We present the case of a patient aged 14 years assessed in the emergency department for colicky pain in the right flank radiating toward the hypogastrium. The urinalysis was normal, and since the presentation was compatible with renal colic, an abdomen radiograph was performed (Fig. 1).
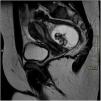
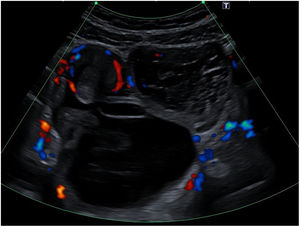
The evaluation continued with an abdominal ultrasound scan (Fig. 2) that evidenced a lesion measuring 73 × 70 × 58 mm, compatible with teratoma, although the organ of origin could not be determined. The patient also underwent a magnetic resonance imaging (MRI) scan of the abdomen (Fig. 3).
Ovarian tumours are rare in children, amounting to 1% to 5% of total paediatric tumours. Up to 90% of paediatric ovarian tumours are germ cell tumours, and the most frequent type is mature cystic teratoma (55%–70% of ovarian tumours in paediatrics).1,2 Ovarian mature cystic teratomas are benign tumours that can develop at any age, but the incidence peaks in the second and third decades of life. They arise from at least 2 of the 3 germ layers, and the contents are most frequently of ectodermal origin (hair, fat, teeth, skin…).2 Most patients are asymptomatic at diagnosis, with detection of the teratoma as a chance finding, but patients may develop abdominal pain, a palpable mass, complications such as ovarian torsion or rupture and even paraneoplastic syndromes, although the latter is very rare. Up to 10% of paediatric cases are bilateral.3 The initial diagnosis is made by abdominal ultrasound, in which the most common appearance is a cystic lesion with posterior shadowing (Rokitansky nodule). The evaluation is usually completed with an MRI scan to measure the mass more accurately and determine its relationship with adjacent structures.2 Approximately 50% have calcifications and up to 22% contain teeth detectable by imaging.4 Therefore, the detection of features with calcification density or shaped like a tooth in an abdominal X-ray may be key in the diagnosis of teratoma.
The management of ovarian teratoma is surgical, and the prognosis excellent. Authors increasingly advocate for conservative approaches ensuring full resection of the teratoma with fertility preservation, as it is not uncommon for metachronous tumours to develop at a later stage requiring additional surgeries, with an incidence that varies between the published series ranging from 5.7% to 23%.5