Our organizational model allows an annual running of 1000 liver transplants. Paediatric liver transplantation constitutes 5% of such activity and provides, in children with severe, progressive and irreversible liver disease, a 1-year survival of 90% and more than 80% after 15 years of follow-up. The main indication is biliary atresia followed by metabolic liver disease and acute liver failure. Around half of the procedures are performed in children under 2 years and 25–30% in the first year of life.
The waiting list remains at around 35 patients, with an average of 100 patients enrolled annually and 60 of them finally transplanted after an average of 136.3 days on the waiting list. The prioritization of the candidates uses the PELD as an objective tool for decision-making. However, the progressive ageing of donors, with a profile increasingly different from the requirements of the paediatric patients included in the waiting list, requires strategies such as living donor liver transplantation and the split liver transplantation, to increase the probability of transplant while reducing both time and mortality on the waiting list at the same time.
Paediatric intestinal transplantation registers a low indication but involves strict requirements that outline a very uncommon donor in our country which, together with the absence of alternatives that outweigh the impact of these difficulties, penalizes the chances of transplant for these patients.
Nuestro modelo organizativo posibilita la realización anual de 1.000 trasplantes hepáticos, de los cuales el trasplante hepático pediátrico constituye el 5% y proporciona, en niños con hepatopatía grave, progresiva e irreversible, una supervivencia del 90% al año y superior al 80% a los 15 años de seguimiento. La principal indicación es la atresia de vías biliares seguida de hepatopatías metabólicas e insuficiencia hepática aguda, realizándose el 50% de los procedimientos en menores de 2 años y el 25–30% en el primer año de vida.
La lista de espera se mantiene en torno a los 35 pacientes, con un promedio de 100 pacientes incluidos anualmente y 60 trasplantados tras un tiempo medio de espera de 136,3 días. La priorización de los candidatos utiliza el PELD como herramienta objetiva de apoyo en la toma de decisiones. No obstante, el progresivo envejecimiento de los donantes, con un perfil cada vez más alejado de los requerimientos de los pacientes infantiles incluidos en lista de espera, precisa impulsar estrategias como el trasplante hepático de donante vivo y la modalidad split, para incrementar las probabilidades de trasplante reduciendo la mortalidad en lista de espera y el tiempo de permanencia en la misma.
El trasplante intestinal/multivisceral pediátrico registra una baja indicación pero conlleva unos requisitos que perfilan un donante muy infrecuente en nuestro país, lo que, unido a la ausencia de alternativas que contrarresten el impacto negativo de estas dificultades, lastra las probabilidades de trasplante de estos pacientes.
The Spanish organizational structure for organ donation and transplantation has allowed Spain to achieve the highest rate of donation worldwide continuously since the early 1990s, exceeding 35 donors per million population (pmp).1 As a direct consequence, between 1000 and 1100 liver transplants can be performed in Spain each year, reaching a rate of 23 procedures pmp, one of the highest in the world.2,3 Among these procedures, paediatric liver transplantation accounts for 5% of the activity nationwide, with a mean of 60 transplants per year.
We ought to note that paediatric liver transplantation is an infrequent procedure due to both the low incidence of the diseases for which it is indicated and the reduced availability of donors that are suitable matches for the recipients on the waiting list, as the donor pool has been ageing on a sustained basis. This becomes evident when we analyze the increase in the mean age of donors in our country, which has practically doubled from 36 to 60 years over the past two decades. In this regard, data from 2014 revealed that only 1.5% of registered donors in Spain were younger than 15 years.1 The comorbidities present in current donors combined with the ageing trend pose challenges to donor–recipient matching, and this has the most negative impact on the paediatric population.
In order to alleviate the negative repercussions that result from the particularities of this procedure, the Consejo Interterritorial del Sistema Nacional de Salud (Interterritorial Council of the National Health System) considers the sites that perform it reference centres, departments and units (Centros, Servicios y Unidades de Referencia [CSURs]). The purpose of this designation is to guarantee equity of access, regardless of the place of residence, and quality services to individuals with rare and complex diseases that require highly specialized care, which in turn necessitates the concentration of patients and health care resources.
Indications for transplantation and waiting list managementPaediatric liver transplantation is indicated for severe liver disease for which there is no other effective treatment when it has been determined that performing the transplant can improve survival and quality of life compared to not performing it, an assessment that requires a precise diagnosis.4,5
Good outcomes in the post-transplant survival of children have led to a shift in the approach to the management of severe paediatric liver disease.6,7 In chronic cases, the risk of death due to liver disease is not the only determinant in the decision to transplant or not, and another factor under consideration is the severe impairment of quality of life, due to a pathology for which there is no other treatment of comparable efficacy and sufficiently developed, that would justify the risk of early death associated with transplantation.
Thus, it is essential that the risk of death be assessed in order to determine the optimal timing for transplantation, anticipating the development of predictable severe complications, and also to assign degrees of priority to the patients on the waiting list managed by each site.
Activity data show that around 5% of patients on the waiting list for a liver transplant belong to the paediatric age group, a percentage that is similar to the one found in the total population of transplanted patients, which shows that the probability of receiving a transplant is maintained in this age group in spite of its particular challenges.
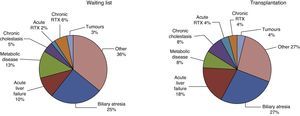
The childhood diseases that may be treated with a liver transplant mainly include cholestasis, metabolic disorders, cirrhosis and severe acute liver failure. The main indication for liver transplantation in children is biliary atresia, which accounts for 25% of the patients in the waiting lists in Spain. Metabolic liver disease accounts for the second highest number of cases included in the waiting lists, followed by acute liver failure, accounting for 13% and 10% of transplant candidates, respectively (Fig. 1).
Similarly, if we analyze the transplantations performed in 2014 (Fig. 1), biliary atresia remained the most frequent disease in children that underwent liver transplantation in Spain (27%), although acute liver failure had become the second most frequent indication (18%), surpassing metabolic diseases (8%). This change was promoted by the prioritization of those cases, which increased their chances of receiving a transplant. Approximately 3–4% of transplants were performed as part of the treatment of non-resectable liver tumours, benign as well as malignant, with both categories accounting for a similar proportion of the patients on the waiting list.
As for the age of paediatric patients on the waiting list and who received transplants, about 50% of liver transplants are performed in children aged less than 2 years, and 25–30% are performed in the first twelve months of life.6
The most important consideration in prioritizing candidates for paediatric liver transplantation in a transplantation centre is severity of illness. In this decision-making framework, the Paediatric End-Stage Liver Disease score (PELD) is the score used most commonly, as it estimates the probability of death within three months in children with chronic liver disease that are on the transplant waiting list. Thus, the PELD score can be a helpful tool for decision-making, as it allows the allocation of donors to recipients based on an objective parameter. Furthermore, prioritizing patients with more severe disease can reduce mortality among patients on the waiting list without negatively impacting post-transplant outcomes in the medium and long term.8
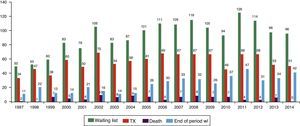
The size of the waiting list has remained fairly stable in the last decade, staying—in terms of prevalence—at about 35 patients in the past 5 years, with an average of 100 patients listed throughout the year of which a mean of 60 patients per year receive a transplant (Fig. 2).
Unfortunately, it is important to mention that some of these patients (six to seven a year) die while awaiting transplantation, although no deaths were recorded in 2014, something that was made possible by alternatives to conventional liver transplantation (living-donor transplantation and split liver transplantation) that increase the probability of receiving a transplant in these patients.1
The mean waiting time for paediatric patients that received a transplant was 106.8 days in 2014, considerably shorter than the waiting time documented for the adult population (136.3 days), a fact that is also due to the positive impact on children of living-donor transplantation, which increases their transplant options.1
The comparative management of the liver transplant waiting list is balanced as it concerns the paediatric population, as children account for 4.5% of the patients on the waiting list and for a similar proportion of the transplanted patients, which is 4.8%.1
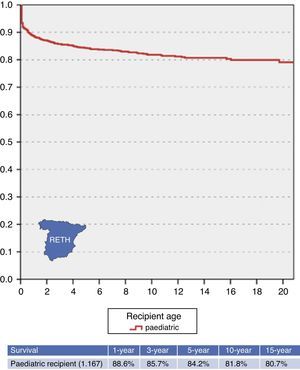
Transplant outcomes: post-transplant morbidity and mortalityAt present, paediatric liver transplantation is a well-established therapeutic option in the paediatric population that has completely changed the life expectancy and quality of life in children with severe, progressive and irreversible liver disease. This can be assessed by analysing the excellent outcomes of transplantation, with a 1-year survival rate of about 90% and survival rates of more than 80% at 15 years of follow-up (Fig. 3).
In paediatric patients, surviving the first year post transplant has been identified as a factor associated with long-term survival, with less than 10% mortality in the subsequent 10 years (Fig. 3). Despite the complexity of the process that follows liver transplantation, the associated morbidity and the ever-present risk of severe complications, once the immediate postoperative period is through, the prognosis and quality of life of these patients are generally very good.
To assess the magnitude and evolution of these outcomes, we have at our disposal the statistical analyses offered by the Registro Español de Trasplante Hepático (Spanish Registry of Liver Transplantations [RETH]),6 a tool that is very useful, as it systematically pools the information of all cases nationwide, gathering data on the characteristics of donors and recipients, short-term technical aspects and immunosuppression and, what is more important, updated information on the graft and recipient outcomes, documenting the cause of death or of retransplantation when applicable. The RETH currently holds data for the 1167 paediatric liver transplantations that have been performed in Spain up to December 2014.
The data analyzed by the RETH6 (Fig. 3) show that the 5- and 10-year survival are 84.2% and 81.8%, respectively, higher than the survival rates documented in adults, which may be thanks to specific characteristics of the paediatric population that can be explanatory factors for this fact.
Advances in surgical technique, the increased efficacy of immunosuppression, and the improved control of infections and other post-transplant complications have contributed to these results. In broad terms, the success of transplantation is based on specific key factors, such as a correct indication, the assessment of the optimal timing for the procedure, and the appropriate management and followup of the patient before and after the intervention.9,10
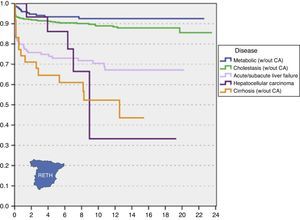
However, not all diseases that are indications for liver transplantation carry the same prognosis nor have the same morbidity and mortality outcomes.11–16 As can be seen in Fig. 4, the indication for transplantation is a determinant for survival, as survival rates are significantly higher for metabolic disorders and cholestasis compared to cirrhosis and liver tumours, with an intermediate prognosis for acute liver failure.
The presence of extrahepatic involvement has a considerable impact on survival. Thus, in 80% of recipients the disease is confined to the liver, and they have a full recovery following transplantation. However, in 20% of cases the disease recurs in the graft, leading to poorer outcomes (as may happen in cases of viral or autoimmune hepatitis, tumours, and syndromes with multiple organ involvement).
In considering the overall outcomes in terms of the need for retransplantation, we ought to highlight that this complication is more frequent in the paediatric population, in which the rate reaches 16.6%, double the rate documented in adults, which is approximately 8%. If we break down the rate of retransplantation by age subsets in the paediatric population, there are no significant differences, and a similar rate is found in children aged less than 2 years compared to children aged 2–15 years (Table 1).
Outcomes of initial transplant in paediatric recipients by indication.
| Outcome of initial transplant by type of disease | ||
|---|---|---|
| Retransplantation | Total | |
| Acute/subacute liver failure | 28 | 150 |
| 18.7% | 100% | |
| Congenital biliary tract diseases | 89 | 567 |
| 15.7% | 100% | |
| Alagille syndrome | 7 | 58 |
| 12.1% | 100% | |
| Malignant tumours | 5 | 64 |
| 7.8% | 100% | |
| Alpha-1-antitrypsin deficiency | 5 | 31 |
| 16.1% | 100% | |
| Byler disease | 6 | 31 |
| 19.4 | 100% | |
| Overall paediatric: 0–15 years | 194 | 1167 |
| 16.6% | 100% | |
| 0–2 years | 103 | 616 |
| 16.7% | 100% | |
| 3–15 years | 91 | 551 |
| 16.5% | 100% | |
The most salient finding when we assessed the rates of retransplantation in the paediatric population by recipient disease was that the rates of retransplantation for the most frequent indications exceed 15% (18.7% of transplants for acute liver failure and 15.7% of transplants for congenital biliary tract disease). The rates of retransplantation for the remaining and less frequent indications exceed 8%.
Starting with the most frequent diseases (congenital biliary tract disease and acute or subacute liver failure), technical complications constitute the main cause for retransplantation, leading to more than 40% of retransplantations for these diseases and to the higher early mortality that we referred to earlier on. Following in frequency are transplant rejection, which is the cause of 33% of retransplantations, and primary graft dysfunction, which accounts for 15–20% of cases. Table 2 also shows the causes for retransplantation in the remaining diseases, although this distribution must be interpreted with caution considering the low number of cases.
Retransplantation in paediatric recipients by indication.
| Causes for retransplantation after initial transplant for the most frequent diseases | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Acute/subacute liver failure | Congenital biliary diseases | Alagille syndrome | Malignant tumours | α1-antitrypsin deficiency. | Byler disease | |||||||
| n | % | n | % | n | % | n | % | n | % | n | % | |
| Technical complication | 11 | 40.7 | 37 | 42 | 1 | 14.3 | 3 | 60 | 3 | 60 | 1 | 16.7 |
| Rejection | 9 | 33.4 | 29 | 33 | 2 | 28.6 | – | – | 1 | 20 | 2 | 33.3 |
| Primary graft dysfunction | 4 | 14.8 | 17 | 19.4 | 3 | 42.8 | 1 | 20 | 1 | 20 | 3 | 50 |
| Recurrence of underlying disease | 1 | 3.7 | – | – | – | – | – | – | – | – | – | – |
| De novo hepatitis | – | – | – | – | – | – | – | – | – | – | – | – |
| De novo tumour | – | – | – | – | – | – | – | – | – | – | – | – |
| Infection | – | – | 1 | 1.1 | – | – | – | – | – | – | – | – |
| Extrahepatic complication | – | – | 1 | 1.1 | – | – | – | – | – | – | – | – |
| Other | 2 | 7.4 | 3 | 3.4 | 1 | 14.3 | 1 | 20 | – | – | – | – |
| Total | 27 | 100 | 88 | 100 | 7 | 100 | 5 | 100 | 5 | 100 | 6 | 100 |
We previously mentioned the high survival rate of paediatric liver transplantation, as the 15-year survival exceeds 80%. However, despite the low mortality rate, analysing the causes of the documented deaths is useful to learn the predictable outcomes of transplanted patients.
In this regard, the information gathered by the RETH also allows the analysis of the main causes of death by the indication for transplantation, identifying the main risks for patients based on their underlying disease and aiding in preventing their development or minimizing their impact.
We must note that the survival rate is significantly lower for transplants treating acute liver failure, as there is a higher mortality during the postoperative period. The most frequent cause of death in this group of patients is infection—responsible for 26.3% of deaths—followed by extrahepatic complications (23.7%) and primary graft failure (13.2%) (Table 3). The main causes of death for other indications for transplantation can be identified based the data collected by the RETH.
Mortality in paediatric recipients by indication.
| Causes of death after initial transplant for the most frequent diseases | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Failure Sub/agudo | Biliary disease | Alagille syndrome | Malignant tumours | α1 antitrypsin deficiency | Byler disease | |||||||
| n | % | n | % | n | % | n | % | n | % | n | % | |
| Infection | 10 | 26.3 | 15 | 24.6 | 2 | 22.2 | 2 | 8.8 | 1 | 50 | – | – |
| Extrahepatic complication | 9 | 23.7 | 9 | 14.8 | 2 | 22.2 | 1 | 4.3 | – | – | 1 | 100 |
| Recurrence of underlying disease | – | – | – | – | – | – | 14 | 60.9 | – | – | – | – |
| De novo tumour | 1 | 2.6 | 3 | 4.9 | 1 | 11.1 | 1 | 4.3 | – | – | – | – |
| Technical complication | 1 | 2.6 | 8 | 13.1 | 1 | 11.1 | 1 | 4.3 | – | – | – | – |
| Perioperative death | 1 | 2.6 | 6 | 9.8 | 2 | 22.2 | – | – | – | – | – | – |
| Rejection | 3 | 7.9 | 3 | 4.9 | 1 | 11.1 | – | – | – | – | – | – |
| Primary graft dysfunction | 5 | 13.2 | 9 | 14.8 | – | – | – | – | 1 | 50 | – | – |
| De novo hepatitis | – | – | 1 | 1.6 | – | – | – | – | – | – | – | – |
| Multiple organ failure | 2 | 5.3 | 1 | 1.6 | – | – | – | – | – | – | – | – |
| Other | 6 | 15.8 | 6 | 9.8 | – | – | 4 | 17.4 | – | – | – | – |
| Total | 38 | 100 | 61 | 100 | 9 | 100 | 23 | 100 | 2 | 100 | 1 | 100 |
This category includes those strategies aimed at increasing the probability of transplantation and reducing both mortality and time spent on the waiting list, especially considering that the shift in the donor pool described above reduces the chances of receiving a transplant in paediatric candidates due to the difficulty of finding a donor of suitable age and size.
In response to this need, various strategies have been promoted in recent years both by the Organización Nacional de Trasplantes (National Transplant Organization [ONT]) and by paediatric transplantation programmes that necessarily include other transplantation modalities, such as living donor liver transplantation and split liver transplantation.
Living donor liver transplantationAccording to data from 2014, fourteen living donor liver transplantations were performed in children in Spain, accounting for 30% of all paediatric liver transplantations. Twenty-four living donor liver transplants were performed on average in the past 5 years, 70% of which were performed on paediatric patients. The data analysis performed by the RETH has shown that the survival of paediatric recipients of liver transplants is significantly higher in living-donor procedures.
This transplantation modality requires very stringent donor selection criteria and highly specialized technical skill to ensure the retrieval of a valid graft with minimum risk to the donor. The implantation procedure is more complicated than it is for cadaveric grafts, which may have an impact on the postoperative course.17–19
Split liver transplantationSplit liver transplantation allows the retrieval of two grafts from a single cadaveric donor. The right lobe is inserted in an adult and the left in either a child or a low-weight adult. This increases the number of available organs, especially for children, who constitute the majority of the left-lobe graft recipients, and can reduce—if the method is implemented extensively—the need for living-donor paediatric transplantations, as the adequate selection of donor and recipient leads to outcomes that are comparable to those of full liver transplants.20–23
Recently, a consensus between transplantation programmes has allowed the launching of the Plan Nacional para el Trasplante Hepático Tipo Split (National Plan for Split Liver Transplantation) with the purpose of implementing a national protocol for the maximization of liver grafts, to be obtained by the division of a suitable liver graft for its simultaneous implantation in two recipients, using the left lateral segments for paediatric recipients and the corresponding right extended lobes for adult recipients.
This initiative seeks to establish a fair and effective system that will contribute to reducing mortality in paediatric patients awaiting a liver transplant without negatively impacting adult candidates.
Intestinal and multivisceral transplantationAs happens with paediatric liver transplantation, intestinal/multivisceral transplantation is included in the group of procedures with a CSUR designation with the aim of guaranteeing equity of access and quality care for individuals with rare and complex pathologies the management of which requires a high degree of specialization and thus the concentration of patients and health care resources in a reduced number of facilities.
In Spain, the prevalence rate of indications for this extremely rare transplantation modality is 0.28 pmp, and the rate of transplantation is 0.17 pmp. Since 2009, the mean transplantation activity in Spain is nine cases a year, which corresponds to a 60% probability of intestinal/multivisceral transplantation for patients on the waiting list.
The analyzed data revealed that despite the low incidence in Spain of the diseases that are indications for intestinal/multivisceral transplantation, meeting the demand for this transplantation modality is a challenging task. This stems from the suitability criteria imposed by transplantation programmes in relation to specific characteristics (a narrow age and weight range, a short length of stay in the ICU, and the absence of hypotension or cardiac arrest, among others), setting a donor profile that is rarely found in Spain. These requirements, along with a lack of alternatives to counteract the impact of these difficulties—unlike what happens with liver transplantation—preclude increasing the probability of transplantation in these patients.
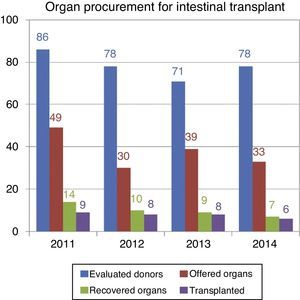
This situation came to light when we analyzed the donation data corresponding to year 2014: of the 78 donors that were assessed for intestinal/multivisceral transplantations, only 33 met the criteria to be offered to patients, and only six transplants were eventually performed. A similar pattern was observed in previous years, as can be seen in Fig. 5.
As a result of these difficulties, the mean time spent on the waiting list for an intestinal/multivisceral transplantation is 304 days, although it is considerably shorter than the 386 days documented for the adult age group.
To conclude, we would like to highlight that paediatric liver transplantation is a treatment option that offers excellent results in terms of survival and quality of life. However, the progressive ageing of the donor pool, with characteristics that diverge increasingly from the requirements for paediatric patients on the waiting list, calls for the promotion and reinforcement of alternatives that could increase the chances of survival and quality of life of these patients.
Conflict of interestThe authors declare no conflict of interest.
Please cite this article as: de la Rosa G, Matesanz R. El trasplante hepático e intestinal en la población pediátrica. An Pediatr (Barc). 2015;83:441.e1–441.e8.