurement of calcifediol levels is ordered in the healthy population,6 despite the fact that this intervention is not recommended by clinical guidelines.
There is no clear consensus regarding the threshold for toxicity in the dosing of vitamin D in the pediatric population5 nor the optimal management of vitamin D toxicity. In nearly half of the cases in this series, providers consulted with the INT, whose recommendations were heterogeneous, especially in relation to the span of time the treatment should be suspended. Although most patients were asymptomatic and were managed conservatively, vitamin D toxicity can cause severe complications, such as hypercalcemia or nephrocalcinosis, especially in children with CYP24A1 gene variants, who are more susceptible to it, even at lower doses.
In conclusion, we want to alert to the increase in vitamin D dosing errors in children and highlight the need to establish consensus-based management protocols.