The main aim of the study was to assess the effects of the recommended preventive programme in the population affected with sickle cell disease in primary care. The programme included, antibiotic prophylaxis, immunizations and health education, following the introduction of universal neonatal screening programme for sickle cell disease in the Community of Madrid.
Patients and methodsA cross-sectional observational study was performed with retrospective data collected from a cohort of newborns with sickle cell disease diagnosed by neonatal screening test in the Community of Madrid.
ResultsFrom the data obtained from a sample of 20 patients, it was found that 95% had been diagnosed by the newborn screening test performed between 5 and 13 days of life. The mean age was 39 months when the study was conducted. During follow-up, from primary care paediatric clinic, it was observed that the compliance for antibiotic prophylaxis was 90%, and the coverage for the official vaccination schedule was 85%. Specific vaccine coverage as a risk population was highly variable (85% for pneumococcal 23V, 50% for influenza, and 15% for hepatitis A). Health education only reached one in every four families.
ConclusionsAcceptable compliance with antibiotic prophylaxis was observed during the follow-up of patients with sickle cell disease in primary care, but a low coverage of routine immunisation, as well as specific immunisations. Coverage of health education was very low.
Improving these parameters would require greater coordination and involvement of primary care professionals so that these patients were followed up appropriately, and could be translated into a reduction of disease complications and an improvement in the quality of life of these patients.
El objetivo principal del estudio fue evaluar desde Atención Primaria la repercusión del programa preventivo recomendado en la población afectada de enfermedad falciforme: profilaxis antibiótica, vacunaciones y educación sanitaria, tras la implantación del programa de cribado neonatal universal de anaemia falciforme en la Comunidad de Madrid.
Pacientes y métodosSe realizó un estudio transversal observacional con recogida de información retrospectiva de una cohorte de niños con enfermedad falciforme diagnosticados por la prueba de cribado neonatal en la Comunidad de Madrid.
ResultadosSe obtuvieron datos de una muestra de 20 pacientes. El 95% de ellos fueron diagnosticados por la prueba de cribado neonatal realizado entre los 5 y 13 días de vida. La edad media de los pacientes cuando se realizó el estudio fue de 39 meses. En el seguimiento de estos pacientes desde Atención Primaria, se objetivó un cumplimiento de la profilaxis antibiótica del 90% y una cobertura del calendario vacunal oficial del 85%. La cobertura de vacunas específicas: 85% neumococo 23V, 50% gripe y 15% hepatitis A. El reconocimiento de haber recibido educación sanitaria solo alcanzó a una de cada 4 familias.
ConclusionesEn el seguimiento de los pacientes con anemia falciforme en Atención Primaria, se objetivó un aceptable cumplimiento de la profilaxis antibiótica, pero unas bajas coberturas tanto de las inmunizaciones sistemáticas como de las inmunizaciones específicas. La cobertura de educación sanitaria fue muy baja.
Para mejorar estos parámetros, sería necesaria una mayor coordinación e implicación de los profesionales de Atención Primaria con el fin de que estos pacientes tengan un seguimiento adecuado y que ello se traduzca en una disminución de las complicaciones de esta enfermedad y una mejoría en la calidad de vida.
Sickle cell disease (SCD) comprises a group of chronic inherited anaemias characterised by haemolysis and intermittent episodes of vascular occlusion leading to high morbidity and with a highly variable clinical expression.1
Early diagnosis allows for the combined followup by hospital paediatric haematology units and primary care (PC) from the first months of life. The various professionals involved are responsible for providing information about the disease and health education, initiating antibiotic prophylaxis, and ensuring compliance with the official routine and specific immunisation schedules.2–5
The aim of these measures is to improve quality of life significantly, reducing the number of complications and increasing the life expectancy of affected patients, as mortality due to SCD in the early years of life can reach up to 10% in the more developed countries.4
The most common presentation of SCD is the HbSS homozygous form, which affects approximately 75% of these patients. It manifests with severe haemolytic anaemia, vaso-occlusive bone pain crises, susceptibility to severe infections and severe end-organ damage, especially in the first 3 years of life. Other, less prevalent presentations are HbSC (25%), sickle thalassaemia (less than 1%) and sickle cell—other haemoglobinopathies, with a highly variable clinical expression, but usually milder.5,6
Clinicians in Spain are facing the challenge of treating SCD more often due to the increase in immigration, especially from African countries, Central and South America, and Asia, that has occurred in every autonomous community.5,6
In May of 2003, the autonomous community of Madrid (ACM) added a universal neonatal screening programme for the early detection of haemoglobinopathies to the already established screening tests.5 The incidence of the disease since the programme started has been 1 in 5851, and the carrier incidence 1 in 412.1,4 These patients are referred to their respective reference hospitals and PC teams to prevent and treat the complications of the disease.5
The main goal of our study was to assess, from PC, the compliance with the recommendations of the Sociedad Española de Hematología y Oncología Pediátricas (Spanish Society of Haematology and Oncology [SEHOP])6 in the ACM: to determine the degree of compliance with infection prophylaxis, the official immunisation schedule coverage (which at the time of the study included the 13-valent pneumococcal conjugate vaccine and the varicella vaccine), of the specific risk-group immunisation schedule (23-valent pneumococcal, influenza, and hepatitis A vaccines) and the health education received by these families. The secondary objectives were to determine the clinical course of the disease from birth, the number of visits to the PC paediatrician, the reasons for seeking care, the chronic diseases patients had, and the compliance with treatment.
Patients and methodsWe performed a retrospective cross-sectional observational study, gathering information on a cohort of newborns in the ACM diagnosed with SCD though the neonatal screening from May 2003 to October 2007. The study was authorised by the corresponding clinical research ethics board.
The followup protocol for these patients, as specified by the clinical guideline of the SEHOP,6 includes a series of steps that we are about to describe. Once the haemoglobin phenotype has been identified in the reference laboratory of the ACM, the family is notified and appointments are scheduled with the various providers of the paediatric haematology unit. During the first visit, the patient is given detailed information about the disease, the family history is taken, and a complete physical examination is performed. The importance of adhering to prophylactic treatment with penicillin and of complying with the official routine and specific immunisation schedules is emphasised. Laboratory tests and other supplemental studies are ordered as specified in the protocol and a clinical report is produced. The nursing staff provides health education to the family. The staff contacts the reference PC centre that the family is assigned to based on their home address and regular appointments are scheduled, both with the reference hospital and the PC team.
Our study consisted in studying the PC followup, gathering data for various variables (demographic, anthropometric, haematological diagnosis, associated disease, compliance with the SEHOP protocol…) and conducting an interview with the paediatrician of the health care centre assigned to the family based on their home between February 2008 and June 2009. The parents signed the informed consent form before the patients were included in the study.
We excluded as lost to followup any patients lost after the diagnosis for whom it was not possible to schedule the first visit with the hospital followup unit, and patients that could not be reached for followup in PC.
ResultsWe obtained data from 20 patients of 67 patients born with SCD in the ACM between May 2003 and October 2007. Of these 20 patients, 45% were male and 55% female. Seventeen had been born at term, 2 preterm, and one post-term. Ninety percent of the newborns had an appropriate weight for their gestational age, and 10% had a higher-than-normal weight. The mean age at the time the study started was 39 months, with the ages ranging from 16 to 69 months.
Of all parents, 85% were from Africa (40% from Nigeria, 35% from Equatorial Guinea, 5% from the Republic of the Congo, and 5% from Zaire). The remaining 15% were from the Dominican Republic. Five families lived in the city of Madrid, eight in the eastern ACM, and seven in the southern ACM.
The specific diagnosis was homozygous HbSS sickle cell anaemia in 85% of patients, HbSC in 10%, and HbCC in 5%. The diagnosis was made between days 5 and 13 post birth in 95%, and the mean was 8.7 days. In one patient born very preterm, the diagnosis was not confirmed definitively until nine months post birth due to multiple pathology in the neonatal period and the various blood components received. Of the 20 patients, 13 had one or more siblings. Twenty-five percent of these families already had one child with a SCD diagnosis.
When it came to scheduled interventions, 90% of patients had participated in the well-child programme of their health centre, and 85% were in compliance with the routine immunisation schedule. When it came to the specific at-risk schedule, only 50% had received the influenza vaccine, 85% had not been vaccinated against hepatitis A, and 15% were also missing the 13-valent pneumococcal conjugate vaccine, even though they were older than 2 years. Ninety percent of the patients were receiving infection prophylaxis with daily doses of penicillin. Only 5 out of the 20 families had attended health education talks on the management of this disease.
As for the medication used, 14 patients received chronic treatment, with folic acid being the most frequently used drug (55%), followed by hydroxyurea (15%). Five percent received other drugs (budesonide, montelukast and cephalosporins), as half the patients had some comorbidity associated to the underlying disease. Two patients needed transfusions. No patients required opioids for pain management.
The collected information regarding attendance of our patients to the healthcare centre and the emergency department (by their own initiative) was highly variable and not very reliable. Half of our patients were followed up at one single healthcare centre by the same paediatrician since their births.
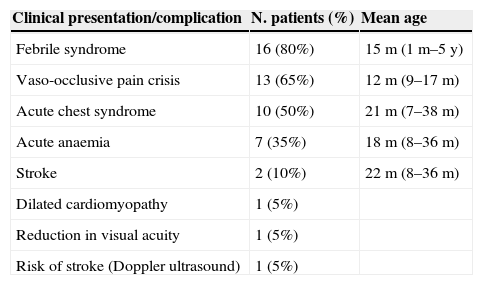
The most frequent reasons for seeking care documented in the medical records of the healthcare centre were febrile syndrome and vaso-occlusive pain crises (Table 1). Eighty percent of patients had some sort of fever, with the number of episodes per patient ranging from 1 to 14, and the mean age at which they happened was 15 months. Sixty-five percent developed vaso-occlusive pain crises, with a mean of two episodes per patient and dactylitis as the main form of presentation in infants. Half the patients developed acute chest syndrome (ACS), with a minimum of 1 episode and a maximum of 5. Seven patients had episodes of acute anaemia due to aplastic or haemolytic crises, of which 70% had a single episode and the other 30% two. Two siblings had strokes, one at 8 months and the other at 3 years of age, and required monthly red blood cell transfusions. As a consequence of the organic effects of the disease and its complications, one patient had dilated cardiomyopathy and another reduced visual acuity in the left eye. Transcranial Doppler ultrasound showed that a patient was at risk of stroke. As for childhood diseases, 2 patients had chickenpox (there was no record of having received the varicella vaccine despite it being appropriate for their ages), 4 bronchiolitis, and 3 pyelonephritis. One instance of a disorder rare in childhood involved a patient of Sub-Saharan descent that presented with pica.
Reasons for visit.
| Clinical presentation/complication | N. patients (%) | Mean age |
|---|---|---|
| Febrile syndrome | 16 (80%) | 15m (1m–5y) |
| Vaso-occlusive pain crisis | 13 (65%) | 12m (9–17m) |
| Acute chest syndrome | 10 (50%) | 21m (7–38m) |
| Acute anaemia | 7 (35%) | 18m (8–36m) |
| Stroke | 2 (10%) | 22m (8–36m) |
| Dilated cardiomyopathy | 1 (5%) | |
| Reduction in visual acuity | 1 (5%) | |
| Risk of stroke (Doppler ultrasound) | 1 (5%) |
Numerous studies have shown that early detection of SCD by neonatal screening tests leads to reduced morbidity and mortality as affected newborns are included in specialised and multidisciplinary followup programmes. Working in collaboration with primary care services can ensure treatment with antibiotic prophylaxis, compliance with specific immunisation schedules, and that the family is educated about the disease.7,8
There is less agreement on whether it is necessary to perform universal screenings, as recommended in the United States since 1987, where there is a high prevalence of SCD, as opposed to screening only risk groups, as advocated by other groups in Europe, where the prevalence is lower.2,4,9–16 The highest risk corresponds to individuals of Sub-Saharan, Latin American and East Indian descent.2,17 In Spain, SCD is an emerging health problem in recent decades due to the increase in immigration. In the ACM, neonates are routinely screened for SCD since May 2003 because a previous pilot study showed high prevalences of SCD and carrier status.1–4
We have analysed the followup of some of these patients in PC, as there are no studies conducted in Spain that address this subject in the medical literature.
Almost all patients were diagnosed through neonatal screening within 13 days post birth, and the HbSS phenotype was the most frequent presentation, consistent with the SEHOP guidelines.6
The loss to followup of patients diagnosed during neonatal screening for whom we could not obtain PC data may be due to various factors. On one hand there was a small number of patients born in our country that were diagnosed with SCD but never had a first visit in the hospital follow-up unit. The reason for this could be a return to the country of origin or relocation to a different autonomous community. We found that many patients were lost to PC followup due to frequent changes of address, with the subsequent switches in assigned healthcare centres and a possible loss of part of their medical records. We must keep in mind that it is hard to identify these patients, as many have very complicated first and last names and a different spelling by a single letter could potentially prevent the correct identification of the patient and lead to the duplication of PC medical records. Other patients spent long periods of time without making appointments (between 2 and 3 years) for which the reason was not documented in their records, with the exception of some who travelled to their countries of origin. Only half of our patients remained in a single healthcare centre and were served by the same paediatrician from birth, and these are the patients for which we obtained the most reliable information on the natural course of SCD. Lastly, we believe that the severity of the diagnosis and social factors may contribute to these families only attending medical visits at the hospital.
Most of our patients’ parents were of African origin. The 2008 and 2009 data of the Instituto Nacional de Estadística (National Institute of Statistics) shows that 17% of the documented foreign population in Spain came from Africa.
During their first visit to their assigned healthcare centre, these patients bring a clinical report and an introductory letter written by the hospital referral unit informing the paediatrician of the importance of complying with daily antibiotic prophylaxis (at least in the first five years of life) and of being up to date with the official ACM immunisation schedule, which needs to be supplemented with the influenza, hepatitis A, and 13-valent and 23-valent pneumococcal vaccines.7,17
Ninety percent of our cohort had attended their routine health check-up appointments, but only 85% were up to date with the official routine immunisation schedule in the years we were collecting data, a time when the nationwide coverage rate for the primary vaccination series ranged between 95.6% and 98.5%.18 This is a disappointment, as is the fact that even though the patients had reports stating the need to have additional vaccines not included in the routine immunisation schedule, many of them were not in compliance. This is particularly serious in the case of vaccination against pneumococcus, as pneumococcal infection is the main cause of mortality in the first years of life because the risk of bacteraemia by Streptococcus pneumoniae is 400 times greater in patients with SCD, as described in the literature.7 This situation may be worse now, as the 13-valent pneumococcal conjugate vaccine has been withdrawn from the ACM routine immunisation schedule since 2012.
Likewise, the degree of compliance with penicillin prophylaxis ought to be monitored closely, as the risk of infection by encapsulated bacteria is higher due to splenic hypofunction. Pneumococcal vaccines and antibiotic prophylaxis reduce the incidence of pneumococcal sepsis by 84% in children younger than 5 years.7 Fortunately, the rate of compliance with penicillin prophylaxis in our patients, while leaving room for improvement, is of 90%, lowering the risk of severe infection.
Vaccination against influenza aims at preventing this disease and its potential complications, such as secondary bacterial infections. Vaccination against hepatitis A is particularly important in these patients considering their parents’ countries of origin due to the risk of contracting the disease in potential visits to these countries. We observed that 2 patients in our cohort had varicella even though they were of an age—3 and 5 years, respectively—in which previous vaccination would have been appropriate; one of them had severe varicella and developed ACS as a complication. For all of the above, PC paediatricians and nurses ought to monitor the vaccination status of these patients, taking advantage of any on-demand, routine or emergency visits for any health reasons to check compliance with the vaccination schedule and catch up as needed. Furthermore, non-attendance to routine visits should raise concern and lead to an investigation of the patient's clinical state by the paediatric staff of the healthcare centre.
There was a wide variation in the number of on-demand and emergency visits the patients made to the healthcare centre as well as in the number of visits to hospital emergency departments. There was a high rate of hospital admissions, both for patients referred by their paediatricians and for patients that went to the hospital of their own accord (80% and 70%, respectively).
The most common complications observed in the followup of our patients during infancy were dactylitis and fever; and ACS and stroke were the most frequent reasons for hospital admission, consistent with the literature.7,8
The absence of patients with chronic analgesic treatment could be due to our cohort consisting of young patients, but another possible reason may be that patients with severe disease treated with multiple analgesic drugs and opioids habitually seek services at the hospital and do not go to their healthcare centres.
A strategy should be formulated to increase existing knowledge of the disease in susceptible populations. In the ACM, each new individual diagnosed with the disease or as a carrier is sent an informational trifold brochure by post the contents of which are later explained in person, both at the hospital and in the PC office. The nursing staff is in charge of health education, individually at the PC office and in workshops carried out at hospitals for parents of patients of different ages. They are instructed, among other things, on how to recognise pain crises, palpate the spleen, manage fever and use analgesics. This also provides a space for parents to share their views and experiences of the disease. However, attendance to these meetings is low, possibly due to long distances between the home and the hospital. For this reason, the PC doctor and nurse can offer a closer connection to the families, improving the goals of health education. Improving the health education of these patients and their families would achieve reductions in the number of visits to healthcare centres and emergency departments and in the number of hospitalisations,19–22 ultimately improving quality of life.
ConclusionsThere is extensive loss to followup of children with SCD by PC teams that is probably due to social factors and difficulties in integrating the immigrant population in the healthcare system. While our country has gained experience in the management of this disease in the past decade due to an increasing number of cases, efforts must be made to adhere to the consensus recommendations of the scientific community. Complete vaccination of these patients has improved significantly, especially considering the current circumstances, with vaccination against pneumococcal disease excluded from the routine schedule. The coordination of primary care and hospital services must be fluid to guarantee an adequate health education, so meetings between professionals in both fields should be promoted.
FundingThe study was funded by the Dr. Prandi grant for research in paediatrics.
Conflict of interestThe authors have no conflicts of interest to declare.
We want to thank Esperanza Escortell, a health technician at the SERMAS, for her collaboration.
Please cite this article as: Rodríguez-Moldes B, Carbajo AJ, Sánchez B, Fernández M, Garí M, Fernández MC, et al. Seguimiento en Atención Primaria de los recién nacidos con enfermedad falciforme detectados en el cribado neonatal de la Comunidad de Madrid. An Pediatr (Barc). 2015;82:222–227.