Invasive meningococcal disease (IMD) remains a serious public health problem. Although culture is the gold standard, previous antibiotic therapy reduces its sensibility. The aim of this study is the epidemiological analysis of IMD in our area, to assess the usefulness of polymerase chain reaction (PCR) to increase its diagnostic accuracy, and to show the association of antibiotic administration with the negative result of the culture.
Patients and methodsA retrospective study was conducted on all children younger than 16 years with microbiologically (positive culture and/or PCR) confirmed IMD, admitted to our hospital between 2004 and 2012.
ResultsSeventy-five patients were included, of whom 52% had sepsis, 30.7% meningitis, and 17.3% with both. PCR showed positive results in all samples, whereas a positive result was seen in 50.7% of the cultures. Previously administered antibiotic was documented in 40 patients (53.3%), and 40% of them were confirmed by PCR only.
ConclusionsPCR was the only test providing evidence for IMD diagnosis and serogroup determination in almost 39% of cases.
La enfermedad meningocócica invasiva (EMI) constituye un grave problema de salud pública. A pesar de que el cultivo es la técnica de referencia para su diagnóstico, la administración previa de antibiótico altera su sensibilidad. Los objetivos de este estudio son el análisis epidemiológico de la EMI en nuestro medio, evaluar la utilidad de la reacción en cadena de la polimerasa (PCR) para incrementar el diagnóstico de confirmación de la EMI y valorar la asociación de la administración de antibiótico con el resultado negativo del cultivo.
Pacientes y métodosEstudio retrospectivo de los pacientes menores de 16 años diagnosticados de EMI mediante cultivo, PCR o ambos, que ingresaron en nuestro centro en el periodo 2004–2012.
ResultadosSe incluyó a 75 pacientes, de los cuales el 52% presentó sepsis, el 30,7% meningitis y el 17,3% sepsis con meningitis. La PCR fue positiva en todas las muestras de sangre y líquido cefalorraquídeo analizadas, mientras que el cultivo tuvo una positividad muy inferior (50,7%). Recibieron antibiótico antes de la extracción de las muestras 40 pacientes (53,3%) y el 40% de ellos fueron confirmados por la PCR.
ConclusionesGracias a la PCR se obtuvo un diagnóstico de confirmación de EMI en el 38,7% de los casos y del serogrupo, hecho relevante para la vigilancia epidemiológica y el estudio de la efectividad vacunal.
Invasive meningococcal disease (IMD) constitutes a serious public health problem worldwide, with a high impact on society and a high rate of morbidity and mortality in all age groups. Despite advances in our knowledge of the disease and its diagnosis and treatment, and the implementation of new preventive strategies, IMD is endemic in many countries, even developed ones, with attack rates of between 1 and 5 cases per 100,000 inhabitants.1
In Spain, according to data from the national system of epidemiological surveillance (Sistema Nacional de Vigilancia Epidemiológica [SNVE]) from 2004 to 2011, the overall incidence rate for IMD was of 0.92–1.67 cases per 100,000 inhabitants.2–4 The highest incidence in children occurs in those younger than 1 year, with a rate of 13 cases per 100,000 in the 2009–2010 season.3 Serogroups B and C caused over 90% of the IMD cases in Spain.2,3,5 The introduction of the conjugate meningococcal C vaccine in 2001 has reduced the incidence of IMD caused by this serotype by up to 88%,6 but it is still a serious disease due to its sequelae (11–19%)2,3 and mortality rate (5–14%).1–3
The diagnosis of IMD is confirmed by ascertaining the presence of Neisseria meningitidis (N. meningitidis) in the blood or in the cerebrospinal fluid (CSF), or in both, either by culture or by detection of bacterial deoxyribonucleic acid (DNA),5,7 or the two methods. Culture continues to be the gold standard for microbiological diagnosis, and it also allows for antimicrobial sensitivity and strain identification testing of the isolate. Still, it does have limitations, chief among which is its low diagnostic yield when the samples are taken from patients who have received previous antibiotic treatment.5,8–11
Even if the culture is performed, there is a sizable percentage of reported IMD cases without a microbiological diagnosis, and this limits the analysis of its epidemiological evolution and the impact of vaccination.
The introduction of DNA detection techniques that use polymerase chain reaction (PCR) represents an advance in confirmatory diagnosis, and various studies and clinical practise guidelines recommend routine PCR testing.5,8,12–14
The aim of this study was to make an epidemiological analysis of IMD in our country, assess the usefulness of PCR in the diagnosis of IMD, and study the correlation of negative cultures in confirmed cases with previous antibiotic therapy.
Patients and methodsWe performed a retrospective study of the medical records of patients younger than 16 years with a clinical diagnosis of IMD confirmed by culture, PCR, or both, admitted to the Hospital Universitari Vall d’Hebron between January 2004 and December 2012. All the cases were selected based on culture and PCR results from the microbiology department.
We collected data on demographic, clinical, and laboratory variables, and also documented whether the patient had received antibiotic therapy prior to sample collection.
Samples of blood, CSF or both were collected for culture and PCR (both techniques were performed on a single sample), and were processed and analysed in the molecular diagnosis, blood culture, and general culture laboratories of the microbiology department. PCR testing was done on samples larger than 100μL. Nucleic acids were extracted from the samples with the EasyMag® automated platform (bioMèrieux, Marcy-l’Étoile, France) and later amplified by multiplex PCR for N. meningitidis (ctrA region, capsular transport gene), Haemophilus influenzae type b (bexA, capsulation gene) and Streptococcus pneumoniae (ply, pneumolysin gene) with TaqMan® fluorescent probes in a Smartcycler® thermal cycler (Cepheid, Sunnyvale, USA).15N. meningitidis was serotyped by agglutination with specific antisera in cases for which the strain was available; and otherwise by PCR following the method described by Mölling et al.16 Blood cultures were done in paediatric FAN bottles using the BacT/ALERT®3D system (Biomèrieux, Marcy l’Etoile, France). Samples for CSF cultures were centrifuged at 1500rpm for 15min and the sediment was inoculated in blood agar plates and LAN enriched medium.
We performed a descriptive analysis of the sample to identify extreme or erroneous values, and then expressed discrete variables as frequencies and proportions, and continuous variables as means (or medians) and their corresponding standard deviations (or interquartile ranges). We used the chi-square test to assess the statistical significance of the association between the administration of antibiotics prior to sample collection and negative culture results. The level of statistical significance was set at P<0.05. The statistical analysis was done with the software SPSS® version 20.0 (SPSS, Chicago, USA).
The study was approved by the ethics committee of the hospital.
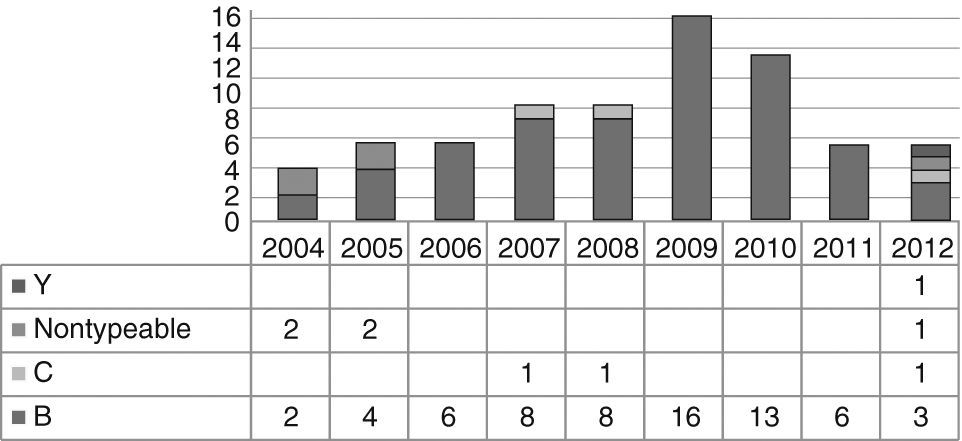
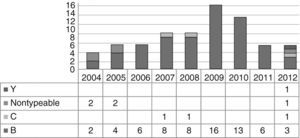
ResultsBetween January 2004 and December 2012, our hospital admitted 75 patients with a clinical diagnosis of IMD confirmed by culture, PCR or both. The case distribution remained homogeneous during the 9 years of the study, save for an increased incidence in 2009 and 2010 (29/75, 38.7%) (Fig. 1). Table 1 summarises the most pertinent demographic and clinical data of the patients.
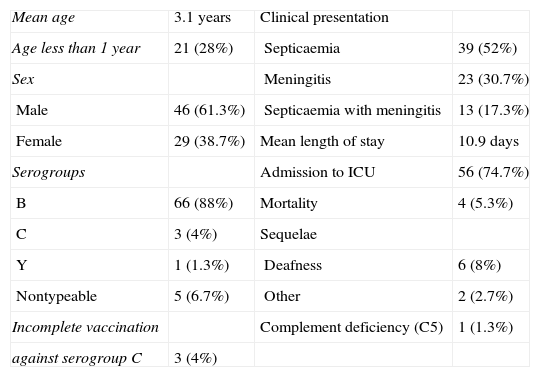
Demographic and clinical characteristics of the 75 patients with invasive meningococcal disease.
| Mean age | 3.1 years | Clinical presentation | |
| Age less than 1 year | 21 (28%) | Septicaemia | 39 (52%) |
| Sex | Meningitis | 23 (30.7%) | |
| Male | 46 (61.3%) | Septicaemia with meningitis | 13 (17.3%) |
| Female | 29 (38.7%) | Mean length of stay | 10.9 days |
| Serogroups | Admission to ICU | 56 (74.7%) | |
| B | 66 (88%) | Mortality | 4 (5.3%) |
| C | 3 (4%) | Sequelae | |
| Y | 1 (1.3%) | Deafness | 6 (8%) |
| Nontypeable | 5 (6.7%) | Other | 2 (2.7%) |
| Incomplete vaccination | Complement deficiency (C5) | 1 (1.3%) | |
| against serogroup C | 3 (4%) |
C5, complement component 5; ICU, intensive care unit.
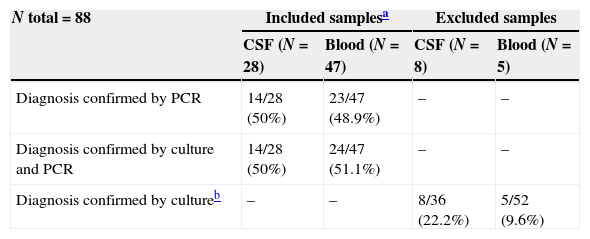
The microbiological data are presented in Table 2. In 8 of the 36 patients with a clinical diagnosis of IMD (23 had meningitis and 13 septicaemia with meningitis), the diagnosis was confirmed by culture alone, as molecular testing was not performed. In the remaining 28 it was possible to do CSF cultures and PCR. The PCR assay was positive in 100% of the cases, and the culture in 50%, that is, half of the cases (14 patients) were diagnosed by means of PCR.
Microbiological characteristics of the 75 patients with invasive meningococcal disease.
| N total=88 | Included samplesa | Excluded samples | ||
|---|---|---|---|---|
| CSF (N=28) | Blood (N=47) | CSF (N=8) | Blood (N=5) | |
| Diagnosis confirmed by PCR | 14/28 (50%) | 23/47 (48.9%) | – | – |
| Diagnosis confirmed by culture and PCR | 14/28 (50%) | 24/47 (51.1%) | – | – |
| Diagnosis confirmed by cultureb | – | – | 8/36 (22.2%) | 5/52 (9.6%) |
CSF, cerebrospinal fluid; N, number of samples; PCR, polymerase chain reaction.
In 5 of the 52 patients diagnosed with septicaemia (39 with septicaemia and 13 with septicaemia with meningitis), the diagnosis was confirmed by culture alone, as molecular testing was not performed. In the remaining 47 patients it was possible to perform both culture and PCR assays. The PCR results were positive in 100% of the cases and the culture was positive in 51.1% of cases, that is, 48.9% of the cases (23 patients) were diagnosed by PCR.
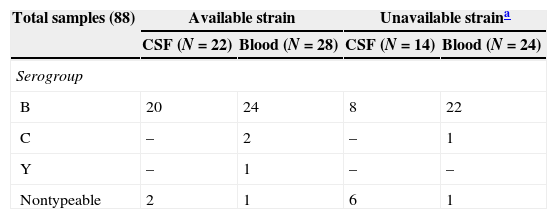
The meningococcal serogroup could be determined in 88.6% of the samples (78/88). PCR successfully serotyped 81.6% (31/38) of the samples: 95.8% of peripheral blood samples (22 serogroup B and 1 serogroup C) and 57.1% of CSF samples (8 serogroup B) (Table 3).
Serogroup distribution of CSF and peripheral blood samples.
| Total samples (88) | Available strain | Unavailable straina | ||
|---|---|---|---|---|
| CSF (N=22) | Blood (N=28) | CSF (N=14) | Blood (N=24) | |
| Serogroup | ||||
| B | 20 | 24 | 8 | 22 |
| C | – | 2 | – | 1 |
| Y | – | 1 | – | – |
| Nontypeable | 2 | 1 | 6 | 1 |
CSF: cerebrospinal fluid.
One or more doses of antibiotics had been given to 53.3% of the patients (40/75) before sample collection, and 40% (16) of these patients could only be diagnosed by PCR. In our study, the association between the administration of antibiotics prior to sample collection and negative culture results did not reach statistical significance (P=0.53).
DiscussionInvasive meningococcal disease has clinical forms of varying severity, such as septicaemia and meningitis. It can progress quickly, and patients with a fulminant course may develop purpura, disseminated intravascular coagulation, shock and coma, often in spite of early and appropriate diagnosis and management.1,5
The clinical and microbiological results obtained in our series are consistent with the literature, with the IMD incidence peaking in infants younger than 1 year, the highest prevalence corresponding to serogroup B, and considerable associated sequelae and mortality rates.2–4
The development of molecular techniques has advanced the microbiological diagnosis of IMD. These methods are increasingly used in reference hospitals and offer several advantages compared to culture: they are more sensitive, specific and quick, and its detection ability is not affected by the previous administration of antibiotics5,8,10–12; yet they also have drawbacks, such as their high cost and the need for qualified personnel to perform them.5,8,13 The latest data published in the European Invasive Bacterial Diseases Surveillance Network17 report for season 2008–2009 show that while culture continues to be the gold standard for diagnosing IMD (47.9% in 2008 and 44.7% in 2009), the percentage of cases confirmed only by PCR is 25%, and even higher in countries such as Greece (42.7%), United Kingdom (51.6%) and Ireland (58.3%). Also, the Spanish Ministry of Health recently published a clinical practise guideline for the management of IMD that recommends routine PCR testing for diagnosis, even if culture continues to be the gold standard.5,13 After reviewing the literature, the authors of the guideline reported that the increase of IMD cases with a diagnosis confirmed by PCR ranges between 30% and 40%.5 The introduction of multiplex PCR in our setting has allowed the diagnosis of 38.7% of the cases of IMD that could not have been confirmed otherwise, a percentage similar to those found in other studies.5,13 Furthermore, PCR has allowed the identification of the serogroup of 81.6% of samples for which the strain of N. meningitidis was not available, an important fact when it comes to epidemiologic surveillance and research on vaccine effectiveness.
Several studies have assessed the sensitivity of PCR compared to culture.5,9,10,12,13 The guidelines of the National Institute for Health and Care Excellence of the United Kingdom13 include 4 studies on PCR that support its routine performance. Their results show that PCR has a sensitivity of 87–88%, while the sensitivity of culture ranges between 17% and 58%. Another study included in the clinical practise guideline of the Spanish Ministry of Health5 assessed the use of PCR in CSF samples for the confirmatory diagnosis of IMD, and found a sensitivity of 92% for PCR and of 64% for culture.
In our study, in patients for whom we could compare the results of both diagnostic tests, PCR was positive in 100% of the analysed samples, while the culture had a much lower positive rate (50.7%), which confirms the greater sensitivity of PCR compared to the gold standard. We ought to note that our study was not designed to calculate the sensitivity or predictive value of these two microbiological methods, and that this study could not analyse the results of some samples due to the reduced amount collected.
Another important limitation of our study is that the sample selection was based on IMD cases with a confirmed microbiological diagnosis, and did not include suspected cases.
The association between negative culture results and the administration of antibiotics prior to sample collection is well known.5,8,10–13 Although it did not reach statistical significance in our study, this was probably due to the small sample size.
The introduction of microbiological molecular techniques has advanced the diagnosis of IMD, leading to a considerable increase in the number of confirmed cases. Despite its high sensitivity and other advantages mentioned above, PCR cannot replace culture as the gold standard. It is recommended that both tests be performed simultaneously because both offer considerable benefits, such as serogroup determination and a greater sensitivity due to a reduction in false negatives; furthermore, serotyping and the assessment of antibiotic resistance can only be undertaken in strains isolated in the culture.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Fernández-San José C, Moraga-Llop FA, Codina G, Soler-Palacín P, Espiau M, Figueras C. La reacción en cadena de la polimerasa en el diagnóstico de la enfermedad meningocócica invasiva. An Pediatr (Barc). 2015;82:139–143.