Home apnea monitors detect abnormalities in cardiac and respiratory frequency, but their use in the diagnosis of respiratory-related sleep disturbances in children has not been demonstrated, as was originally thought.
ObjectiveTo describe the type of patients being monitored, for how long and their outcome.
Material and methodsA retrospective descriptive study was conducted on patients with controlled home cardiorespiratory monitoring from October 2008 to September 2012 in the Outpatient department of a Maternity tertiary hospital.
ResultsDuring the study period 88 patients were included, 58% of them were male, with a median age of 15.5 days, and followed up for a period of 4.7 months. The reason for monitoring was due to a history of sudden death without finding underlying pathology in 20.5%, 25% due to apnea of prematurity, 20.5% due to apparent life-threatening event, and 14.8% due to choking. Other causes accounted for 19.3% (apnea/hypopnea, desaturation and periodic breathing). Of these last three groups, pathological events were observed in 50% of them: reflux disease (9), apnea of prematurity (2), neurological causes (3), and apnea of unknown cause (10).
ConclusionsSuspected infant apnea is a cause for consultation that creates a great deal of concern to the family and the paediatrician. Home monitoring is useful in detecting changes in cardiac and respiratory frequency, but is necessary to limit its indications and ensure proper monitoring of these patients, avoiding the abuse of other tests or treatments.
Los monitores de apneas detectan anomalías en la frecuencia cardíaca y respiratoria, sin utilidad demostrada para el diagnóstico de alteraciones respiratorias relacionadas con el sueño en los niños como se pensaba en su origen.
ObjetivoDescribir el tipo de pacientes que se monitorizan, durante cuánto tiempo y la evolución de los mismos.
Materiales y métodosEstudio descriptivo retrospectivo de los pacientes con monitorización cardiorrespiratoria domiciliaria controlados, desde octubre del 2008 hasta septiembre del 2012, en consultas externas de un hospital materno-infantil de tercer nivel.
ResultadosDurante el periodo de estudio fueron incluidos 88 pacientes, el 58% de ellos de sexo masculino, con una mediana de edad de 15,5 días y durante un periodo de 4,7 meses. El motivo de monitorización fue en un 20,5% por antecedente de muerte súbita, sin encontrar patología subyacente; un 25% por apnea de la prematuridad; un 20,5% por episodio aparentemente letal, y un 14.8% por atragantamiento. Otras causas suponen el 19,3% (apnea/hipopnea, desaturaciones y respiración periódica). De estos 3 últimos grupos, en el 50% se registraron eventos patológicos: reflujo patológico (9), apneas de la prematuridad (2), causa neurológica (3) y apneas de causa desconocida (10).
ConclusionesLa sospecha de apnea del lactante es un motivo de consulta que crea gran preocupación tanto a la familia como al pediatra. La monitorización domiciliaria es útil en la detección de alteraciones en la frecuencia cardíaca y respiratoria pero es necesario limitar sus indicaciones y realizar un buen seguimiento de estos pacientes, evitando el abuso de otras pruebas complementarias o tratamientos.
Apnoea monitors are devices designed to detect changes in heart rate and breathing effort associated with apnoea, and not to diagnose respiratory abnormalities associated with sleep in children.1
Home apnoea monitors started to be used over thirty years ago, when it was hypothesised that prolonged apnoea may be the cause of sudden infant death syndrome (SIDS). They were designed to try to prevent death in infants by detecting episodes of central apnoea or bradycardia and alerting the parents so they could intervene before the event turned fatal.
Subsequently, several studies have concluded that apnoea is not associated with SIDS and that the use of monitors will not prevent sudden death.2
The fear of sudden infant death leads parents and clinicians to monitor at-risk infants for their protection, with the regrettable consequence that this provides a false sense of security when in fact monitoring devices are designed to detect a limited range of events.
In our hospital, we started following up the use of apnoea monitors since 1997, at first in the context of preventing sudden death, and later including other indications for monitoring.
The aim of our study was to describe the type of patients that are monitored, for how long, and the outcomes of these patients.
Materials and methodsWe conducted a retrospective descriptive study of patients subject to home cardiorespiratory monitoring followed up between October 2008 and September 2012 at the outpatient clinic of a tertiary children's and maternity hospital.
We selected the patients by the retrospective review of the electronic or paper medical records of all patients with an initial presenting complaint or a final diagnosis related to apnoea. From this set, we selected the patients with home apnoea monitors that were followed up in the outpatient clinic, and we collected data for epidemiological, clinical and management variables.
Definitions3Apnoea: unexplained episode of cessation of airflow lasting 20s or longer, or of shorter duration if accompanied by bradycardia, cyanosis, pallor or severe hypotonia.
Periodic breathing: breathing pattern with pauses lasting between 3 and 20s alternating with periods of normal breathing.
Apparent life-threatening event (ALTE): acute event that is frightening to the observer consisting of some combination of apnoea of 20s of duration or longer, change in colour, and change in muscle tone, and requiring vigorous stimulation or resuscitation.
SIDS: sudden death that is unexplained by history and for which the post-mortem examination fails to demonstrate the cause of death.
The patients that were monitored due to apnoea of prematurity were those referred from the neonatal unit, and the patients included in the study for a history of ALTE were those with documented pathological events detected by monitoring during the observation period in the inpatient ward.
We entered and processed the collected data in a Microsoft Access relational database (Microsoft Corporation, Redmond, United States).
We performed the statistical analysis with the SPSS 20.0 software (SPSS Inc., Chicago, United States). Most variables were dichotomous and nominal, and were expressed as percentages, absolute frequencies, means with their standard deviations (SD) and medians with their interquartile range (IQR).
We compared qualitative variables between groups by means of contingency tables, using the chi square test. We compared quantitative variables with the parametric Student's t test for independent samples.
ResultsThe duration of followup in our study was 47 months, from October 2008 through September 2012. We included a total of 88 patients, 57.9% of whom were male, with a median age of 15.5 days at the start of monitoring (IQR, 2–54.2 days), and a median duration of monitoring of 4.7 months (IQR, 2.4–8.1 months).
The indication for monitoring was a family history of sudden death in 20.5% of the patients, a previous ALTE in 20.5%, apnoea of prematurity in 25.0%, and choking in 14.8%. Other reasons accounted for the monitoring of 19.2% of the patients (apnoea/hypopnoea, episodes of oxygen desaturation, and periodic breathing).
We have described the results for each of the three follow-up groups: apnoea of prematurity, history of sudden death and ALTE, the latter of which included choking and other reasons for monitoring.
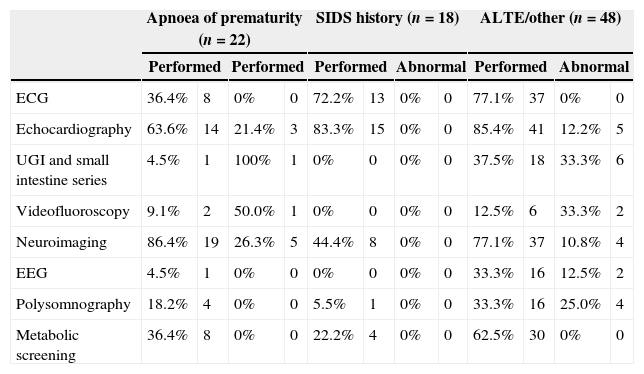
In the 22 patients of the apnoea of prematurity follow-up group that had been referred by the neonatology unit (25.0%), the mean and standard deviation of the duration of monitoring were 5.6±3.1 months. Nineteen (86.4%) of these patients were treated with caffeine for a mean of 2.6±1.2 months due to recordings compatible with apnoea of prematurity and/or immature breathing. Among them, 68.2% were born at gestational ages ranging from 32.0 to 36+6 weeks, 18.2% at 28.0 to 31+6 weeks of gestational age (GA) and another 13.6% at less than 28 weeks of GA.
Eighteen patients (50.0% of whom were male) were followed up due to a family history of sudden death for a median of 8.1 months (IQR, 3.5–11 months). Additional tests were performed in these patients: cardiovascular assessment in 15 children (83.3%), neuroimaging studies in 8 (44.4%) and metabolic screening in 4 (22.2%). The tests did not detect disease in any of the patients, although in one of them they detected episodes of apnoea accompanied by bradycardia that resolved spontaneously. One of the patients died of an accidental pulmonary aspiration four months after monitoring was discontinued.
In the third group of patients (n=48) that included ALTE, choking and other reasons for monitoring, a cardiovascular assessment was performed in 85.4% of the patients, and five had abnormal results (3 cases of foramen ovale, 1 of inferior vena cava agenesis, and 1 of ventricular septal defect). A Holter electrocardiogram (ECG) was performed in 5 patients, with normal results in all. An upper gastrointestinal (UGI) with small bowel series was performed in 37.5% of patients and was abnormal in six (33.3%). Videofluoroscopy was requested for 6 patients and was abnormal in 2. Neuroimaging tests were done in 37 patients (77.1%) with abnormal findings in 4 (arachnoid cyst in 1, signs of hypoxia due to severe hypoxic-ischaemic encephalopathy in 2, delayed myelination in 1). An electroencephalogram (EEG) was performed in 16 children (33.3%), with abnormal findings in two. Polysomnography was done in 16 patients and was abnormal in four. Metabolic screening was done in 62.5% of patients and was normal in all. In 50.0% (24) of the patients in this group, no new events were detected during monitoring. The final diagnosis of the patients in whom new events were detected were gastroesophageal reflux disease (GERD) in nine, apnoea of prematurity in two, a neurological condition in three, and apnoeas that were self-limited and of unknown cause in ten. While only two patients were diagnosed with apnoea of prematurity, eight were given caffeine for a suspected breathing disorder related to immaturity, and while GERD was detected in 9 patients, 12 received treatment.
Table 1 summarises all the diagnostic tests performed in each group along with their results.
Tests performed in the study by reason for followup.
| Apnoea of prematurity (n=22) | SIDS history (n=18) | ALTE/other (n=48) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Performed | Performed | Performed | Abnormal | Performed | Abnormal | |||||||
| ECG | 36.4% | 8 | 0% | 0 | 72.2% | 13 | 0% | 0 | 77.1% | 37 | 0% | 0 |
| Echocardiography | 63.6% | 14 | 21.4% | 3 | 83.3% | 15 | 0% | 0 | 85.4% | 41 | 12.2% | 5 |
| UGI and small intestine series | 4.5% | 1 | 100% | 1 | 0% | 0 | 0% | 0 | 37.5% | 18 | 33.3% | 6 |
| Videofluoroscopy | 9.1% | 2 | 50.0% | 1 | 0% | 0 | 0% | 0 | 12.5% | 6 | 33.3% | 2 |
| Neuroimaging | 86.4% | 19 | 26.3% | 5 | 44.4% | 8 | 0% | 0 | 77.1% | 37 | 10.8% | 4 |
| EEG | 4.5% | 1 | 0% | 0 | 0% | 0 | 0% | 0 | 33.3% | 16 | 12.5% | 2 |
| Polysomnography | 18.2% | 4 | 0% | 0 | 5.5% | 1 | 0% | 0 | 33.3% | 16 | 25.0% | 4 |
| Metabolic screening | 36.4% | 8 | 0% | 0 | 22.2% | 4 | 0% | 0 | 62.5% | 30 | 0% | 0 |
The results of the comparisons between groups were not statistically significant.
DiscussionPneumograms are useful in the detection of pathological events associated with changes in heart rate and breathing effort. However, after decades of home monitoring, the controversy surrounding their efficacy has led to recommendations for their use to be restricted to selected circumstances. They must be used with caution for ruling out other diseases or as a safety system for other events that occur in sleep.4
Home apnoea monitors started to be used over twenty-five years ago at a time when prolonged apnoea was proposed as the possible cause of sudden infant death syndrome (SIDS). The original intent of these monitors was to detect bradycardia or prolonged breathing pauses and to alert the parents in order to prevent fatal outcomes in children with known risk factors. Subsequently, several studies have concluded that prolonged apnoea is not associated with SIDS and that monitors cannot prevent sudden death.5,6 The factors with a demonstrated association with a higher risk of sudden death, on which there is consensus among health professionals worldwide and which can be prevented, are prone sleep and prenatal and postnatal maternal smoking.4,7
Epidemiologically, there has been no change in the incidence of SIDS in relation to the use of monitors in the past decades,6 but in clinical practice it is often still challenging for clinicians to determine when monitoring should be prescribed, for how long, and how to follow up these patients. The study by Hunt et al.8 proposed that subtle cardiorespiratory changes detectable by monitors may precede pathological events like extreme apnoeas or bradycardias by a few hours. However, the American Academy of Paediatrics and the Asociación Española de Pediatría4 recommend against using home monitoring for the prevention of SIDS, although they accept its potential usefulness for the quick detection of central apnoea in certain situations and in specific diseases.
The indications for cardiorespiratory monitoring in our hospital, which are similar to those applied in many other facilities and are to be considered according to some clinical guidelines,3 are essentially a history of sudden death in a sibling, apnoea of prematurity, or ALTE. We did not investigate other respiratory diseases that require assisted mechanical ventilation in our study. Thus, this case series assesses the diagnostic tests performed in children monitored for each of these reasons, including cardiovascular assessment, UGI and small bowel series, videofluoroscopy, EEG, neuroimaging and metabolic screening.
Among the children followed up for apnoea of prematurity in our series, most of those being monitored at home had gestational ages that ranged between 32 and 36+6 weeks. The 2001 review by Zhaoy et al.9 noted that the incidence of apnoea of prematurity is inversely proportional to gestational age, and that it affects almost all newborns younger than 29 weeks. This discrepancy may be due to the fact that in extremely preterm newborns, apnoea resolves before requiring followup, as apnoea of prematurity is a maturational and self-limiting problem, although we must also take into account that there is a smaller proportion of extremely preterm newborns. Their review also suggested that most cases resolve by week 36 to 40 of postconceptional age, in contrast with other studies that extend this period to 43 weeks of postconceptional age.2 However, the duration of monitoring in patients with a history of apnoea of prematurity was probably excessive in our study, as it was of 5.6 months.
In children followed up due to the previous death by SIDS of a sibling, the results of all the diagnostic tests were normal, with cardiovascular assessment being the most frequent investigation (83.3%). The median duration of followup was 8.1 months, which was probably related to the degree of anxiety experienced by the parents, and in some cases it lasted a few more months. Several reviews suggest that the risk of SIDS decreases after 6 months10 and after 9 months in severe cases, and it is recommended that monitoring is discontinued at least 2 months beyond the age of the previous infant death.3 The fact that only one pathological event was detected should make us reconsider this approach.
In the case review by Hally et al.,11 7% of the children that died of SIDS had a history of ALTE. While some mothers of children that died of SIDS reported a previous ALTE more frequently that mothers of control children, those cases constituted a small proportion of the total cases of SIDS. In our study, none of the children that were followed up experienced a new event, and none of them died.
There is published evidence on risk factors for ALTE that are identified in the anamnesis and physical examination and that would make a patient a candidate for home apnoea monitoring.12 The known risk factors include preterm birth, multiple previous ALTEs and suspected child abuse. The yield of diagnostic tests for ALTE as defined in 19873 is questionable, and an aetiological investigation should be performed before prescribing the use of an apnoea monitor to rule out diseases that are treatable and may have caused the event.3 At present, there is no well-defined protocol for the management of infants that experience ALTEs, and more powerful studies are needed to establish it. As Weiss et al. suggest in their prospective 2010 study,13 the yield of diagnostic tests following an ALTE is low overall, and it only increases when there is a high degree of suspicion. Screening tests for gastroesophageal reflux, meningitis, bacteraemia or seizures are low yield in infants without historical risk factors or suggestive physical examination findings.12 In our case series, EEG was performed in 33.3% of patients in the ALTE group, and it was only abnormal in two. The study we just mentioned reported a 4.5% yield for this test, in contrast with other studies that support the inclusion of EEG as a first-line test in cases of ALTE based on the fact that 11% of these patients are eventually diagnosed with seizures.14 In our series, abnormal tracings were found in 4.2% of the ALTE patients, although some of these patients had additional signs and symptoms that suggested the presence of an underlying disease.
Another example is the cardiovascular assessment. There is evidence that highlights the role of ECG as a potentially useful tool in the diagnosis of ALTE caused by changes in heart rate.15 In our study, we found that ECG had been performed in 85.4% of patients that had experienced ALTEs, and the results of 12.2% of the tests had been abnormal. However, the echocardiogram findings did not explain the clinical features of the ALTE.
As for neuroimaging as the gold standard for testing, the study by Weiss et al.13 mentioned above advocated for reserving these methods for cases in which there is a strong clinical suspicion of neurological causes. In our case series, it was performed in 77.1% of the patients, and it was abnormal in four cases in which there was at least one concurrent abnormal finding, so its use for screening could be considered on a case-by-case basis.
On the other hand, metabolic screening is included in the basic investigation of ALTEs in many studies.14 In our series, it was performed in 62.5% of patients in the ALTE group and 22.2% of patients in the SIDS history group, and it was negative in all cases. While there are references that advocate for performing the screening because it is an innocuous and affordable test,10,14,16 its routine implementation is questionable based on the results of our study.
Most of the diagnostic tests performed in our study were negative, and the few that had abnormal results usually did not suffice to determine the cause of apnoea. Thus, the most suitable approach may be to perform specific diagnostic tests based on the individual clinical context, as opposed to establishing a series of tests to be performed in all of these patients.
The limitations of our study are its retrospective design, with the disadvantages that it carries, and that the sample consisted of children monitored at home, leaving out all cases of children that had an ALTE that was evaluated and did not require subsequent monitoring.
In conclusion, suspected apnoea in infants is a presenting complaint that elicits great concern both in the family and the paediatrician, and the indication of apnoea monitoring is a subject of controversy. We know that it is useful in the detection of changes in heart rate and breathing effort, but its use must be restricted to selected circumstances and there must be an adequate followup of the patients, as there is a tendency to overuse it. The indication of monitoring in subsequent siblings of SIDS victims should be reviewed, the known risk factors established for ALTE should be evaluated, and limits should be set for the duration of its use in patients with apnoea of prematurity. It is also important to avoid the abuse of additional diagnostic tests and unnecessary treatments, and that further research of a greater scope be conducted to study the indications for testing, the duration of treatment and monitoring, and the followup of patients with risk factors.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Martínez Monseny A, Bobillo Pérez S, Martínez Planas A, García García JJ. Papel de las exploraciones complementarias y de la monitorización domiciliaria en los pacientes de riesgo de episodio aparentemente letal, apneas y síndrome de muerte súbita del lactante. An Pediatr (Barc). 2015;83:104–108.