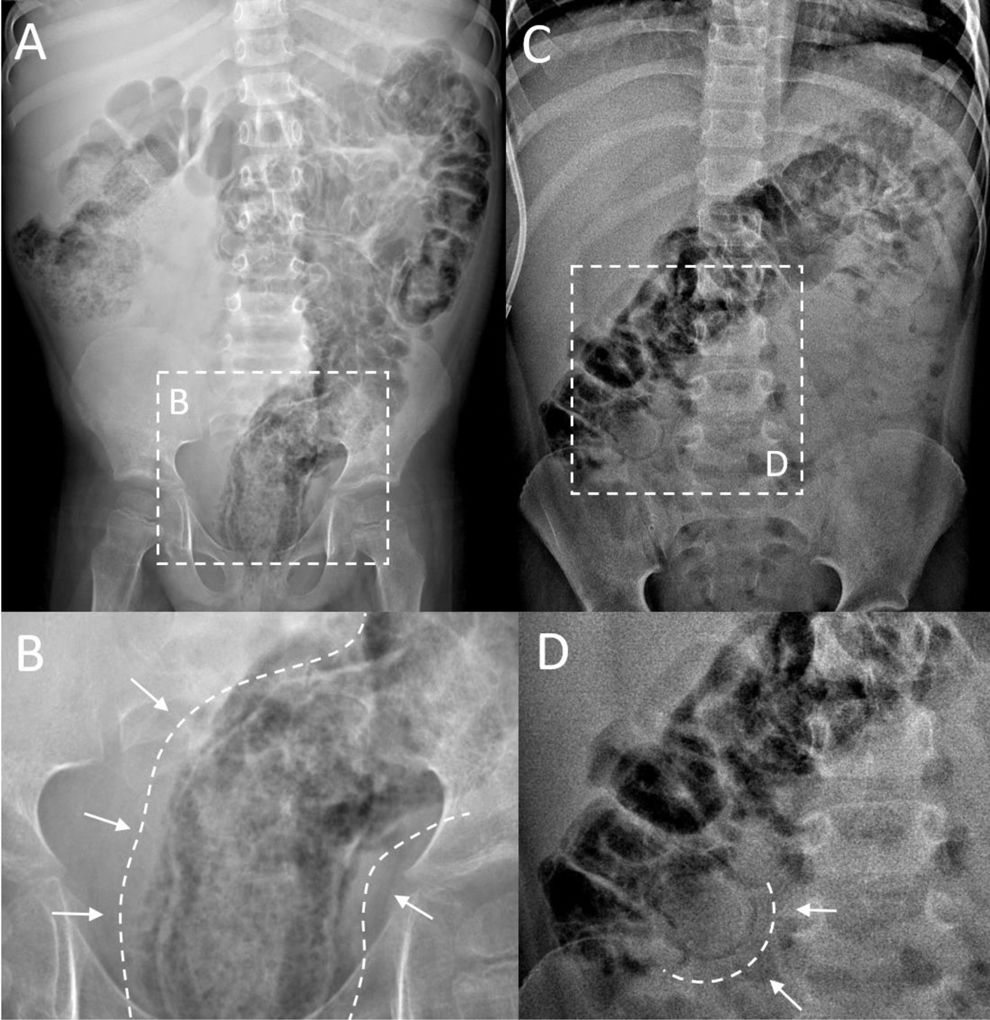
We present two cases of mural intestinal pneumatosis (IP) diagnosed by means of plain abdominal radiography in hematopoietic stem cell transplantation (HSCT) recipients receiving immunosuppressive therapy for acute graft-versus-host disease (aGVHD) with gastrointestinal involvement. The first was a boy aged 5 years admitted 51 days post HSCT with aGVHD that had responded favorably to treatment with mycophenolate, steroids and extracorporeal photopheresis and presented with abrupt abdominal distension (Fig. 1A and B). The second was a boy aged 6 years on day 71 following a second HSCT in treatment with mycophenolate and steroids, who presented with constipation and abdominal pain in whom the physical examination revealed abdominal distension (Fig. 1C and D).
Plain radiograph of the abdomen. First patient: (A) extensive pneumatosis, more apparent in the descending and sigmoid colon and rectum; (B) expanded image of the pelvic region with clear visualization of dark streaks of air running parallel to the rectal lumen, compatible with intramural gas. Second patient: (C) involvement of hypochondrium and epigastric region characterized by distension of the intestinal lumen superimposed to multiple, less apparent features indicative of intramural gas; (D) detail showing a round streak of air corresponding to a more clearly defined area of mural pneumatosis.
Intestinal pneumatosis consists in the presence of gas in the intestinal wall. In a neonate, it is a sign associated with necrotizing enterocolitis, but in older children it is a rare finding whose etiology is not well known. Its clinical presentation varies widely, ranging from the absence of symptoms to gastrointestinal bleeding. There is evidence of an increased incidence in children who undergo HSCT, patients receiving immunosuppressive treatment and children with neurodevelopmental disorders.1 Cases of IP have also been described in adults receiving steroids as monotherapy.2,3 In most cases, the prognosis of IP is good and its management is conservative.1